The novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which causes the disease COVID-19, has caused a pandemic that has rapidly affected the whole world and caused a significant threat to public health. The aim of this study was to investigate and analyze the social and occupational effects of the COVID-19 pandemic on patients with multiple sclerosis (MS) in three different countries: China, Spain, and Cuba.
MethodsA cross-sectional survey was designed to assess the social and occupational effects of the COVID-19 pandemic in MS patients in these three countries, using a 25-item anonymous online questionnaire, structured into three sections. Quantitative data are expressed as mean (standard deviation), and quantitative data as absolute frequency and percentage.
ResultsA total of 361 participants responded to the questionnaire: 194 from China, 104 from Spain, and 63 from Cuba. We found no cases of COVID-19 among Chinese patients with MS, and few cases in Spain and Cuba. Respondents reported different levels of impact on relationships with friends, family, and colleagues, and patients in all three countries described increased use of digital or social media platforms. Spanish patients reported a significantly less negative impact than those in Cuba and China. Mental and cognitive effects were similar in all three countries, although China seemed to have a better situation. We also found that the time spent exercising decreased at specific points during the pandemic, but with few changes in dietary habits. Patients reported little or no change in their means of transport in all three countries. Most patients in all three countries reported little or no physical deterioration, especially in Chinese patients (82.47%), compared to the Spanish (70.20%) and Cuban respondents (73.02%). In general, patients from all three countries demonstrated confidence in overcoming the COVID-19 pandemic, although to a lesser extent among Spanish respondents.
ConclusionsDuring the pandemic, family support was more effective in China than in Cuba and Spain. Neither COVID-19 infections nor the number of MS relapses increased significantly during lockdown in any of the three countries. Regarding their economic situation, Spanish MS patients reported a significantly less severe negative impact than those in Cuba and China. Patients from all three countries used digital or social media platforms more frequently, probably to maintain personal relationships. Chinese and Cuban respondents were more confident of the control of the pandemic than the Spanish, who were more pessimistic.
El nuevo coronavirus de tipo 2, causante del síndrome respiratorio agudo severo o COVID-19, se ha expandido rápidamente a nivel mundial, convirtiéndose en una grave amenaza para la salud pública en forma de pandemia. El objetivo de este estudio es analizar los efectos sociolaborales de la pandemia de COVID-19 en pacientes con esclerosis múltiple (EM) en 3 países diferentes (China, España y Cuba).
MétodosDiseñamos un estudio transversal para valorar los efectos sociolaborales de la pandemia de COVID-19 en pacientes con EM procedentes de China, España y Cuba mediante un cuestionario digital de 25 preguntas divididas en 3 apartados. Los datos cuantitativos se expresan como medias y desviaciones estándar, mientras que los datos cualitativos se expresan mediante valores y porcentajes.
ResultadosUn total de 361 pacientes respondieron al cuestionario (194 de China, 104 de España y 63 de Cuba). No encontramos ningún paciente chino con EM que hubiera padecido COVID-19, y los casos diagnosticados en España y Cuba fueron muy infrecuentes. A raíz de la pandemia, se observaron cambios en las relaciones con amigos, familiares y compañeros; además, los pacientes con EM usaron plataformas digitales y redes sociales con más frecuencia en los 3 países. El impacto negativo fue significativamente menor en España que en Cuba o China. Los efectos mentales y cognitivos de la pandemia fueron similares en los 3 países, aunque parece que la situación previa era mejor en China. Igualmente, observamos que el tiempo dedicado al ejercicio se redujo en momentos específicos durante la pandemia. Por el contrario, no se detectaron grandes cambios en los hábitos alimentarios. Los pacientes de los 3 países consideraron que no se produjeron cambios en su medio de transporte, o que estos fueron escasos. La mayoría de los pacientes ha experimentado poco o ningún deterioro físico, particularmente los pacientes chinos (82,47%) en comparación con los españoles (70,20%) y cubanos (73,02%). En líneas generales, todos los pacientes se mostraron esperanzados en superar la pandemia, aunque los pacientes españoles en menor grado.
ConclusionesDurante la pandemia, el apoyo familiar fue más importante en China que en Cuba o España. En ninguno de los 3 países se observó un aumento significativo en el número de casos de COVID-19 ni de brotes o recaídas durante el periodo de confinamiento. En términos económicos, los pacientes con EM españoles sufrieron un impacto negativo significativamente menor que los cubanos y chinos. Todos los pacientes usaron plataformas digitales o redes sociales con más frecuencia, probablemente con el fin de mantener relaciones personales. Los pacientes chinos y cubanos mostraron mayor confianza en el control de la pandemia que los españoles, que resultaron ser más pesimistas.
The new severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), also called COVID-19, named by The World Health Organization (WHO),1 has caused a pandemic that has rapidly affected the whole world and has caused a great threat to public health. The report showed more than 49.7 million cases of Covid-19 and more than 1.2 million deaths worldwide on November 10, 2020.2 The presence of COVID-19 is manifested by a variety of symptoms, ranging from no symptoms or mild symptoms to severe illness and death. Common symptoms include cough, fever, and breathlessness. Other reported symptoms are weakness, malaise, muscle pain, sore throat, loss of taste and/or smell.3
The first case of endemic pneumonia of unknown cause first broke out in Wuhan City, Hubei Province, China, in December 2019. As the outbreak coincided with the arrival of the Lunar New Year, interprovincial travel facilitated its spread. Within a month, it had spread massively to the 34 provinces of China.4 According to data from the National Health Commission of China, the total number of cases continued to rise sharply in early February, with an average of more than 3000 new confirmed cases per day. To control COVID-19, China has implemented unprecedented strict public health measures. On January 23, Wuhan City was lockdown via blocked connecting roads of the city to restrict travel. Subsequently, the Chinese government has adopted suitable prevention measures for all provinces, such as family confinement, the extension of national fairs, the closure of schools throughout the country, the banning of meetings, the closure of public facilities, and the closure city total to control the COVID-19 outbreak.5 These measures, mainly homed confinement, limited human mobility, and decreased new cases' appearance in a notable and sustained manner.6 It proved such restrictions harmed people's daily lives. Wuhan lifted quarantines on April 8, and so far, China has not yet relaxed its control measures. Except for isolated cases caused by infections from frozen products originating from other countries,7 all imported cases are from abroad. In the past six months, China's economic life and education have gradually recovered. However, despite China's control of the outbreak, the international spread of COVID-19 has accelerated since late February, with a growing number of countries reporting large numbers of infected.
The global COVID-19 pandemic has forced many countries to take containment measures to minimize the virus's spread, which has occurred in Spain. The Spanish government announced that it had entered a state of alarm on March 15, 2020, and then adopted a series of mandatory measures to restrict free movement. The first COVID-19 alert status ended on June 21, 2020.8 These measures are useful since they substantially reduced infections, which allowed starting a de-escalation phase towards the usual daily routine. However, in late September, there appeared to be a second outbreak across Europe. On October 9, 2020, the Spanish government announced that it had once again entered a state of alarm to establish the necessary measures to deal with the extraordinary risks caused by the uncontrolled spread caused by SARS-CoV-2. The second state of alarm for COVID-19 ended on October 24, 2020.8,9
A period of confinement or quarantine implies a radical change in the population's lifestyle, disrupting normal daily activities.10 Changes in Spanish adults (alcohol, tobacco, sleep time, and the consumption of fruits and vegetables) progressively decreased during COVID-19 confinement. The only habit that increased was alcohol consumption and the time of exposure to the TV screen and computers.11 However, the experience of a long period of confinement may have had a significant impact on those who have suffered the strictest restrictions on free movement and other potential consequences such as patients with Multiple Sclerosis (MS).
On March 11, 2020, Cuba reported the first confirmed cases of COVID-19 case, and on April 7, the stage of limited autochthonous transmission was declared.12 The Ministry of Public Health (MINSAP) developed a plan of activities to limit this disease's information and at the proper control of cases.13 On March 24, the country reported 40 new measures on different sectors to confront COVID-19. Due to the accumulated experiences in the fight against different epidemics, the Cuban National Health System (SNS) is well prepared to face this epidemiological challenge.14 With the appropriate measures that the government has taken and the population's efforts, Cuba achieved success against COVID-19 in three months. On June 18, the criteria for post-COVID-19 recovery in its three phases began to be gradually applied, except the Matanzas and Havana provinces.12,15 Subsequently, given the epidemiological complex in Havana, it decided to take new restrictive measures to reinforce physical isolation in the capital as of September 1. A month later, it indicated that the country would enter into force the new stages as the new normal, and this measure started on October 12.
MS is a chronic autoimmune disease of the central nervous system in which inflammation, demyelination, and axonal loss occur even in the early stages of the disease.16 Some research proved the connection between other types of coronavirus and demyelinating diseases. However, few studies reported the association between SARS-CoV-2 and the deterioration of MS.17 The proportion of MS patients studied with a risk of death from COVID-19 is less than 1%, in particular, the vast majority do not receive any treatment with DMT.18 COVID-19 has spread rapidly worldwide, significantly affecting people's lives, the social economy, and health systems. During the initial phase of the COVID-19 outbreak in China, more than half of those surveyed rated the psychological impact as moderate to severe. About a third reported mild to severe anxiety.19
The prevalence and incidence of MS vary widely between different countries and different geographic areas. Kurtzke proposed in 1980 to divide the different areas of the world into three geographical regions concerning the prevalence of MS: High>30/100,000, Medium 5–25/100,000, and Low risk <5/100,000.20 The prevalence of China,20 Cuba,21 and Spain22 are 3–5, 10–15, and 80–180 per 100,000 inhabitants, respectively. Therefore, we conducted these investigations to analyze the socio-occupational effects of the COVID-19 pandemic in patients with MS in three different countries: China, Spain, and Cuba. At the same time, to study the pandemic's impact on patients with MS in various stages.
Materials and methodsEnvironment and participantsWe adopted a cross-sectional survey design to assess the socio-occupational effects of the COVID-19 pandemic in relapsing–remitting MS (RRMS) patients in three different countries: China, Spain, and Cuba, using an anonymous online questionnaire. Participants came from various MS research centers in the three countries. The participants from China, Spain, and Cuba came from the Northwestern University Medical College, the Department of Research and Treatment of MS of the DINAC Foundation, and the Department of Neurology of the Hospital Hermanos Ameijeiras in the province of Havana, respectively.
ProcedureWe surveyed from October 10 to 24, 2020, through private institutions and social networks; for example, the public platform WeChat (China), the official website of the DINAC Foundation (Spain), and WhatsApp (Cuba) completed the questionnaire in Chinese and Spanish. The study fully complied with national and international regulations and the Declaration of Helsinki (2000). Informed consent was designed into the introduction of the questionnaire to fully inform the research requirements and accepted the privacy and data exchange policy. The first question of the questionnaire allows patients to freely choose whether they were willing to participate in the study or not, if they agreed, they would continue with the questionnaire, if they refused, they would exit. Minors were required to complete under parental supervision. The anonymous nature of online investigations did not allow the tracking of sensitive personal data in any way.
Design of the questionnaireThe questionnaire was designed by Zhang Guoxun, Zhao Runze, Zhang Wenting and others, with the Dinac Foundation's support. It consists of 3 parts and 25 questions. Part 1: Demographic characteristics of the patient (for example, age, sex, educational level, marital status, and residence region). Part 2: Effects of COVID-19 in MS patients (you have been infecting with COVID-19, some of your family, friends and colleagues have infected with COVID-19, you have had difficulty seeing your doctor, you have had a relapse/outbreak, you have had trouble getting your MS medicine). Part 3: Impact of COVID-19 in different situations (for example, a total of 14 questions related to study, work, transport, economy, and life). The full version of the questionnaire is available as an Annex.
Statistical analysisThe database was collected using Excel 2019 software and analyzed with the SPSS 25.0 program. Before analyzing the data, each variable displayed individually, eliminating possible transcription errors. We analyzed quantitative data by the mean ± standard deviation (x ± s). Besides, a number and percentage in parentheses (%) was also used in the questionnaire.
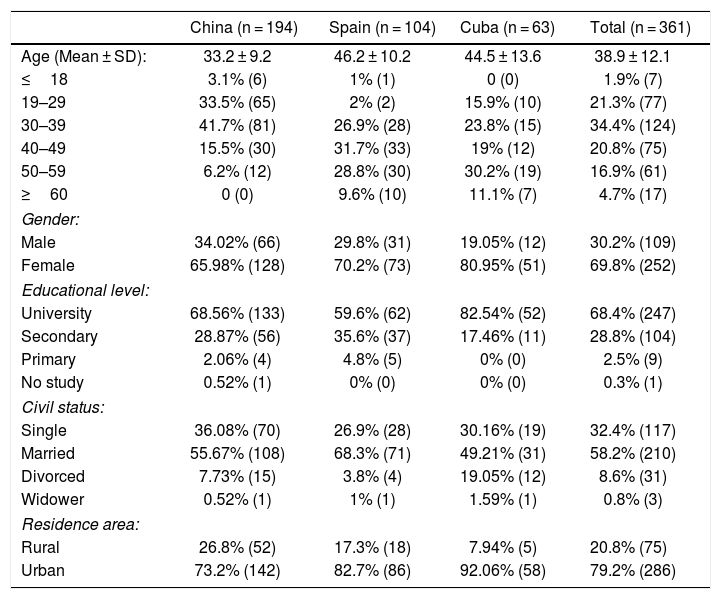
ResultsDemographic characteristicsThe demographic characteristics shown in Table 1. A total of 450 questionnaires were sent out for this study, including 230 from China, 90 from Cuba, and 130 from Spain, 361 participants answered the questionnaire. The male proportion was 30.2% (109) and the female ratio was 69.8% (252). In China, 194 patients participated in the questionnaire, of which 65.98% (128) were women and 34.02% (61) were men. In Spain, 104 patients participated, of which 70.2% (73) were women and 29.8% (31) were men. There were 63 patients from Cuba, of which 80.95% (51) were women and 19.05% (12) were men.
Demographic characteristics of study sample (n = 361).
| China (n = 194) | Spain (n = 104) | Cuba (n = 63) | Total (n = 361) | |
|---|---|---|---|---|
| Age (Mean ± SD): | 33.2 ± 9.2 | 46.2 ± 10.2 | 44.5 ± 13.6 | 38.9 ± 12.1 |
| ≤18 | 3.1% (6) | 1% (1) | 0 (0) | 1.9% (7) |
| 19–29 | 33.5% (65) | 2% (2) | 15.9% (10) | 21.3% (77) |
| 30–39 | 41.7% (81) | 26.9% (28) | 23.8% (15) | 34.4% (124) |
| 40–49 | 15.5% (30) | 31.7% (33) | 19% (12) | 20.8% (75) |
| 50–59 | 6.2% (12) | 28.8% (30) | 30.2% (19) | 16.9% (61) |
| ≥60 | 0 (0) | 9.6% (10) | 11.1% (7) | 4.7% (17) |
| Gender: | ||||
| Male | 34.02% (66) | 29.8% (31) | 19.05% (12) | 30.2% (109) |
| Female | 65.98% (128) | 70.2% (73) | 80.95% (51) | 69.8% (252) |
| Educational level: | ||||
| University | 68.56% (133) | 59.6% (62) | 82.54% (52) | 68.4% (247) |
| Secondary | 28.87% (56) | 35.6% (37) | 17.46% (11) | 28.8% (104) |
| Primary | 2.06% (4) | 4.8% (5) | 0% (0) | 2.5% (9) |
| No study | 0.52% (1) | 0% (0) | 0% (0) | 0.3% (1) |
| Civil status: | ||||
| Single | 36.08% (70) | 26.9% (28) | 30.16% (19) | 32.4% (117) |
| Married | 55.67% (108) | 68.3% (71) | 49.21% (31) | 58.2% (210) |
| Divorced | 7.73% (15) | 3.8% (4) | 19.05% (12) | 8.6% (31) |
| Widower | 0.52% (1) | 1% (1) | 1.59% (1) | 0.8% (3) |
| Residence area: | ||||
| Rural | 26.8% (52) | 17.3% (18) | 7.94% (5) | 20.8% (75) |
| Urban | 73.2% (142) | 82.7% (86) | 92.06% (58) | 79.2% (286) |
Note: n: number; SD: standard deviation.
Among the surveyed populations, whose found different age ranges between 13 and 75 years of age, the mean age was 38.9 ± 12.1. The mean ages of China, Spain, and Cuba were 33.2 ± 9.2, 46.2 ± 10.2, and 46.2 ± 10.2, respectively. In China, 3.1% (6) were less than or equal to 18 years old, 33.5% (65) were between 19 and 29 years old, 41.7% (81) were between 30 and 39 years old, 15.5% (30) were between 40 and 49 years old, 6.2% (12) were between 50 and 59 years old. In Spain, 1% (1) were less than or equal to 18 years old, 2% (2) were between 19 and 29 years old, 26.9% (28) were between 30 and 39 years old, 31.7% (33) were between 40 and 49 years old, 28.8% (30) were between 50 and 59 years old, 9.6% (10) were older than or equal to 60 years. In Cuba, 0% (0) were less than or equal to 18 years old, 15.9% (10) were between 19 and 29 years old, 23.8% (15) were between 30 and 39 years old, 19% (12) were between 40 and 49 years old, 30.2% (19) were between 50 and 59 years old, 11.1% (7) were equal to or more than 60 years old.
All the patients from the three countries participating in the questionnaire were 20.8% (75) of rural origin and 79.2% (286) urban. They had an educational level of secondary or university training, which represented approximately 97.2%. Their marital statuses were 32.4% (117) single, 58.2% (210) married, 8.6% (31) divorced, and 0.8% (3) widowed.
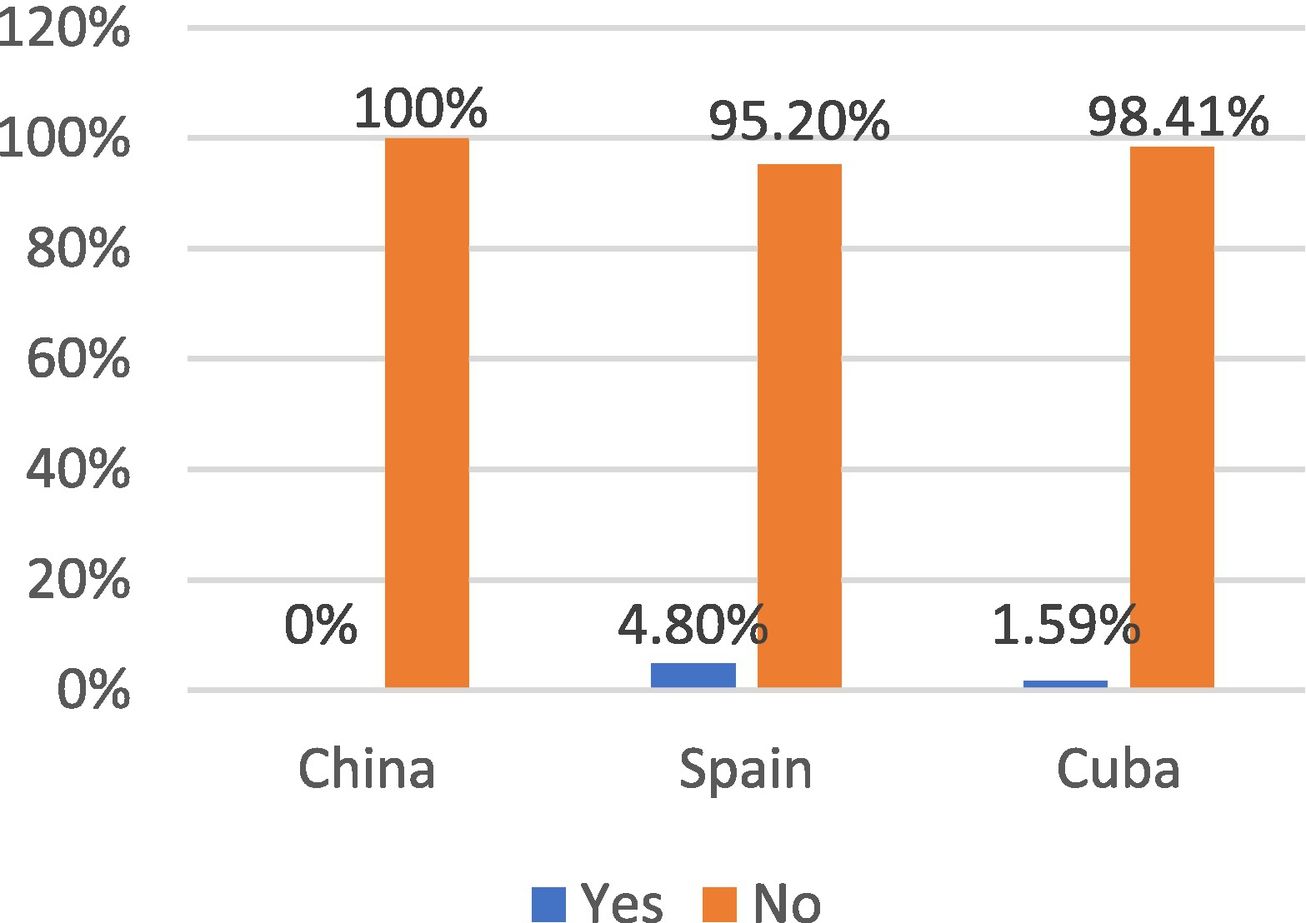
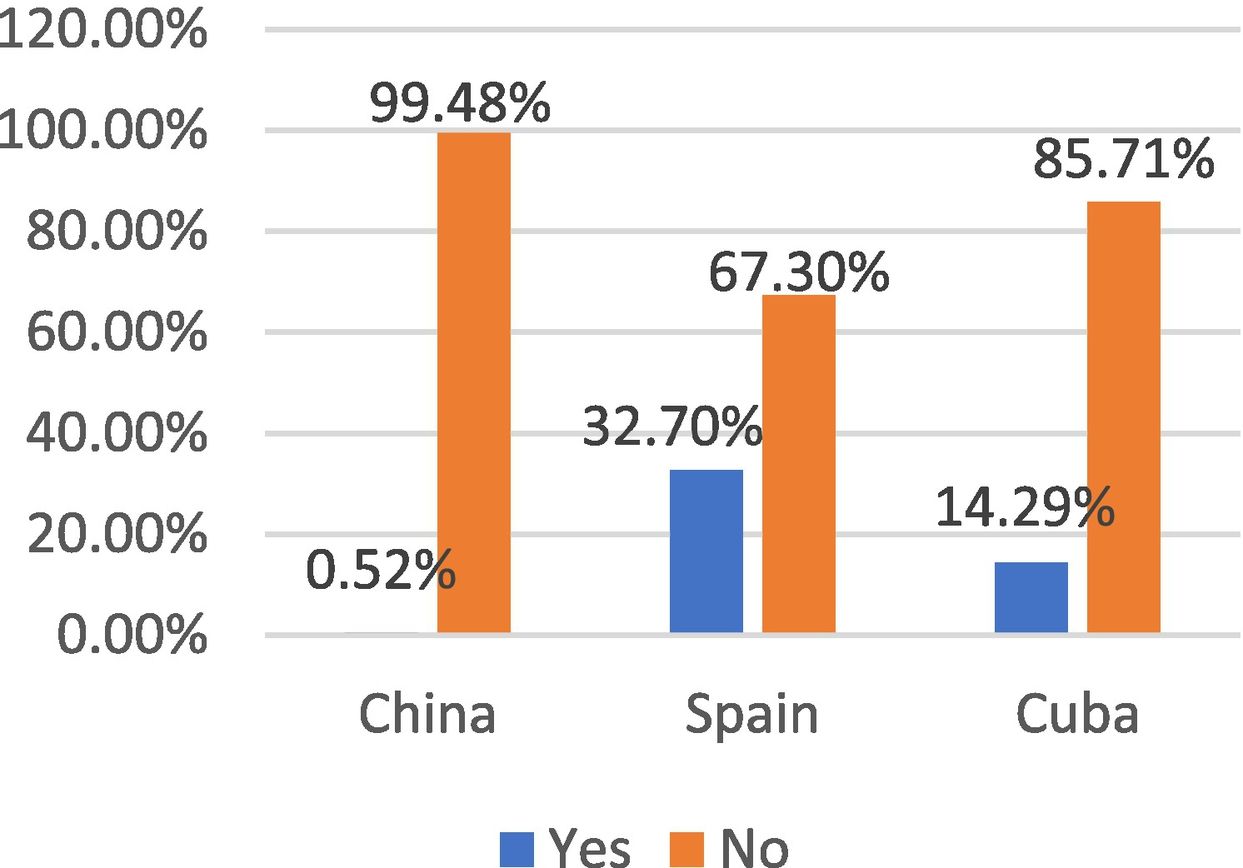
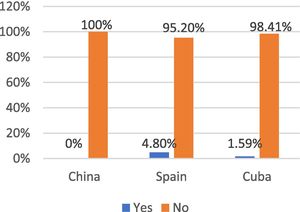
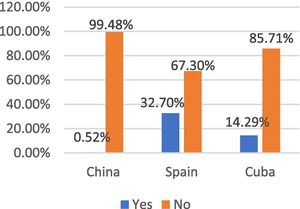
Effects of COVID-19 in MS patientsAccording to the data collected, during the COVID-19 pandemic, China did not find any MS patient who suffered from COVID-19 infection, Spain had 4.8% (5) patients, Cuba had 1.59% (1) patients (Fig. 1). In China, 0.52% (1), in Spain, 32.7% (34), and in Cuba, 14.2% (9) of patients with MS had relatives, friends, or colleagues infected with COVID-19 (Fig. 2).
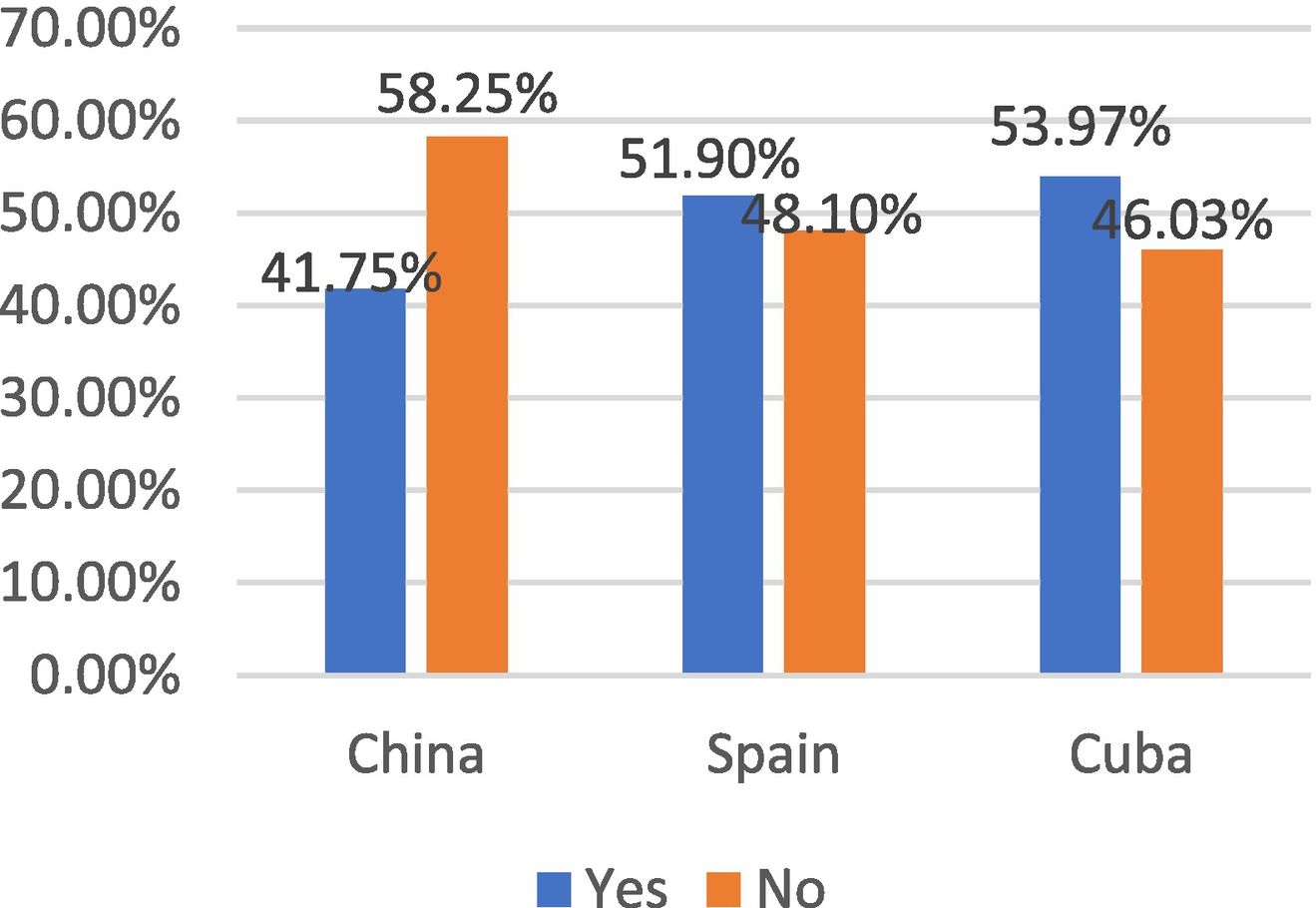
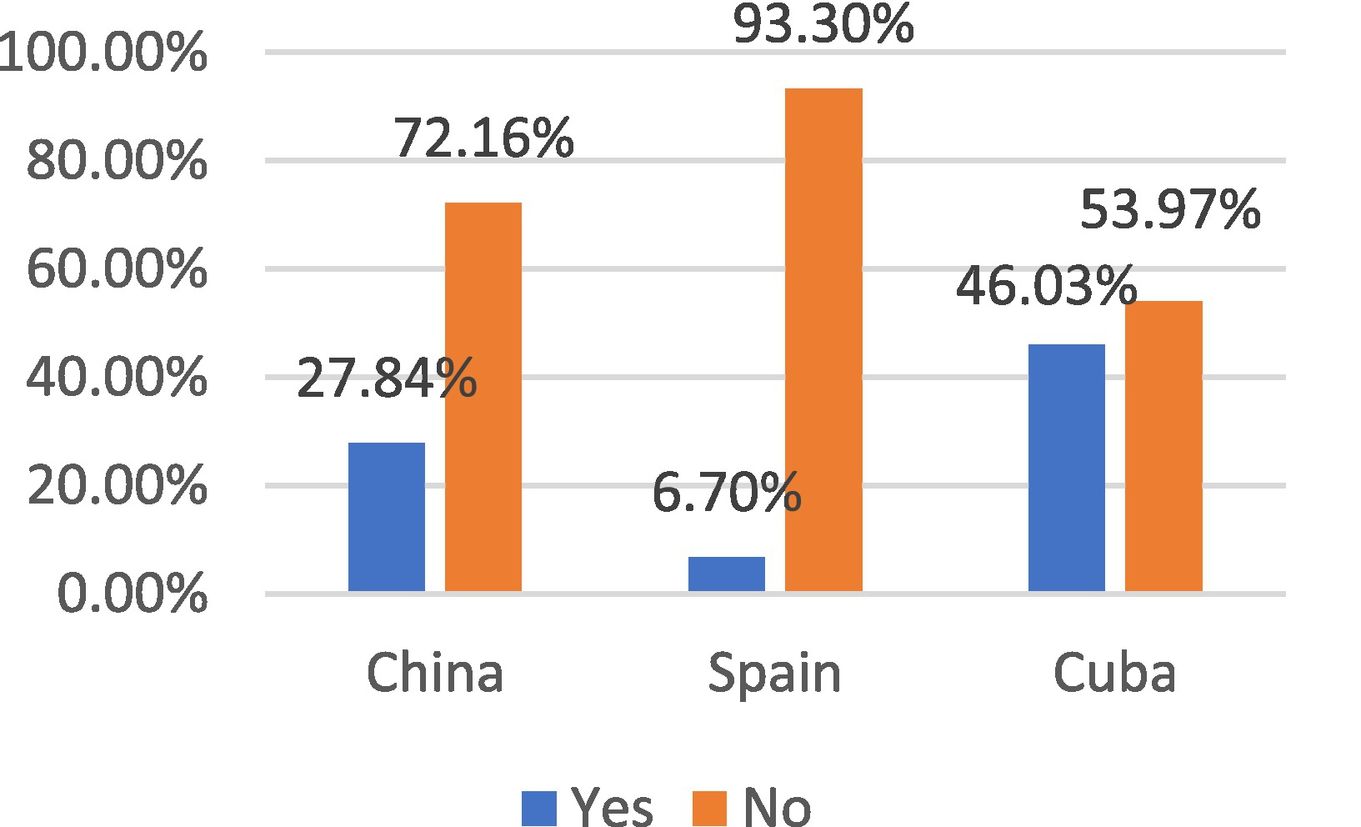
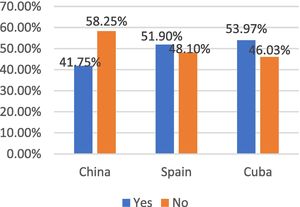
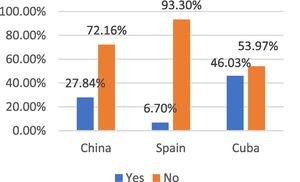
We have observed that around 58.25% Chinese patients with MS during the pandemic have had no difficulty seeing their doctor, a somewhat higher proportion than Spain (48.1% and Cuba (46.03%) (Fig. 3). But patients from Spain had easier to continue with drug treatment, the proportion reached 93.3%, higher than China (72.16%) and Cuba (53.97%) (Fig. 4).
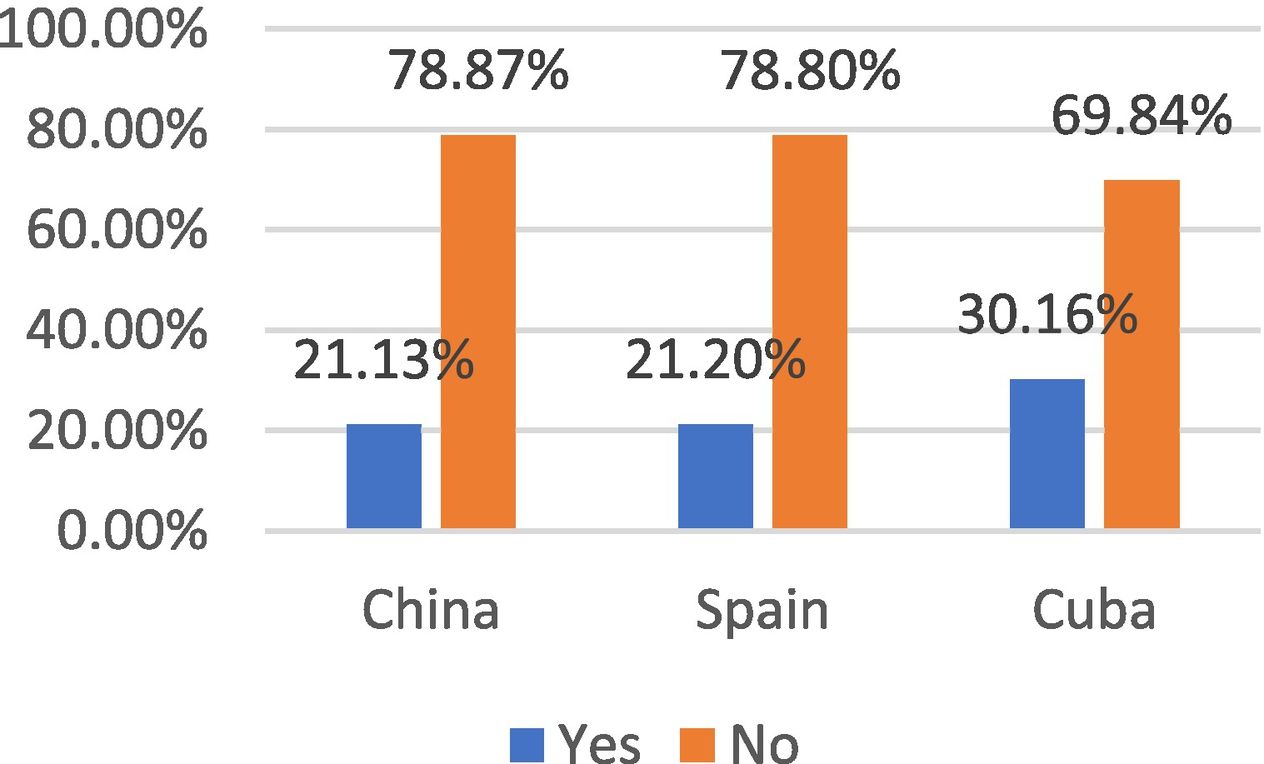
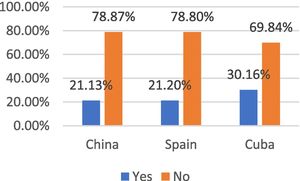
Furthermore, during the pandemic, the recurrence / outbreak rate in these three countries was low, 21.13% from China, 21.2% from Spain, and 30.16% from Cuba (Fig. 5).
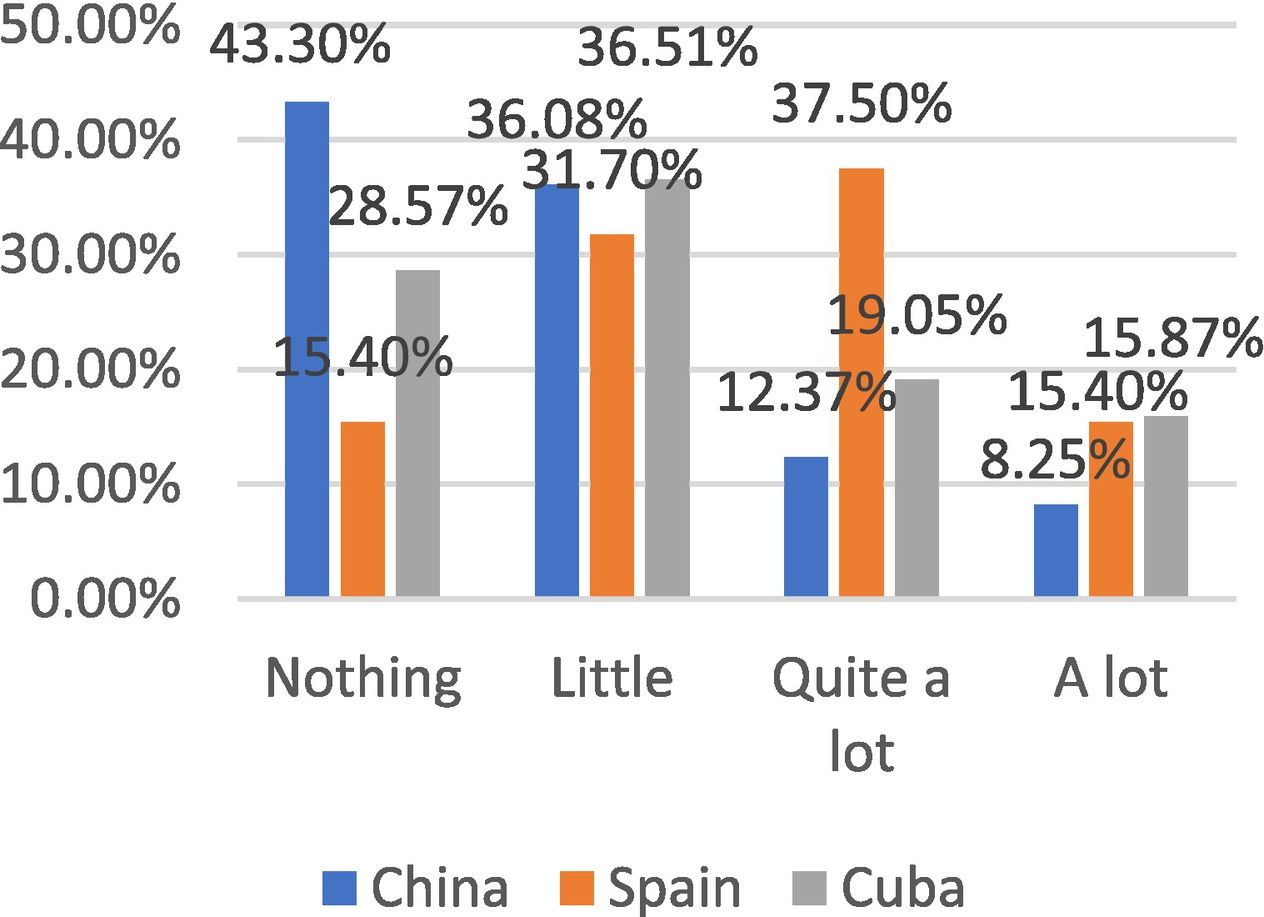
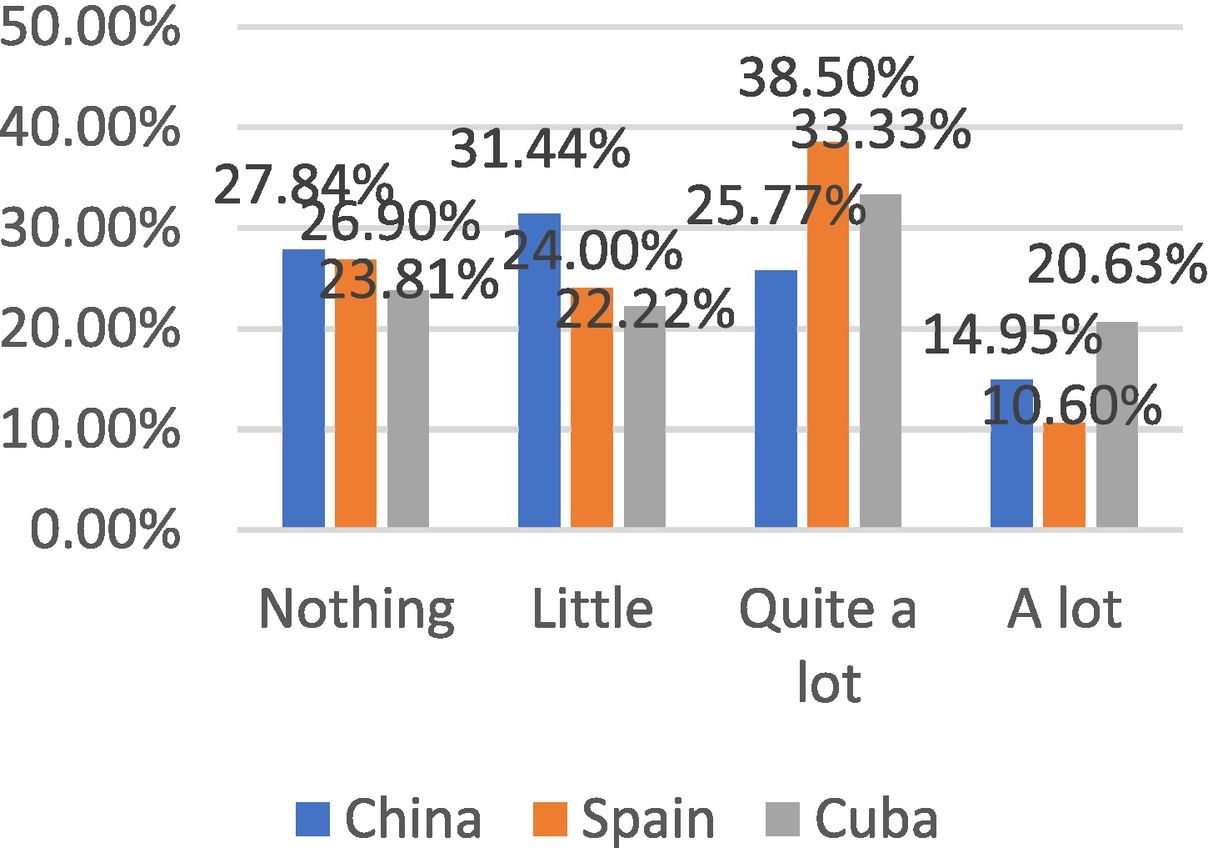
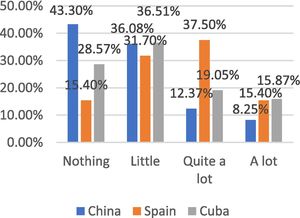
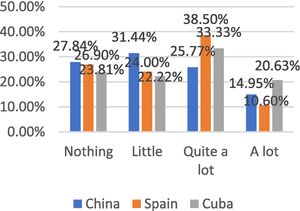
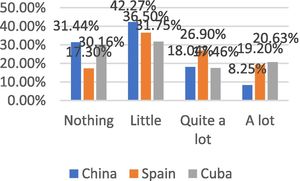
Impact of COVID-19 in different situationsFamily relationships and closest support networkIn the family support assessment, we could see that China had lowest percentage of “quite a lot” and “a lot” in three countries, while Spain exceeds 52.9% and Cuba was at an intermediate level. It means that different pandemic stages have affected relationships between friends, family, and colleagues differently (Fig. 6). Patients used digital or social media platforms more frequently in all three countries, probably due to maintain personal relationships (Fig. 7).
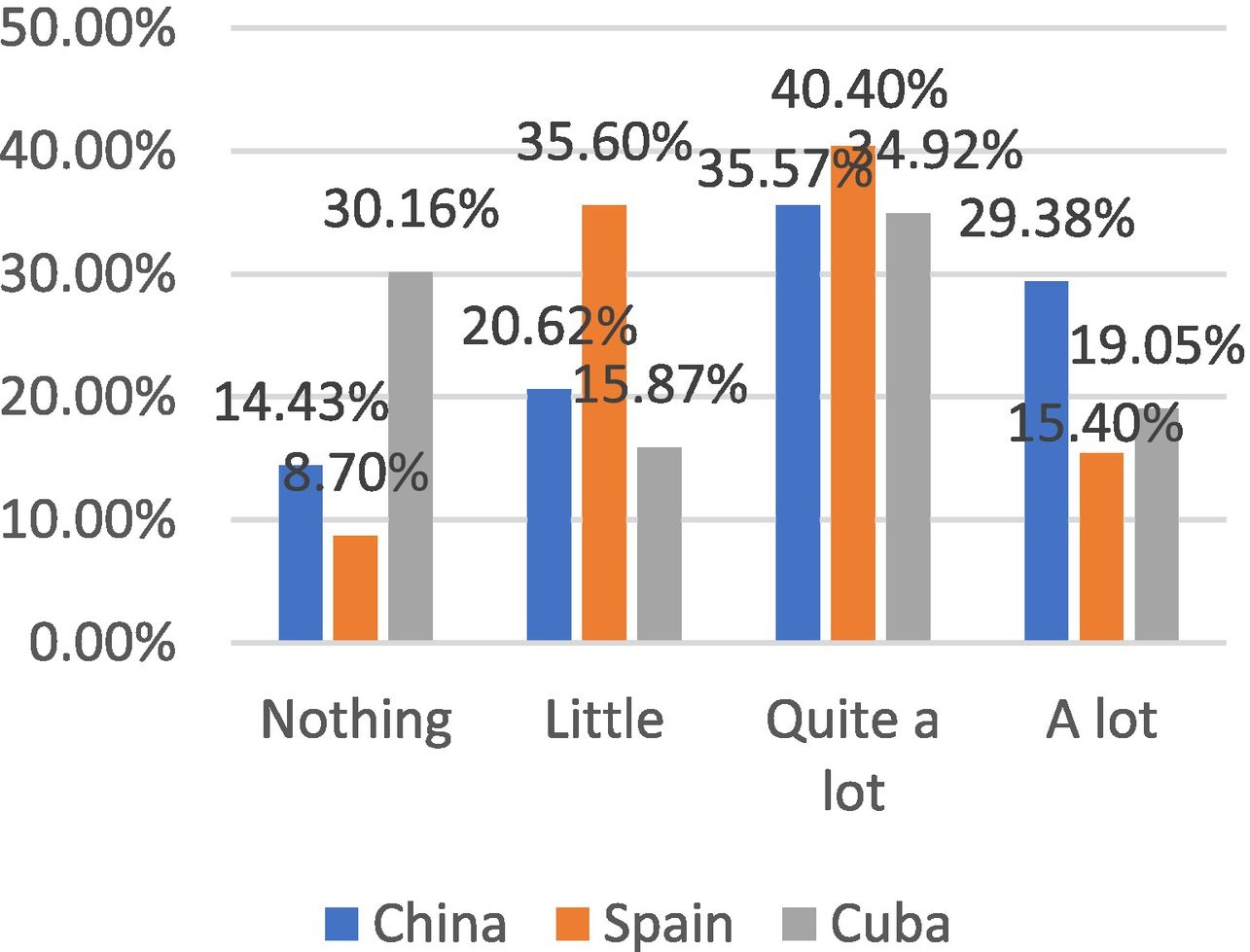
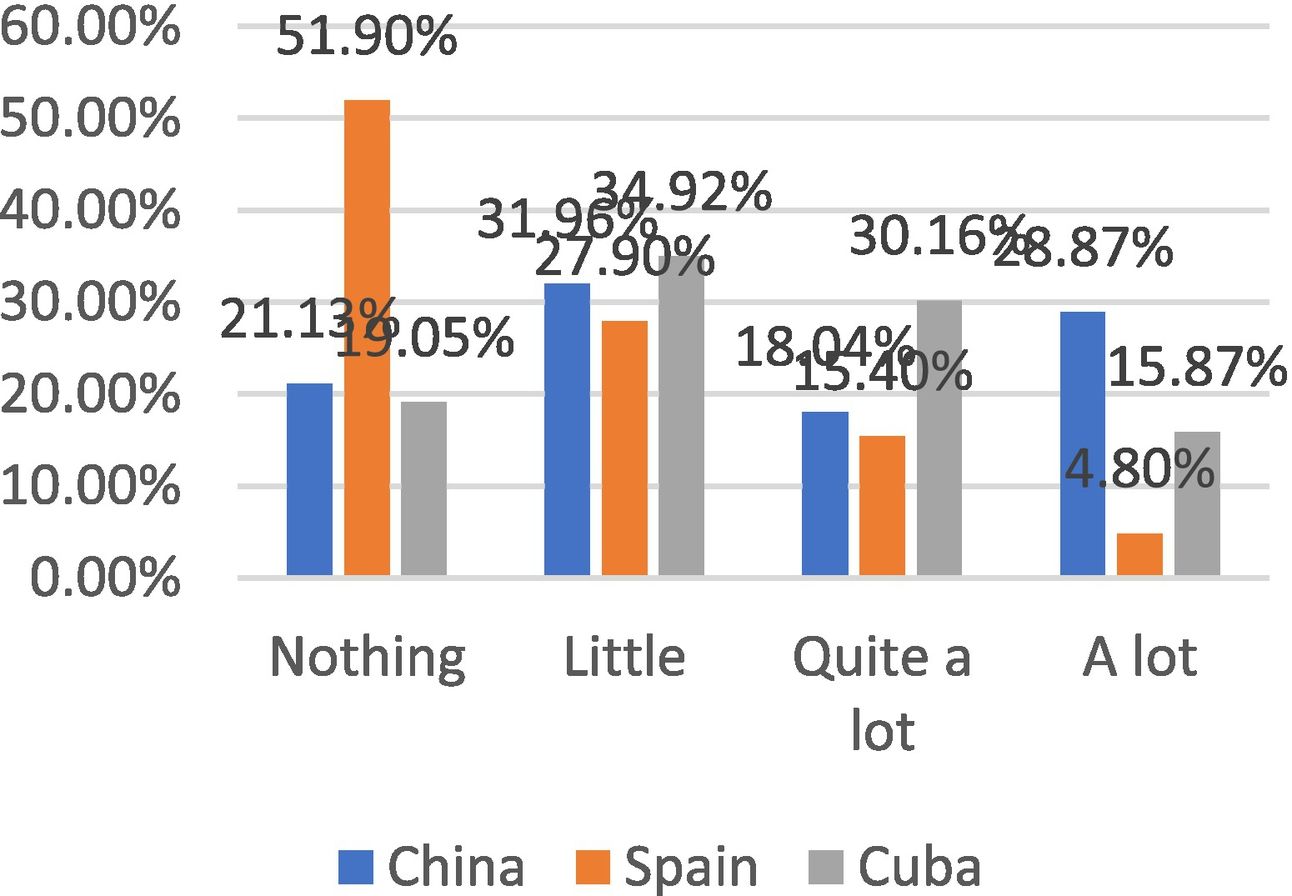
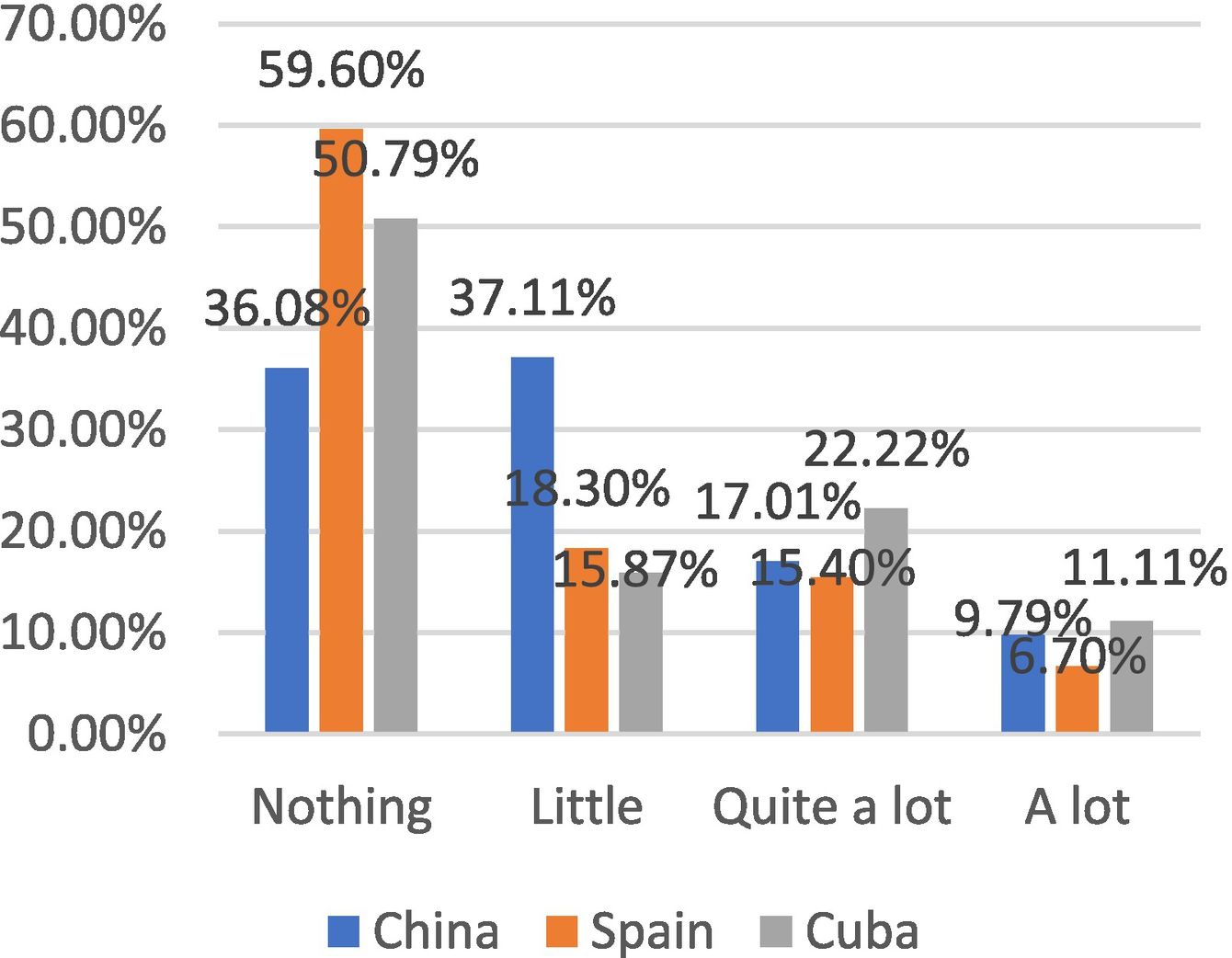
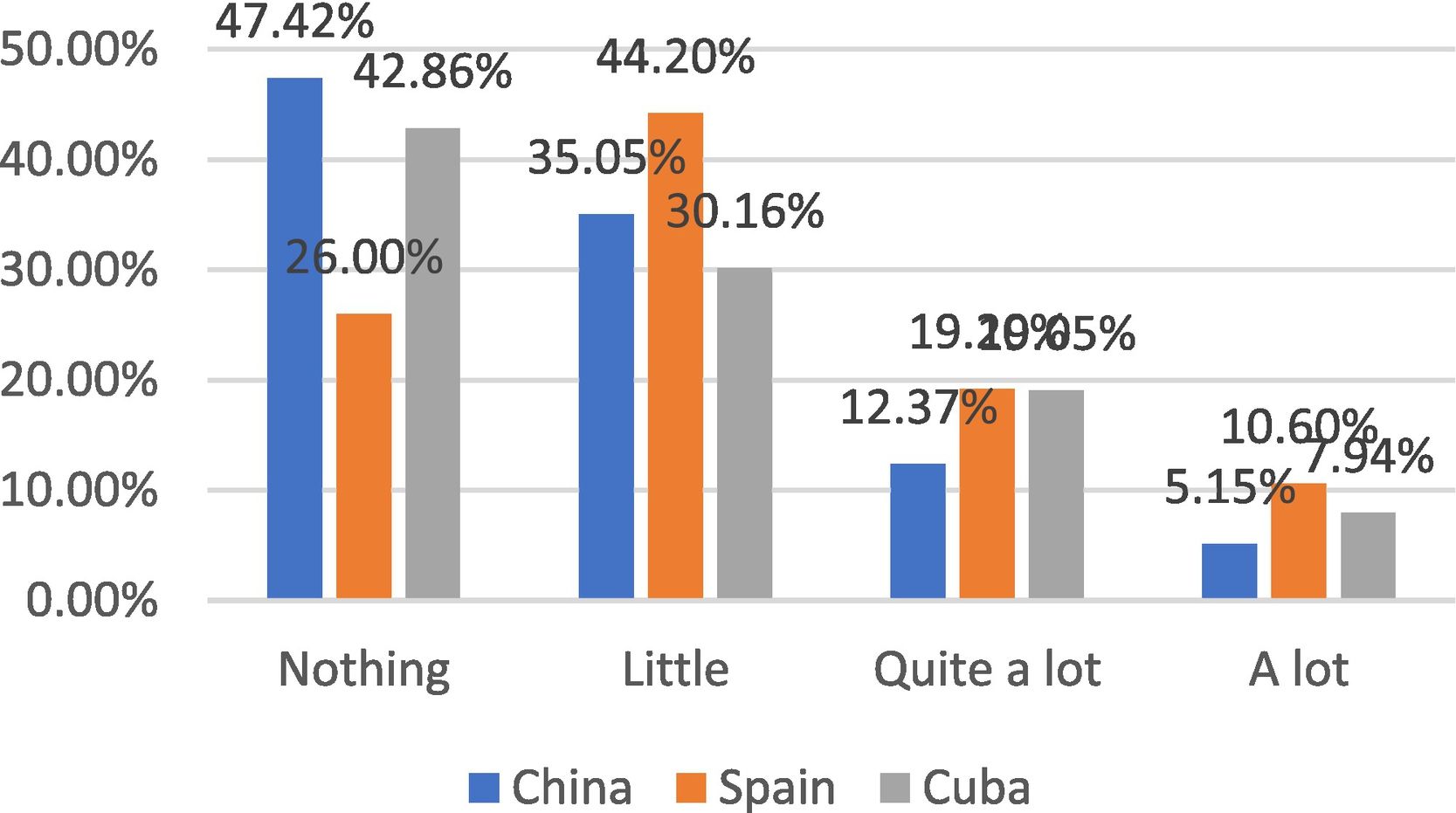
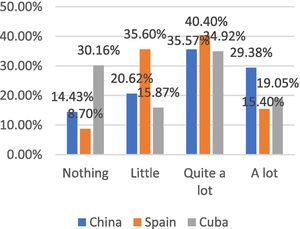
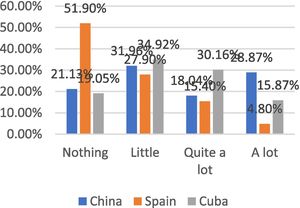
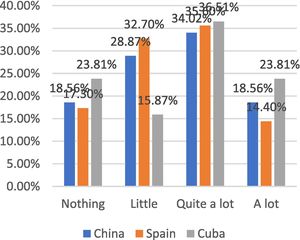
Regarding the changes in the work and study situation in Spanish patients, the enormous difference between 67.3% of the sum of “nothing”–“little” affected versus 32.7% of “quite a lot”–“a lot” is surprising. In the comparative analysis with China and Cuba we perceive that the percentages are equally distributed, the difference between both extremes is lower about Spain, with 59.28%, 53.97% of “nothing”–“little” compared to 40.72%, 46.03% of “quite a lot”–“a lot”, respectively (Fig. 8). We believed that this may reflect that MS patients have tended to have a medium-high socio-economic level in many cases due to the support of pensions for the disease. However, the work and study situation in families in China were better than in Cuba and Spain (Fig. 9). Regarding their economic status, Spanish MS patients received a significantly less negative impact than Cuba and China (Fig. 10).
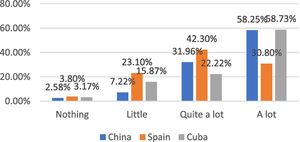
Psycho-cognitive disordersIn Figs. 11 and 12, we have found similar mental and cognitive effects in the three countries, China seemed to have a better situation, which could be related to the control before the pandemic in China. We could say that the effects of confinement have not varied dramatically in terms of cognitive impairment. This data will probably have to be assessed in the medium- and long term, since expected more critical problems when patients are evaluated at least six months after confinement.
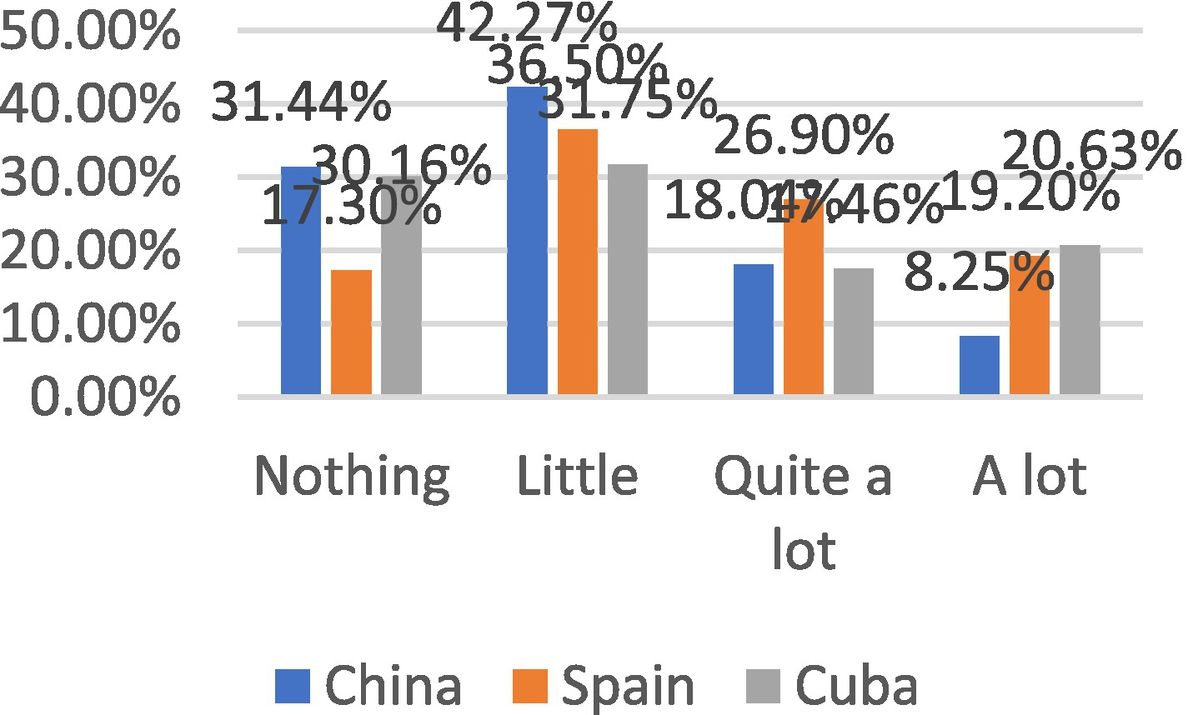
In terms of sleep disorders, China was significantly better than the others, patients from China had a significant difference between 73.71% of the sum of patients who had “nothing” or “little” compared to 24.23% of those who had “quite a lot” or “a lot”. Especially China had only 8.25% in “a lot”, however, Spain and Cuba had 19.2% and 20.63% respectively (Fig. 13).
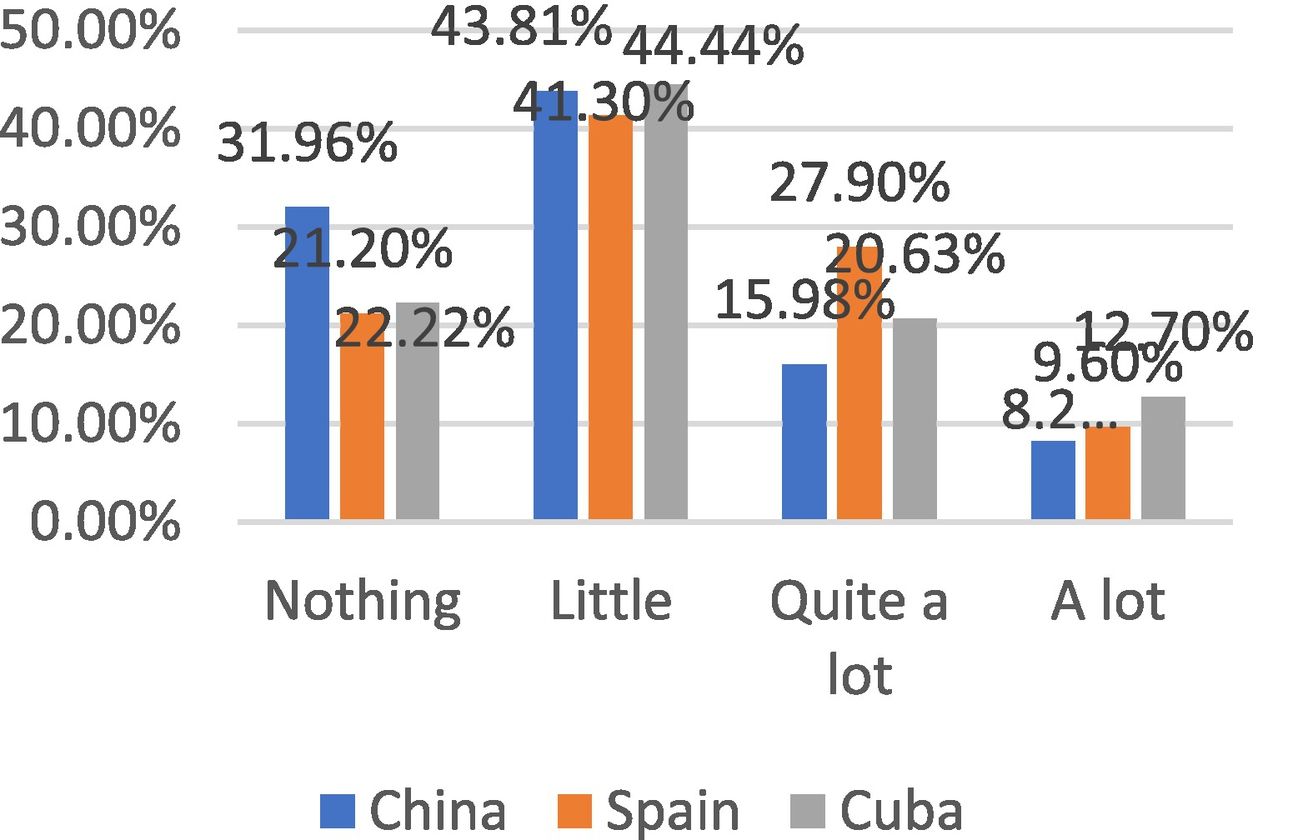
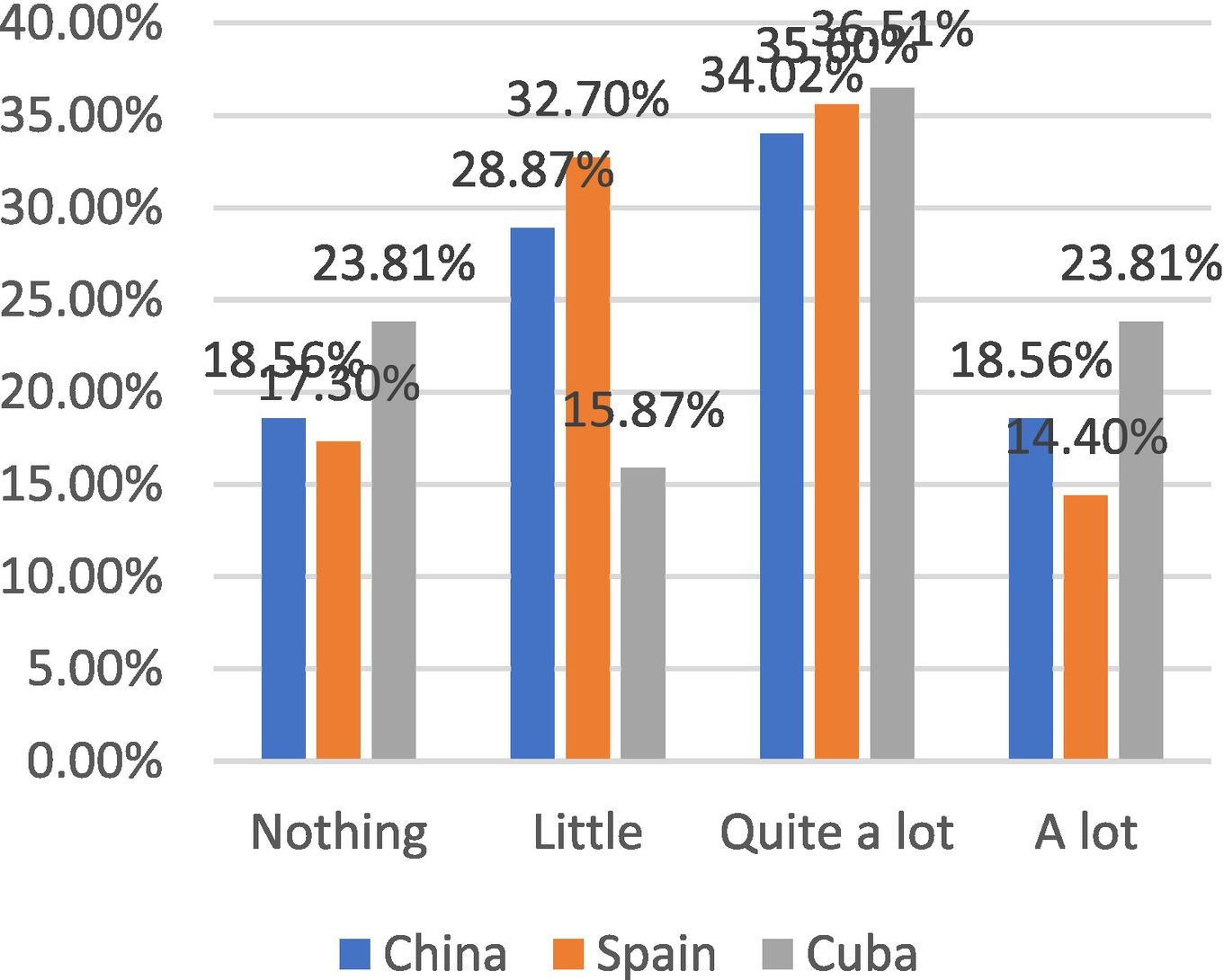
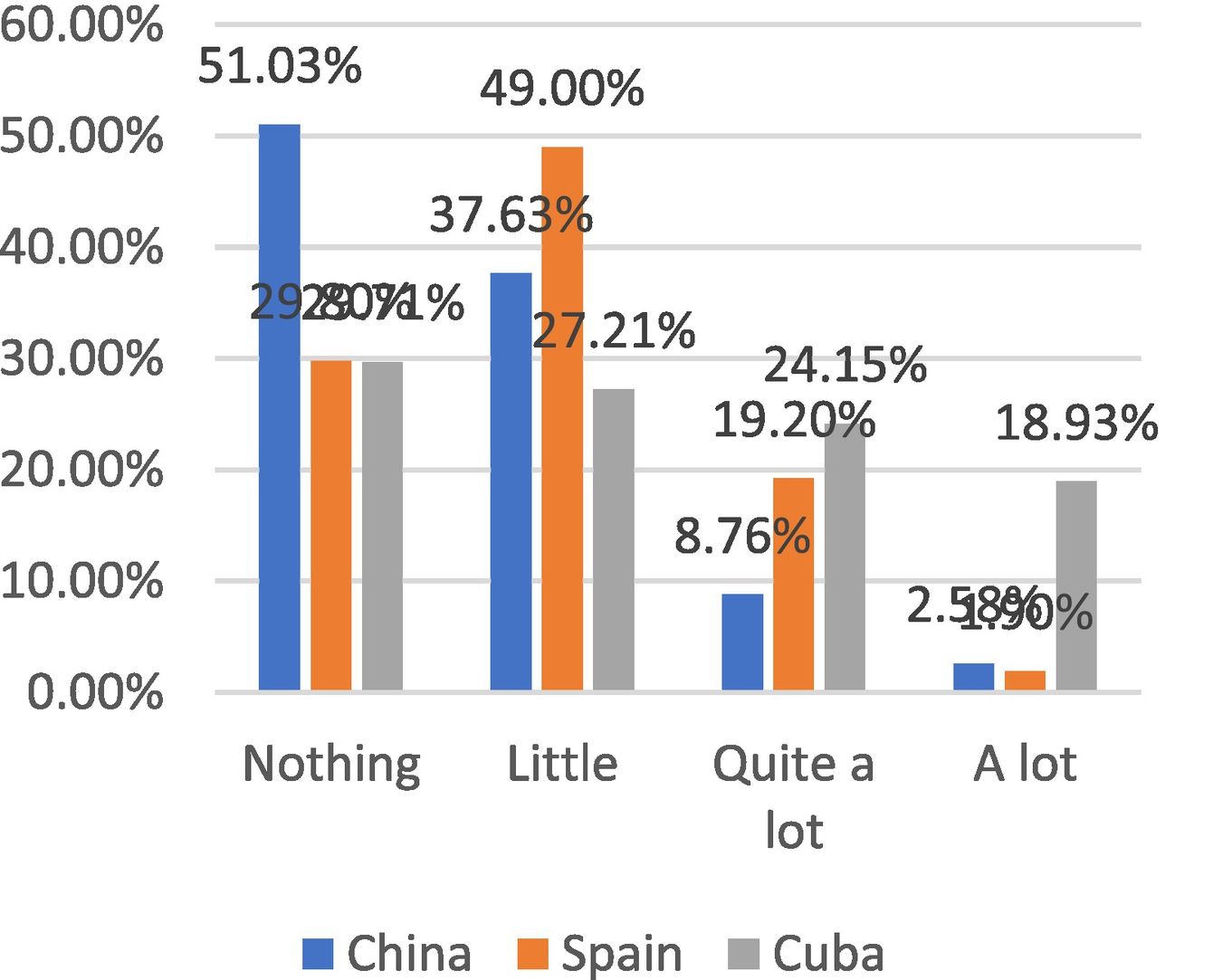
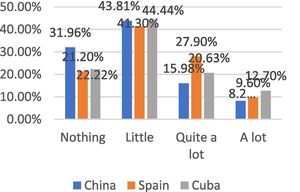
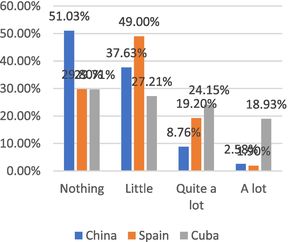
Lifestyle changesIn Fig. 14, we found that exercise time has decreased at specific points during the pandemic. Approximately a third of the patients reported that it has affected them quite a lot in the three countries in a similar way (China: 34.02%; Spain: 35.6%; Cuba: 36.51% respectively). Regarding the frequency of dietary changes, we could not find many changes. Half of the Chinese patients (51.03%) did not change their habits, and almost half of the Spanish patients (49.0%) changed very little. However, we found that the sum of “quite a lot” and “a lot” (43.08%) in Cuban patients, much more than the Spanish (21.1%), and the Chinese (11.34%) in Fig. 15.
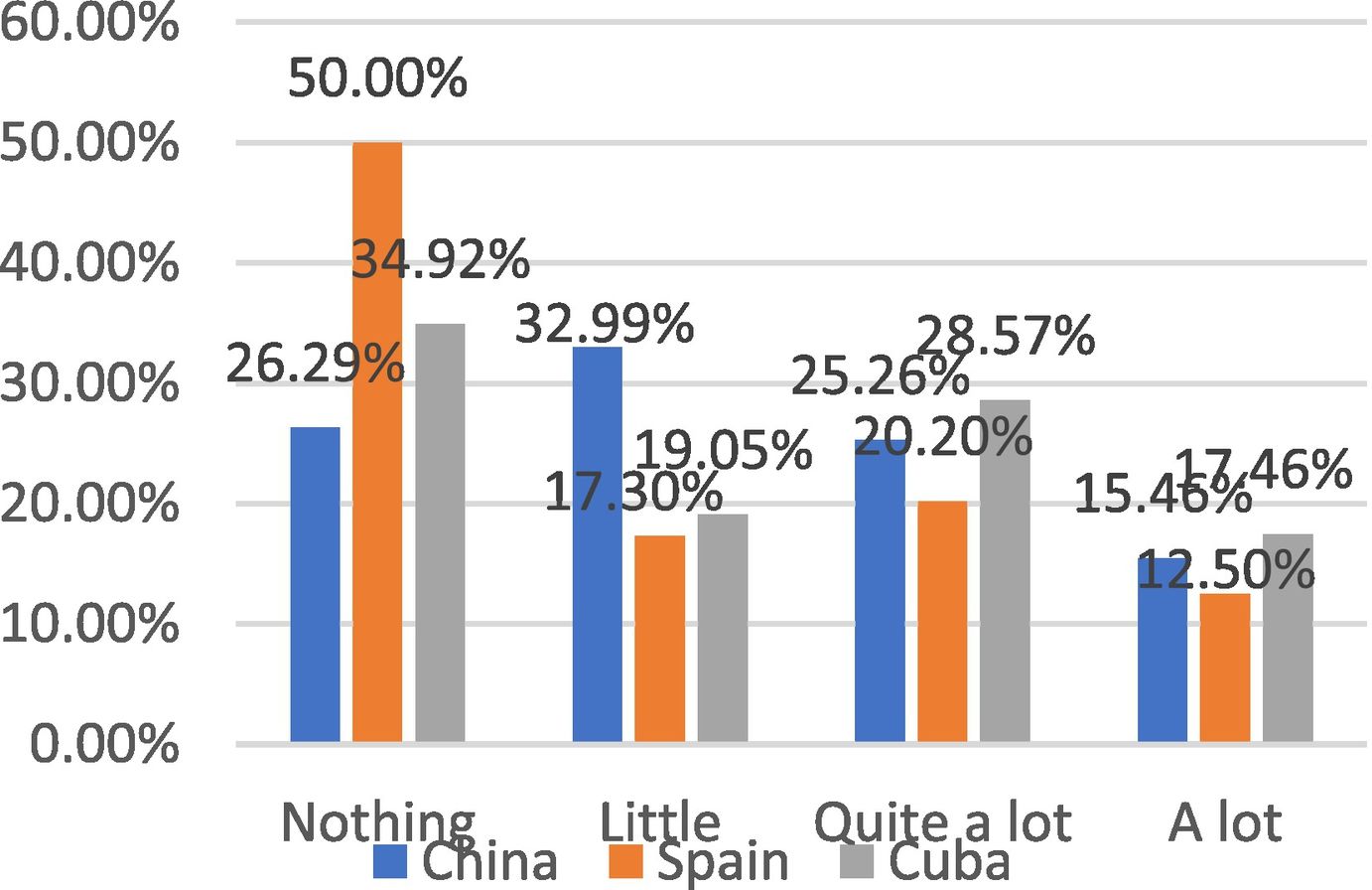
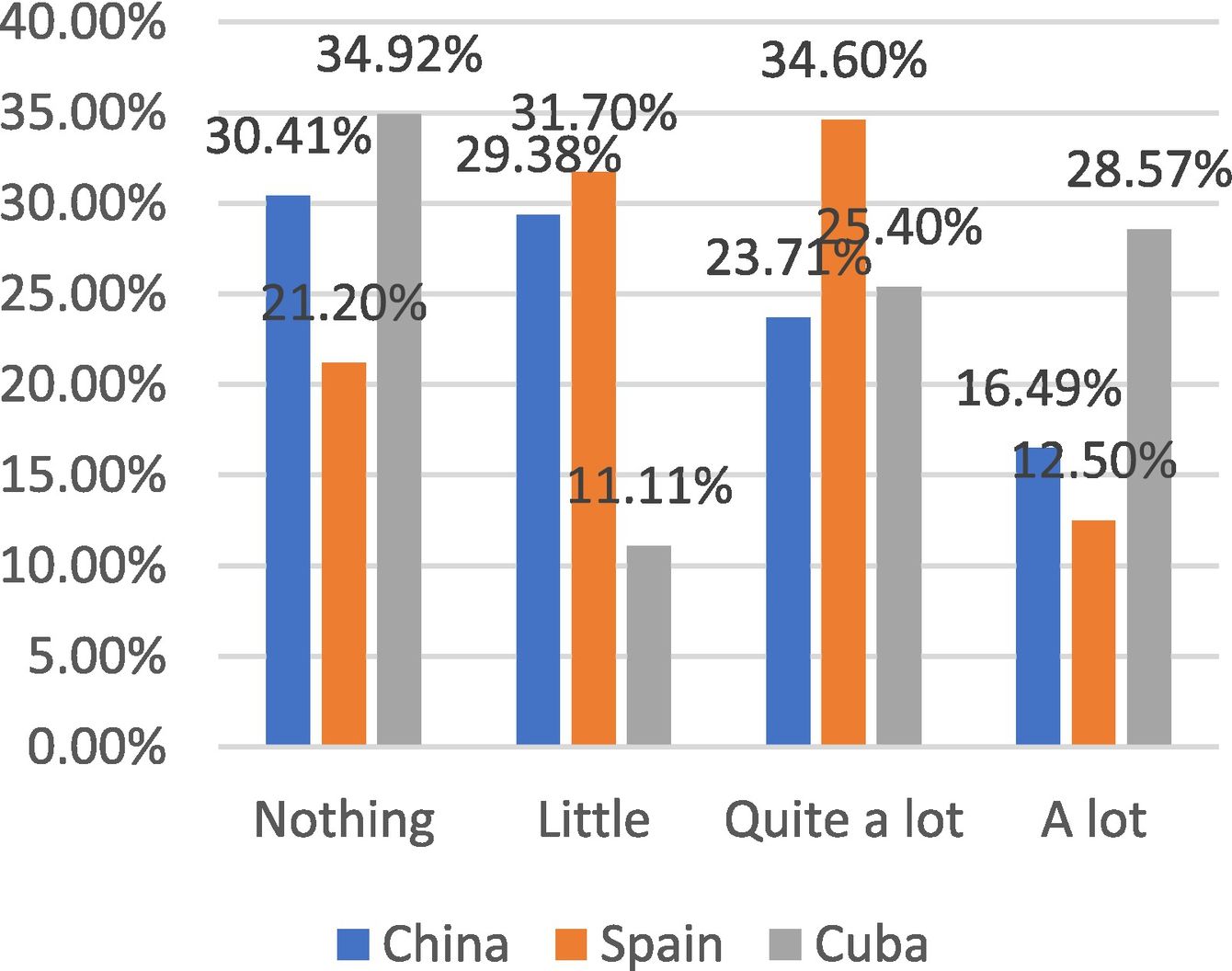
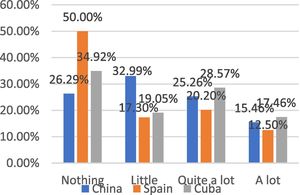
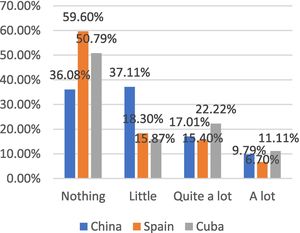
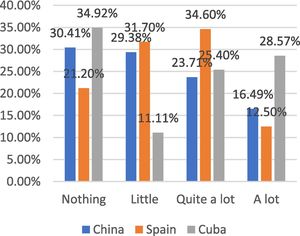
Transport and purchase alterationsIn Fig. 16, we have found that most of the patients considered that their means of transport had not modified o modified a little in the three countries (China: 73.19%; Spain: 77.9%; Cuba: 66.66%, respectively). As shown in Fig. 17, almost a third of Chinese patients (30.41%) and Cubans (34.92%) did not change the frequency of online purchases, where they found a higher proportion than Spanish (21.2%). More than a quarter of Cuban patients (28.57%) considered that it has changed a lot, and this proportion was double that of China (16.49%) and Spain (12.50%). The sum of intensity “quite a lot” and “a lot” of the Spanish (49.1%) and Cuban (53.97%) patients were found to be higher than that of China (40.2%), which may be due to the incredible power of making the purchase online in China.
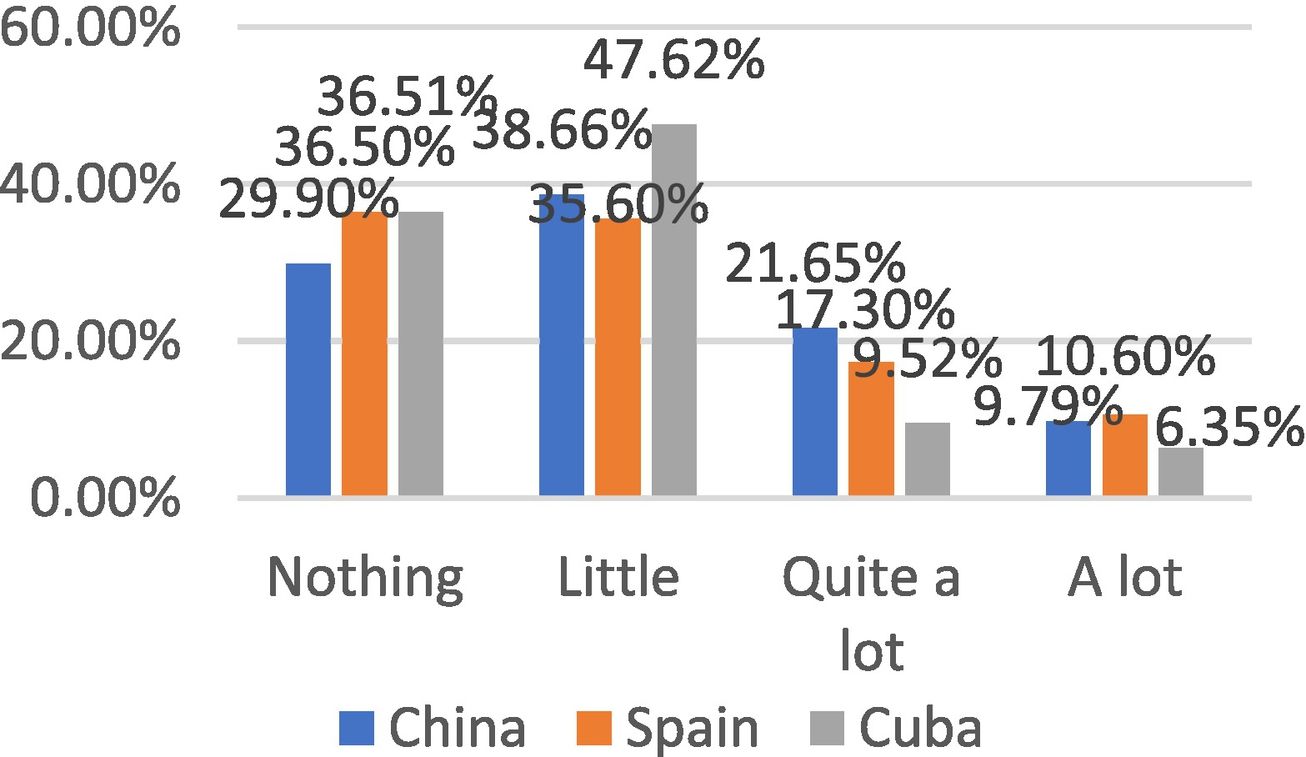
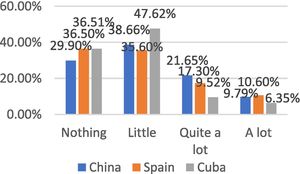
Physical health statusIn Fig. 18 we have found that most of the patients in the three countries have not deteriorated physically or have only presented a slight deterioration in their physical condition, especially the Chinese patients (82.47%) compared to the Spanish (70. 20%) and the Cubans (73.02%).
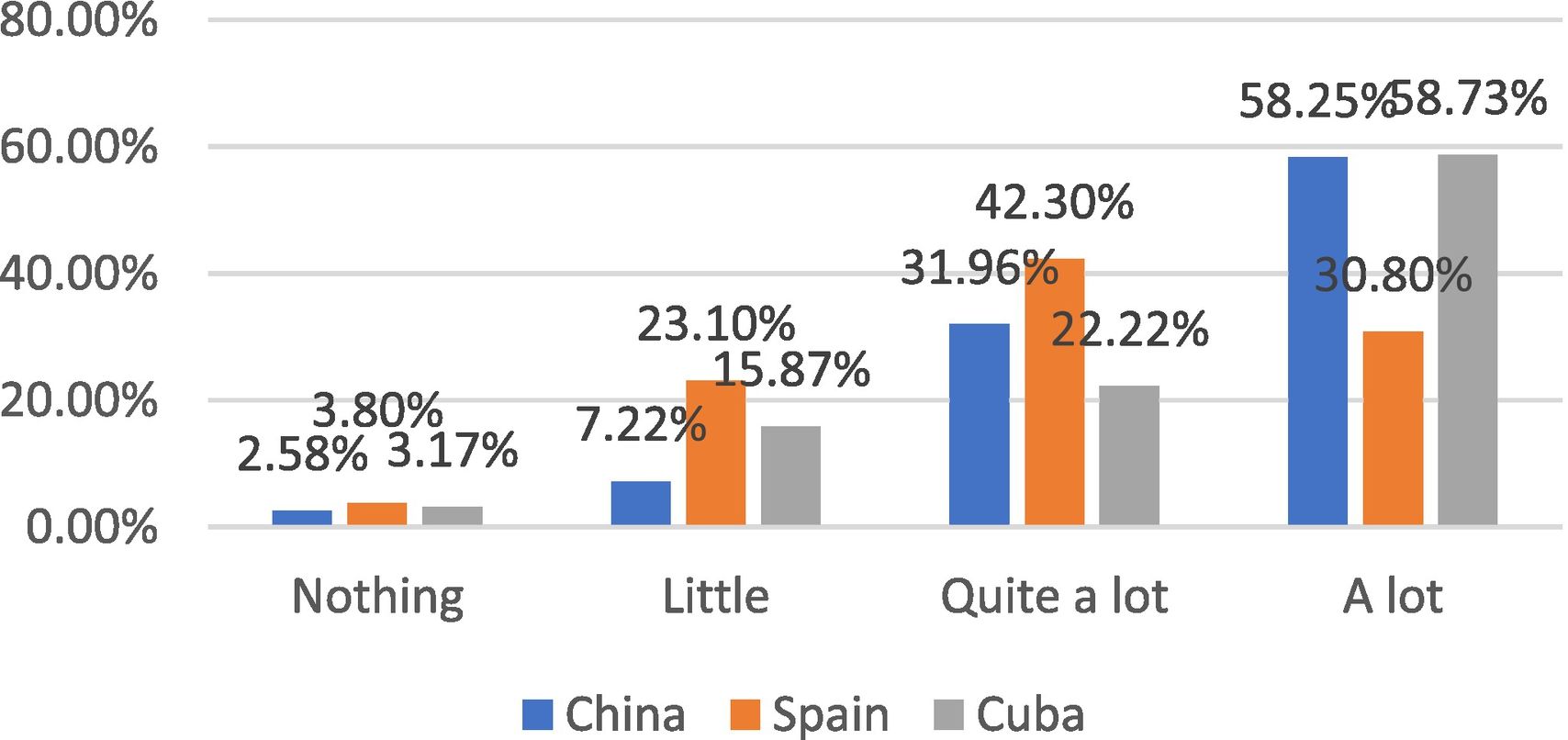
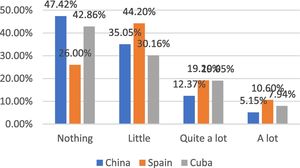
Confidence in beating COVID-19In general, patients from all three countries demonstrated confidence in beating COVID-19. However, Spanish patients have not presented strongly. More than half of the Chinese (58.25%) and Cuban (58.73%) patients have had a lot of confidence in overcoming it, almost twice that of the Spanish (30.80%) (Fig. 19).
DiscussionIn April, we have compared the socio-economic impact of COVID-19 on RRMS patients between China and Spain in a previous study.20 This research, a continuation of prior research, is based on studies of different races, countries, and continents and compares the impact of the new crown pandemic on RRMS patients (Chinese and Western) in three countries first time.
COVID-19 is raging across the planet, some countries such as Europe and Latin America have been secondary outbreaks to some extent. Under this situation, the aspect of labor, economic and training activity is badly affected.
In this study, the ratio of men to women was approximately 1:2. The mean age was 38.9 ± 12.1, China, Spain, and Cuba were 33.2 ± 9.2, 46.2 ± 10.2, and 46.2 ± 10.2, respectively. It declared the age range of MS patients are between 20 and 50 years of age; the ratio of men and women is about 1:2 ~ 3,23,24 which is matching to the epidemiological characteristics of MS.
One of the particularly significant findings of our study was that MS patients did not show a high rate of infection, relapse, and worsening rates of three countries were in the low percentage. Some research proved that continuing disease modification therapy in MS patients during an outbreak does not increase the risk of developing COVID-19.25,26 We consider that COVID-19 less affect MS patients. However, the interesting finding was that the relatives and friends of Spanish MS patients have been more susceptible to COVID-19; the proportion is 32.7% in Spain, 14.2% in Cuba, and 0.52% in China, The possible reason could be widespread of COVID-19 in Spain.27 Since Wuhan released from quarantine on April 8, the strict control of anti-epidemic measures by the Chinese government, there have been almost no other cases of MS with COVID-19 infection apart from sporadic cases in the past six months.
Although Spain currently is one of the countries most affected by COVID-19, it has less impact on the sick's work, training, and economy compared with China and Cuba in accordance; this is consistent with the results of our survey in April between China and Spain.20 Tourism has represented a very important source of income in Cuba, so that the pandemic has caused a great impact on its economy due to the closure of the borders. In the treatment respect, lack of imported medicine in Cuba and China restricted patient to receive effective treatment. Spain is less affected on patient treatment due to socioeconomic subsidies and a reliable health system and less medicine restriction. Specifically, Spanish patients were easily accessible to MS drugs. The weakness of Chinese healthcare still restricts patients to get medicine even this phenomenon has improved compared to six months ago. Besides, the age should be considered; since the patients of China are generally younger and the majority of the university students do not have work. Therefore, the COVID-19 could have some impact.
During the pandemic, visible effects were also observed in public transport and shopping modes, for many people, public transport is the main means, and sometimes it is the only one. A study has reported that 48% of Americans considered themselves to be taking public transport would increase the risk of infecting COVID-19, 2/3 participants believe that you have to be very careful when traveling by plane.28 The pandemic has affected the means of transportation in different ways.29 Because public transport is a closed space that favors the transmission of infectious diseases from person to person, it can become a vector of COVID-19. Compared with other two countries, China implement measures on improvement of public transportation safety such as strengthen ventilation of airports, train stations, bus stations, increase disinfection of stations and vehicles, augmenting ventilation, restriction of passenger flow.30 Until now, China had not had any massive transmission of Covid-19 caused by public transport services and therefore the effectiveness of these measures are effectively prevent massive spread of Covid-19 via public transport services in China.31 As described in this research, during the pandemic, people's travel mode was significantly influenced especially in transport.
Some studies show that before the pandemic in Spain, consumers bought food mainly in supermarkets (96.6%), small stores (39.21%) and on the Internet (7.56%). There are not significant changes during the period of COVID-19 (p = 0.095).32 Meanwhile, china showed that online shopping become to the mean trend. To be specific, storing or purchasing food online play a key role in people's daily life. There are no differences in the dietary diversity score of the families.33 But the data of online purchases in Cuba have increased significantly. Shopping online has been a common phenomenon in China and Spain; it has established a complete sector platform. However, the Cuban government has promoted the development of the digital business during the pandemic; for that reason, an evident increase in online shopping has been observed in Cuban patients concerning Chinese and Spanish patients.34
COVID-19 not only affects the physical state, but also affects its social, economic, and psychological aspects. Our study prioritizes those who might need more help, psychologists, professionals, and social workers, who offer mental health services can at least begin to solve mental health problems, even during their confinement. In these three countries, the frequency of digital use has increased, which may also be due to the popularity of telecommuting, online learning,35 and strengthened communication with families and friends.20 Studies have found that the daily amount of time spent looking at the screen is much higher than recommended for adults, which can contribute to mental illnesses, such as depression, etc.36
During the COVID-19 pandemic, more than half of the population experienced changes in their eating habits, decreased physical activity, and increased appetite.37 which is similar to our research in three counties. The reason is that the gym's closure, prohibition physical exercise in the park or sports field might restrict people to do exercise, which lead people more focus on cooking food. It can cause a sedentary lifestyle that favors the appearance of some chronic diseases such as obesity, high blood pressure, diabetes mellitus, cardiovascular disease, etc.38–41 Diet habit change is also related to quarantine, Robinson et al. reported that 56% of its casuistry was written with the increase in the frequency of the diet42 and is considered another risk factor related to the diseases above.40–42
The results of studies on confidence in beating COVID-19 are more subtle. In general, the severity of COVID-19 in a region and the results of government prevention measures have a positive effect on the confidence of the inhabitants of the region, and the relationship depends on the health and level of physical activity of the region/individual. In the countries most affected by COVID-19 (for example: Cuba and Spain), reduced exercise frequency, excessive food intake, and prolonged confinement trips may have little confidence in victory over COVID-19.
Primary health care (PHC) has played an indispensable role in the fight against COVID-19.43,44 The family and community approach of PHC, with a territorial and intersectoral perspective, may be contributing to better prevention and control of the pandemic. Spain and Cuba have established a universal PHC system, accumulating much experience to face the pandemic.11,45 However, COVID-19 has raised the alarm about PHC in China, especially in the place where it originates, with doctors' generous support in different regions and the central level, China achieved a success in Wuhan, and eventually at the national level.
This study has certain limitations. First, the study is based on an Internet questionnaire, the COVID-19 pandemic varies from country to country, might not reflect really situation. Secondly, the collected data were subdivided into three groups (China, Spain, and Cuba), and each group include less, it will lead to publication bias.
ConclusionDuring the pandemic, family support was more effective in China than in Cuba and Spain. Neither COVID-19 infections nor the number of outbreaks/relapses increased significantly in the confinement period in any of the three countries. Patients in all three countries used digital or social media platforms more frequently, probably to try to maintain personal relationships. The psychological and cognitive disorders of the patients will have to be studied at least within a year. Regarding their economic situation, Spanish MS patients received a significantly less negative impact than Cuba and China. The physical state has been maintained acceptably in the tres countries but especially better in China. The Chinese and Cubans trust more in the control of the pandemic than the Spanish, who are more pessimistic.
Authors' contributionsGuo-Xun Zhang, Run-Ze Zhao and Wen-Ting Zhang conceived and designed the study. Guo-Xun Zhang, Run-Ze Zhao and Wen-Ting Zhang responsible for data collection and analysis and drafted the manuscript. Wen-Jin Yu, Xiao-Jie Zhang, Shuai-Shuai Gao, IR. Olivera Leal, Maria Cáceres Toledo, Zurina Lestayo O'Farrill, Antonio Carrilllo-Vico, Jing-Ye Zhu and Pascual Amoedo R assist in data collection and provide advice. Izquierdo Guillermo and Gang Zhao responsible for conceptualization, reviewed and revised the paper. All authors read and approved the manuscript.
FinancingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
This study was supported by the Multiple Sclerosis Unit, Neurology Service, Vithas Nisa Hospital, Seville, Spain.