An 42-year-old man with a history of a diaphragmatic hernia, presented to the emergency department with dyspnea.
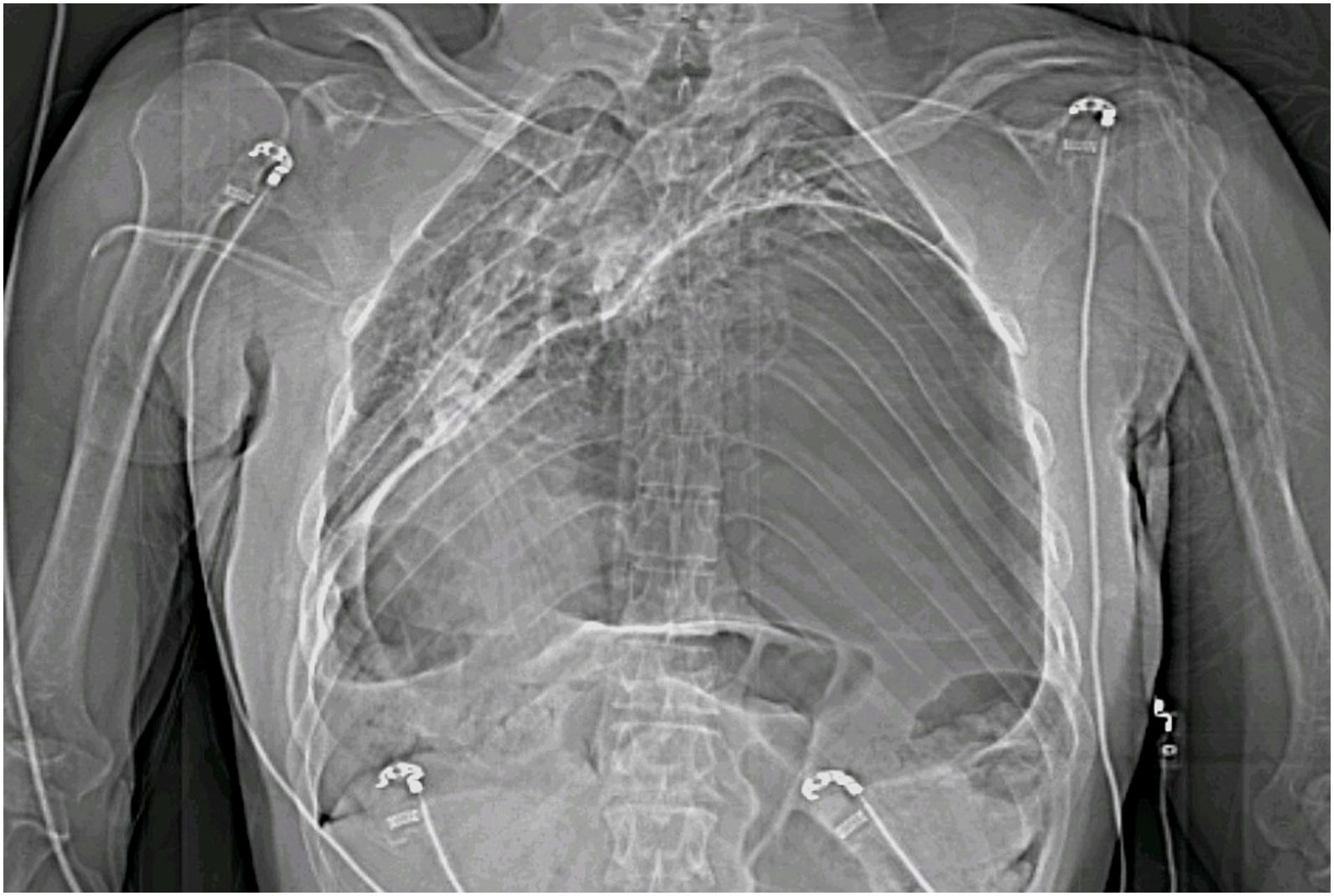
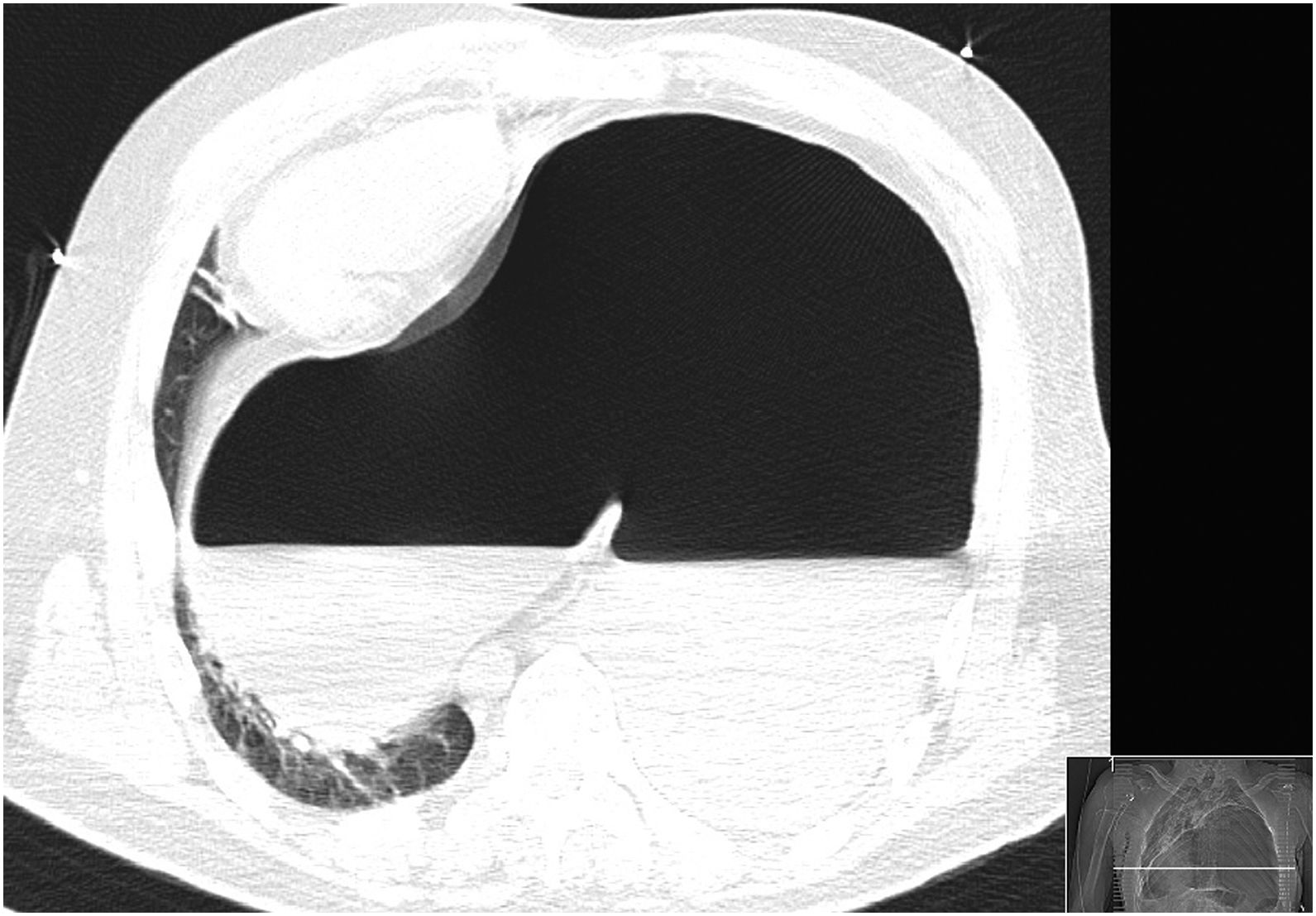
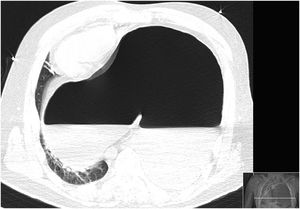
The physical examination findings were hypotension, tachycardia and tachypnea. The oxygen saturation was 80% (ambient air). He had thoracic asymmetry with no breath sounds in the left hemithorax (Figs. 1 and 2).
The arterial blood gasometry revealed an hypoxemic respiratory failure with metabolic acidemia and elevated lactate.
The CT scan of the chest showed diaphragmatic eventration with massively passage of hollow visceral organs to thoracic cavity, occupying almost the whole left hemithorax and part of the right, with compression of mediastinum and heart structures.
Emergent laparotomy was performed with reduction of intra-thoracic vísceras (all stomach, spleen and transverse colon).
He was transferred to intensive care, but the postoperative course was complicated with clinical deterioration and died.
A diaphragmatic hernia is a protrusion of abdominal contents into the thoracic cavity as a result of a defect within the diaphragm,1 and usually diagnosed in neonatal period.2 It is most common as a congenital phenomenon; however, there have also been cases where it can be acquired, mostly secondary to trauma which results in diaphragmatic rupture.3
Considering the circumstances and the absence of trauma, the case presented in this report is most likely due to a congenital hernia rupture.
Clinical awareness of this uncommon condition should be raised especially when evaluating patients with respiratory distress and atypical abdominal pain4 delay in appropriate diagnosis and management could result in significant morbidity and mortality.4,5
Authors highlight this uncommon condition as a cause of obstructive shock, which despite being quickly identified, has led to an adverse outcome.