The COVID-19 pandemic is attributed to SARS-COV-2 virus rapidly spreading around the world as a global health emergency. The difference in the rate of infection and disease severity has raised doubts about the impact of genetic predisposition on the COVID-19 severity. Previous studies have proposed the relationship between blood group antigens as one of genetic risk factors involved in susceptibility to COVID-19. Herein, we aimed to delve into the association between ABO blood group and COVID-19 infection, severity, and mortality rate.
MethodsIn this cohort study, the patients who referred to university-based referral hospital (Hazrat Rasool) in Tehran, Iran, with the positive PCR test for COVID-19 were followed up during 2021. They were classified as: (1) mild, (2) moderate, (3) severe, and (4) death based on disease severity. The demographic information including age, gender, and underlying disease and the patient's medical record such as blood type, intubation, and severity of illness was recorded. Then, the predefined variables were recorded in each group and compared with each other. Finally, the obtained findings were analyzed by SPSS version-22 software.
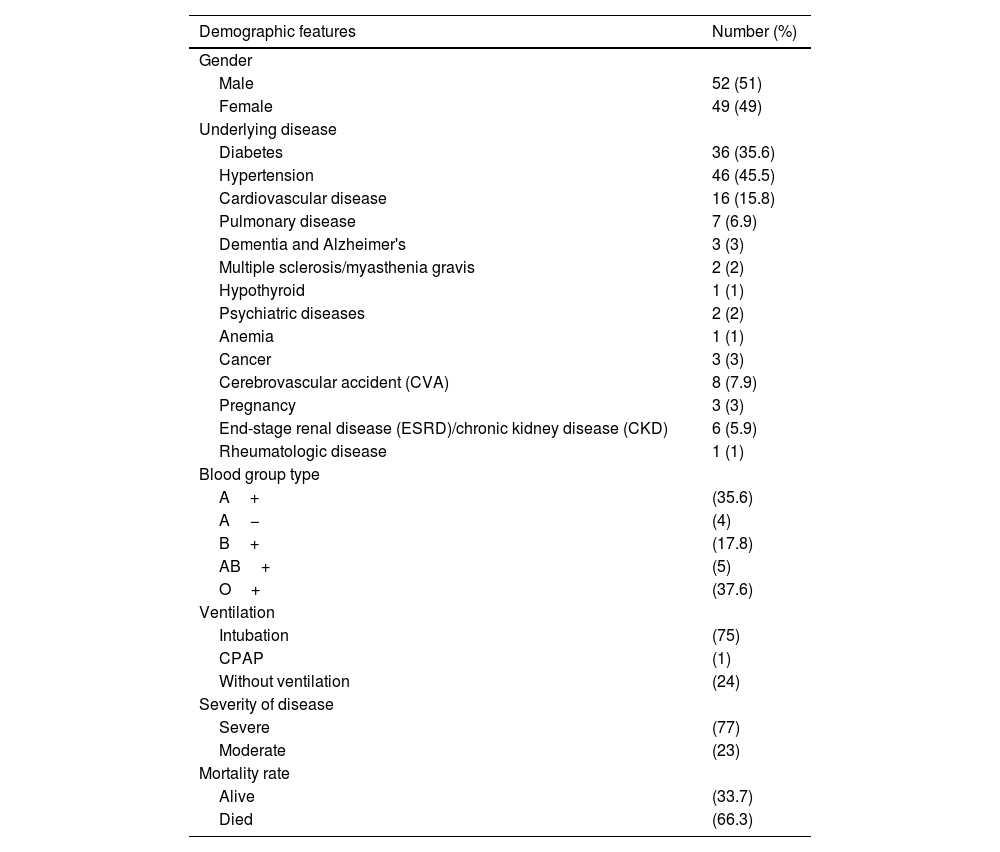
ResultsOverall, 101 patients were included among which 51.5% (52 cases) were male and the rest were female. Their average age was 64.14±16.37 years (ranged from 20 to 94 years). The most common blood group in affected cases was O+ (37.6%) and then A+ (35.6%). Also, the most underlying disease was hypertension and diabetes with a prevalence of 45.5% and 35.6%, respectively. 66.3% of cases died and 76.2% and 22.8% of cases presented severe and moderate form of COVID19, respectively. The average hospitalization time was 19.77±18.34 days (the longest time of 150 days) compared to the 12.79±10.45 days in ICU (the longest time of 55 days). In addition, the most common blood group amongst the hospitalized cases was O+ which were significantly associated with the lower severity and mortality rate of COVID19 (p-value ≤.0001).
ConclusionsThe findings of current study suggest that A+ blood group might be more susceptible to COVID-19 with significantly higher severity or mortality rate of disease while O+ blood group might be less susceptible with longer survival and less severity of disease. Our results add to the growing body of evidences suggesting the blood group types may pave the way for early preventive measures and management approaches of COVID-19.
La pandemia de COVID-19 se atribuye a la rápida propagación del virus SARS-COV-2 por todo el mundo como una emergencia sanitaria mundial. La diferencia en la tasa de infección y la gravedad de la enfermedad ha generado dudas sobre el impacto de la predisposición genética en la gravedad del COVID-19. Estudios anteriores han propuesto la relación entre los antígenos de los grupos sanguíneos como uno de los factores de riesgo genéticos implicados en la susceptibilidad a la COVID-19. En este documento, nuestro objetivo fue profundizar en la asociación entre el grupo sanguíneo ABO y la infección, gravedad y tasa de mortalidad por COVID-19.
MétodosEn este estudio de cohorte, se realizó un seguimiento de los pacientes remitidos al hospital universitario de referencia (Hazrat Rasool) en Teherán, Irán, con una prueba de PCR positiva para COVID-19 durante 2021. Se clasificaron como (1) leves, (2) moderada, (3) grave y (4) muerte según la gravedad de la enfermedad. Se registró la información demográfica, incluida la edad, el sexo y la enfermedad subyacente, y el historial médico del paciente, como el tipo de sangre, la intubación y la gravedad de la enfermedad. Luego se registraron las variables predefinidas en cada grupo y se compararon entre sí. Finalmente, los hallazgos obtenidos fueron analizados mediante el software SPSS versión 22.
ResultadosEn total se incluyeron 101 pacientes de los cuales el 51,5% (52 casos) fueron hombres y el resto mujeres. Su edad promedio fue de 64,14 ± 16,37 años (osciló entre 20 y 94 años). El grupo sanguíneo más común en los casos afectados fue el O+ (37,6%) y luego el A+ (35,6%). Asimismo, la enfermedad más subyacente fue la hipertensión y la diabetes con una prevalencia del 45,5% y 35,6%, respectivamente. El 66,3% de los casos falleció y el 76,2% y 22,8% de los casos presentaron forma grave y moderada de COVID19, respectivamente. El tiempo medio de hospitalización fue de 19,77 ± 18,34 días (el tiempo más largo de 150 días) frente a los 12,79 ± 10,45 días en UCI (el tiempo más largo de 55 días). Además, el grupo sanguíneo más común entre los casos hospitalizados fue O+, que se asoció significativamente con una menor gravedad y tasa de mortalidad de COVID19 (valor de p≤0,0001).
ConclusionesLos hallazgos del estudio actual sugieren que el grupo sanguíneo A+ podría ser más susceptible al COVID-19 con una gravedad o tasa de mortalidad de la enfermedad significativamente mayor, mientras que el grupo sanguíneo O+ podría ser menos susceptible con una supervivencia más larga y una menor gravedad de la enfermedad. Nuestros resultados se suman al creciente conjunto de evidencias que sugieren que los tipos de grupos sanguíneos pueden allanar el camino para medidas preventivas tempranas y enfoques de manejo de COVID-19.
The novel Coronavirus SARS-CoV-2, as leading cause of COVID-19 disease and rapidly spreading, is one of the most global health problems.1 A number of risk factors has been attributed to COVID-19 morbidity including age, gender, smoking, hypertension, and diabetes, chronic cardiovascular and respiratory diseases leading to health-related severe outcomes.1–4 The ABO gene is associated with a number of traits and risk factors including ABO blood types reflecting genetic polymorphisms, activity of the angiotensin converting enzyme,5,6 hematocrit and hemoglobin concentration,7 red blood cell count, von Willebrand factor,8 coronary artery disease and myocardial infarction,5,9 ischemic stroke,10 diabetes type II,11 thromboembolism as well as severity of COVID-19.12–15 The growing body of evidences has been indicated that there were associations between ABO blood groups and severity in a number of infectious disease including SARS-CoV-1,16H. pylori,17N. gonorrhoeae,18 hepatitis B,19 and Norwalk virus.20
Previously published studies were pointed to the real associations between blood group types and COVID-19 mortality and morbidity rate.21 Findings of a meta-analysis showed that non-O+ blood group is amongst the most sensitive genetic factors for thromboembolism and coagulopathy,22 as the main aspects in COVID-19 pathology which must be carefully managed.23,24 Based on the findings of genome-wide association studies, there was association between the multiple genes and loci and increasing risk of COVID-19 respiratory failure.25 In addition, there was no correlation between ABO blood type and COVID-19 severity in a UK study.26 Other Danish study has introduced the ABO blood group as a risk factor of SARS-CoV-2 viral infection but not for long hospitalization stay or COVID-19 mortality rate.27 There are conflicting reports due to multiple confounding effects on the relation between outcomes severity and genetics in COVID-19 patients. As a consequence, controversy remains with respect to whether diverse dominance of the blood subgroups and variants are related to the COVID-19 and which of these antigens are protective or risk factor. Further study in this area might have a significant impact on the management of treatment costs and healthcare systems. The current study was designed to elucidate the relationship between ABO blood group and COVID-19 severity and mortality rate.
MethodsThis population-based, retrospective cohort study was conducted in a university based referral center, Hazrate Rasoul hospital in 2021. According to the census method, all the patients (101 cases) who were hospitalized due to COVID-19 were included to determine blood group type. A checklist was prepared to enter demographic information including age, gender, and underlying disease with the patient's medical records such as blood type, intubation, and severity of illness. All retrieved data were recorded from the confirmed cases through the real-time polymerase chain reaction (RT-PCR). The ABO and Rh testing was performed using a hem-agglutination assay per the manufacturer’s instructions and slide method was applied to detect the reaction of the antibodies including anti-A, anti-B, anti-AB, and anti-D antigens for Rh indicating the presence or absence of the corresponding antigen in blood samples.
Data analysisData were analyzed using SPSS statistical software (version 22; SPSS). Quantitative data was reported using descriptive statistics as the mean and standard deviation and qualitative data was reported as percentage. Then, a χ 2 test was used to determine the relationship between blood group and morbidity and mortality of patients. A level of .05 was considered in terms of statistically significant variables.
ResultsDemographic features of COVID-19 patientsTo evaluate the effect of blood group on the incidence and severity of COVID-19 disease, 101 patients, admitted to Hazrat Rasool Akram Hospital in 2021, were included among which 51.5% (52 cases) were male and the rest were female. The average age of all cases was similar, 64.14±16.37 years old ranged from 20 to 94 years. The most common blood group in affected cases was O+ (37.6%) followed by A+ (35.6%). Besides, the most common underlying disease was hypertension with a prevalence of 45.5%, which can be summarized as the distribution of underlying diseases in Table 1. In terms of disease severity, 75.2% of cases underwent intubation, 1% of them underwent CPAP, and the rest did not undergo ventilation. Moreover, 76.2% of cases had severe disease and 22.8% of them had moderate disease among which 66.3% of them finally died. The average hospitalization time of cases in ICU was 12.79±10.45 days and the average hospitalization time was 19.77±18.34 days. The longest hospitalization time in ICU was 55 days and the longest hospitalization time was 150 days.
Demographic features of patients with COVID-19.
| Demographic features | Number (%) |
|---|---|
| Gender | |
| Male | 52 (51) |
| Female | 49 (49) |
| Underlying disease | |
| Diabetes | 36 (35.6) |
| Hypertension | 46 (45.5) |
| Cardiovascular disease | 16 (15.8) |
| Pulmonary disease | 7 (6.9) |
| Dementia and Alzheimer's | 3 (3) |
| Multiple sclerosis/myasthenia gravis | 2 (2) |
| Hypothyroid | 1 (1) |
| Psychiatric diseases | 2 (2) |
| Anemia | 1 (1) |
| Cancer | 3 (3) |
| Cerebrovascular accident (CVA) | 8 (7.9) |
| Pregnancy | 3 (3) |
| End-stage renal disease (ESRD)/chronic kidney disease (CKD) | 6 (5.9) |
| Rheumatologic disease | 1 (1) |
| Blood group type | |
| A+ | (35.6) |
| A− | (4) |
| B+ | (17.8) |
| AB+ | (5) |
| O+ | (37.6) |
| Ventilation | |
| Intubation | (75) |
| CPAP | (1) |
| Without ventilation | (24) |
| Severity of disease | |
| Severe | (77) |
| Moderate | (23) |
| Mortality rate | |
| Alive | (33.7) |
| Died | (66.3) |
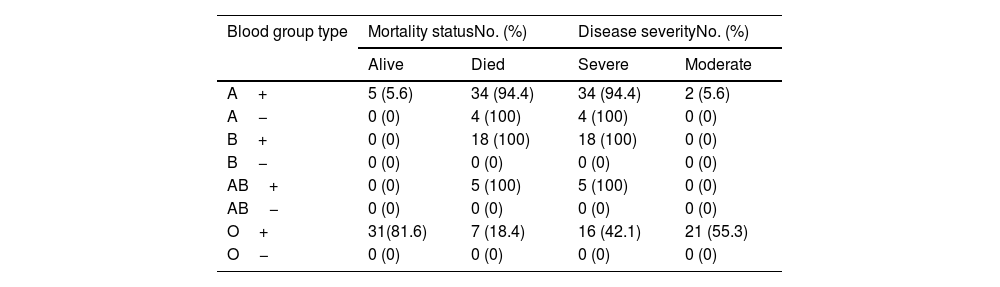
To assess the prognostic role of blood group type on disease severity and mortality rate, the χ2 test was used, which blood group showed a significant relation with ventilation (p-value=.001). It was also found that the blood group is related to the severity of the disease and mortality rate of patients. As shown in Table 2, the cases with O+ blood group as the most common blood group among hospitalized population, had a significantly lower disease severity (p-value=.0001) and less mortality rate (p-value=.0001).
COVID-19 severity and mortality based on blood group type.
| Blood group type | Mortality statusNo. (%) | Disease severityNo. (%) | ||
|---|---|---|---|---|
| Alive | Died | Severe | Moderate | |
| A+ | 5 (5.6) | 34 (94.4) | 34 (94.4) | 2 (5.6) |
| A− | 0 (0) | 4 (100) | 4 (100) | 0 (0) |
| B+ | 0 (0) | 18 (100) | 18 (100) | 0 (0) |
| B− | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| AB+ | 0 (0) | 5 (100) | 5 (100) | 0 (0) |
| AB− | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| O+ | 31(81.6) | 7 (18.4) | 16 (42.1) | 21 (55.3) |
| O− | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
To decide if a sample comes from a population with a specific distribution, the Kolmogorov–Smirnov test was used which showed that the age (p-value=.014) and time of hospitalization in the ICU (p-value=.0001) and the hospital ward (p-value=.0001) did not follow the normal distribution. Furthermore, by using the Kruskal–Wallis as a non-parametric test, it was found that blood type has no significant association with the age of hospitalized patients (p-value=.197) and the time of hospitalization in ICU (p-value=.450) and hospital ward (p-value=.463). Analytical assessment of findings using the multinomial logistic regression model indicated that blood type is an influencing factor on the severity of the disease and the mortality of patients (p-value=.0001). Evidently, it was found that gender is one of the main prognostic factors affecting mortality (p-value=.0001) and females (38%) survived longer than males (28%) (Table 2).
DiscussionToday, based on many studies that have been published regarding COVID-19, we know that this viral disease affects almost all organs, including kidneys, liver, lungs, eyes, skin, heart, etc. Sometimes, these side effects are so fatal leading to the death of the patient.28–37 So, the need to assess possible relationship between risk factors and COVID-19 development is rationale. One of the discussed factors is ABO group of people to develop COVID-19. The association of blood groups with several infectious diseases has been described and may partially explain regional differences in the distribution of infectious diseases. Famous examples are the association of ABO blood groups with several bacterial infections,38 for example, the association between cholera severity and the O phenotype.39 Not only infectious disease but also non-infectious disease can be related to ABO group. In summary, almost all diseases have a relationship with ABO group. According to the some comprehensive reviews, the risk of coronary heart disease is lower in blood type O. Some think it may be because other blood types are more likely to have higher cholesterol and more protein associated with blood clotting. Blood groups A, AB, and B are more at risk than group O. Especially people with blood type A are more likely to get stomach cancer. Researchers believe that this may be because Helicobacter pylori infection is more common in people with type A blood. People with AB blood type had more memory problems than others. People with blood type A tend to have more cortisol. Therefore, these people may be less resistant to deal with stressful situations. O blood type may help ward-off malaria. Peptic ulcers and painful open ulcers that appear on the wall of the stomach or upper intestine seem to be more common in people with blood type O. Research shows that people with blood type A, B, or AB are more at risk of blood clots. If the blood type is O, the probability of a person's longevity is higher. Experts believe that reducing the risk of cardiovascular disease may be one of the reasons for this. Type 2 diabetes seems to occur more often in people with blood types A and B. Experts don't know why. More research is needed. The risk of stroke increases in AB blood type.40–48
Similar to SARS-CoV-1, the association of ABO blood with the severity of COVID-19 or different risks of infection with SARS-CoV-2 has been debated for several months. Regarding the possible association between the different probabilities of contracting SARS-CoV-2 or the severity of COVID-19, several explanations have been proposed to address the presence of AB antibodies as described above for SARS-CoV-1.49 In addition, some authors have recently proposed different degrees of protection.50 Several studies have reported the possible relationship between the ABO blood group and the susceptibility to COVID-19 disease. Conversely, conflicting findings have been obtained from some studies.51 A number of risk factors has been identified to be associated with the COVID-19 progression into a severe and advanced stages, including age, gender, smoking, in addition to underlying disease such as hypertension, diabetes, chronic cardiovascular and respiratory diseases, cancers, immunodeficiency, pregnancy, liver, and kidney diseases.52,53 Therefore, better understanding of COVID-19 relation with clinicopathological characteristics as well as genetic predisposition in involved patients is imperative given the toll of the current pandemic.54,55 It has been demonstrated that the ABO and Rh systems dominance as well as their linkage with the COVID-19 disease may differ among populations55; therefore, the present study was conducted with the aim of investigating the association between ABO blood group and the severity of COVID-19 disease and mortality rate in 101 patients admitted to Hazrat Rasool Akram Hospital in 2021. In this study, we found that the most common blood group among hospitalized patients was O positive blood group and with a small distance A positive blood group. However, it has been indicated that the risk of COVID-19 exposure is lower in patients with blood type O when compared to other types, and it seems that blood type O is a protective factor.56 In our study, patients with blood group A were more likely to experience severe infection of COVID-19 with significantly higher mortality rate after contracting SARS-CoV-2, whereas patients with blood group type O had a reduced risk. Therefore, it can be stated that the blood type is the factor affecting the severity of the illness and patients’ mortality rate, of course, the gender is other important factor affecting the mortality, so that males presented shorter survival time. Our findings were consistent with previous studies on the topic from worldwide.50,57 In a seroepidemiology study by Rouhanizadeh et al., blood samples of 1504 people were taken and IgG and IgM antibodies were checked by ELISA test and the blood group of the people was determined. The frequency of positive IgG among people of blood group A, B, AB, and O was 12.7, 11.8, 9.4, and 9.6%, respectively. After adjusting the effect of variables suspected of confounding, the chance of contracting COVID-19 based on serological results (IgG+/IgM+) with a 95% confidence interval were as follows: in people of blood group A (1.19; 95% CI=1.67–0.85), blood group B (1.33; 95% CI=0.94–1.87), AB blood group (0.82; 95% CI=0.44–1.55), and O blood group (0.70; 95% CI=0.50–0.98). The chance of getting a COVID-19 infection in people with blood group O is significantly lower by 30% compared to other blood groups. Therefore, it can be stated that blood type O is probably a protective factor against COVID-19.56 Also, in a live meta-analysis by Pourali et al., the pooled frequency of blood groups A, B, O, and AB among people following COVID-19 was estimated to be 36.22%, 24.99%, 29.67%, and 9.29%, respectively. The frequency of blood groups A, B, O, and AB among the patients who expired following COVID-19 was estimated to be 40%, 23%, 29%, and 8%, respectively. The odds ratio of contracting COVID-19 for blood group A compared to other blood groups was estimated to be 1.16 (95% CI: 1.02–1.33). These values for blood groups O and AB compared to other blood groups were estimated as 0.73 (95% CI: 0.88–0.60) and 1.25 (95% CI: 0.84–1.86), respectively. Overall, people with blood type A are at a higher risk of contracting COVID-19, while people with blood type O are at a lower risk.58 The results obtained from this study were consistent with a study by Rouhanizadeh et al.56
The severity of SARS-CoV-2 infection might be predictable according to the patients’ blood group. Unfortunately, ABO distributions among hospitalized cases with COVID-19 than those hospitalized with non–COVID-19-related conditions could not be investigated due to lack of data.59 In addition, ABO distributions were not evaluated among the infected survivors and the deadly cases, as such, we could not be extrapolated or deliberated if a particular blood group was related to the mortality or other non–COVID-19 disorders.59 Evidently, these findings have also been established in other studies that carriers of blood group O+ had a lower risk and 35% lower severity of infection,60 which has been attributed to the angiotensin-converting enzyme5 activity and anti-A and -B antibodies.60 The ABO blood group has been reported to associate with the ACE activity and ACE inhibitor-induced cough amongst Chinese patients with hypertension and is mainly related to the GATC haplotype of the ABO gene with 4 polymorphisms (rs8176746, rs8176740, rs495828, and rs12683493).61,62 In so doing, a lower ACE level has been detected in serum of O blood type carriers as well as higher interleukin 6 (IL-6) levels.63 In the study of Guillon et al., it was reported that binding of spikes protein (S form) of SARS-CoV-2 to ACE2 can be inhibited by natural anti-A antibody, and in fact, natural anti-A and anti-B antibodies in carriers of blood group O can potentially bind and block the interaction between the viral spike proteins and the target cells’ receptors to prevent viral attachment to host cells or to act through the opsonization.64,65 Another aspects in modulating COVID-19 infection in terms of ABO blood group system is the host transmembrane protease serine subtype 2 as an important protective factor.66
In addition, it has been suggested that blood type O had advantages in maintaining of ACE2 activity followed by reduction in the risk of improving hypertension.67 Therefore, it can be concluded that the developing hypertension in our studied cases, which mostly had blood group type A+, can be mainly due to the higher ACE activity related to the GATC haplotype. In addition, Zhao et al. demonstrated an association between blood types and COVID-19 risk with a superior proportion of A and an inferior proportion of O blood types amongst the patients.1 Likewise, based on a meta-analysis from Italy and Spain, a higher risk of COVID-19 was observed among the blood type A than a lower risk among O blood type.25 The reason for the difference between the prevalence of blood groups in this study and other studies is probably due to the fact that, we evaluated only hospitalized patients and those who underwent blood group testing during hospitalization. Among the other findings of the present study was the relationship between gender and mortality, which has been realized in other studies. One of the important factors in females’ mortality rate involved by COVID-19 may be linked to the stronger innate and specific immune system in females, the escape from inactivation of the X chromosome in the areas of genes related to the immune system and the strengthening effect of estrogen on female's immune system.68
In conclusion, it was found that the most common blood group among hospitalized patients was O positive blood group compared to the A positive blood group. Cases with O positive blood group had significantly less disease severity and survived longer, and people with A positive blood group had significantly higher disease severity and mortality rate. Therefore, it seems that natural antibodies against A and B have a protective effect in patients with COVID-19 disease and they might be applied in the treatment of COVID-19 in the future. Certainly, it is felt necessary to conduct more studies, especially clinical trials with a larger sample size to pave the way for discovering the underlying molecular aspects which make individuals more or less susceptible to improving severe SARS-CoV-2.
FundingThere is no funding for the present study.
Ethical considerationThe study is approved by ethics committee of Iran University of Medical Sciences (IR.IUMS.REC.1401.488). All authors read and approved the study. Written informed consent received from participants.
We are grateful to Dr Kamran Aghakhani and Dr. Atefeh Gurjizadeh.