Colorectal cancer (CRC) is one of the leading causes of death and comprises a considerable percentage of cases presented with metastases. Herein, we report 81 yr-old female patient who was admitted to our clinic due to persistent nausea and vomiting. She had an eight years-history of colorectal cancer, and she had undergone a right hemicolectomy and received adjuvant capecitabine treatment. An incisional hernia was palpated around the umbilicus and confirmed by abdominal CT (computed tomography). Whole-body PET (positron emission tomography) revealed FDG (fluorodeoxyglucose)-enhanced lesions in the lungs, pancreas, and small bowel, suggesting metastases. Colonoscopy did not reveal any recurrence. Biopsies obtained from the pancreas with endosonography diagnosed colorectal cancer metastasis. During hospitalisation she has been operated due to ileus and the obstructed jejunal segment was resected. Histopathological examiation confirmed intestinal metastasis of the colorectal cancer. In conclusion, pancreas and small bowel metastases are both rare phenomena individually. Ileus caused by intestinal metastasis is also exceptional. The coexistence of these rare metastases and lung metastases in CRC can be related to the unique biologic behavior of this tumor.
El cáncer colorrectal (CCR) es una de las principales causas de muerte y comprende un porcentaje considerable de casos que se presentan con metástasis. Presentamos el caso de una paciente de 81 años que ingresó en nuestra clínica por presentar náuseas y vómitos persistentes. Tenía antecedentes de cáncer colorrectal de ocho años de evolución, había sido intervenida de hemicolectomía derecha y recibía tratamiento adyuvante con capecitabina. Se palpó una hernia incisional alrededor del ombligo y se confirmó mediante TC abdominal (tomografía computarizada). La PET (tomografía por emisión de positrones) de cuerpo entero reveló lesiones realzadas con FDG (fluorodesoxiglucosa) en los pulmones, el páncreas y el intestino delgado, lo que sugiere metástasis. La colonoscopia no reveló ninguna recurrencia. Las biopsias obtenidas del páncreas con endosonografía diagnosticaron metástasis de cáncer colorrectal. Durante su hospitalización ha sido operada de íleo y se le resecó el segmento de yeyuno obstruido. El examen histopatológico confirmó la metástasis intestinal del cáncer colorrectal. En conclusión, las metástasis de páncreas e intestino delgado son fenómenos raros individualmente. El íleo causado por metástasis intestinales también es excepcional. La coexistencia de estas raras metástasis y metástasis pulmonares en CCR puede estar relacionada con el comportamiento biológico único de este tumor.
CRC is the third most common cancer and the second most common cause of death related to cancer. CRC-related mortality decreased considerably over the years due to screening programs and the development of new treatment modalities. Almost 20% of patients have distant metastasis at the time of presentation and hematogenous and lymphatic dissemination are responsible for most of them1. Although the regional lymph nodes, liver, lungs, and peritoneum are the major sites of metastases, pancreas and small intestine metastases were rarely reported in the literature. Moreover, Secondary malignancies of the pancreas caused by metastases constitute an extremely small proportion (2-5%) of all pancreatic neoplasms. While renal cell carcinomas are the most common neoplasms (62,6-70%) that metastasize to the pancreas, CRC is responsible for a minority of cases (6,2-8,8%)2. Small intestinal metastases of CRC are accepted as a late complication of this disease and its incidence makes up 6% of all small intestinal tumors3,4. To our knowledge, this case is the first reported case of presenting with recurrence with metastases in the lung, pancreas, and small intestine.
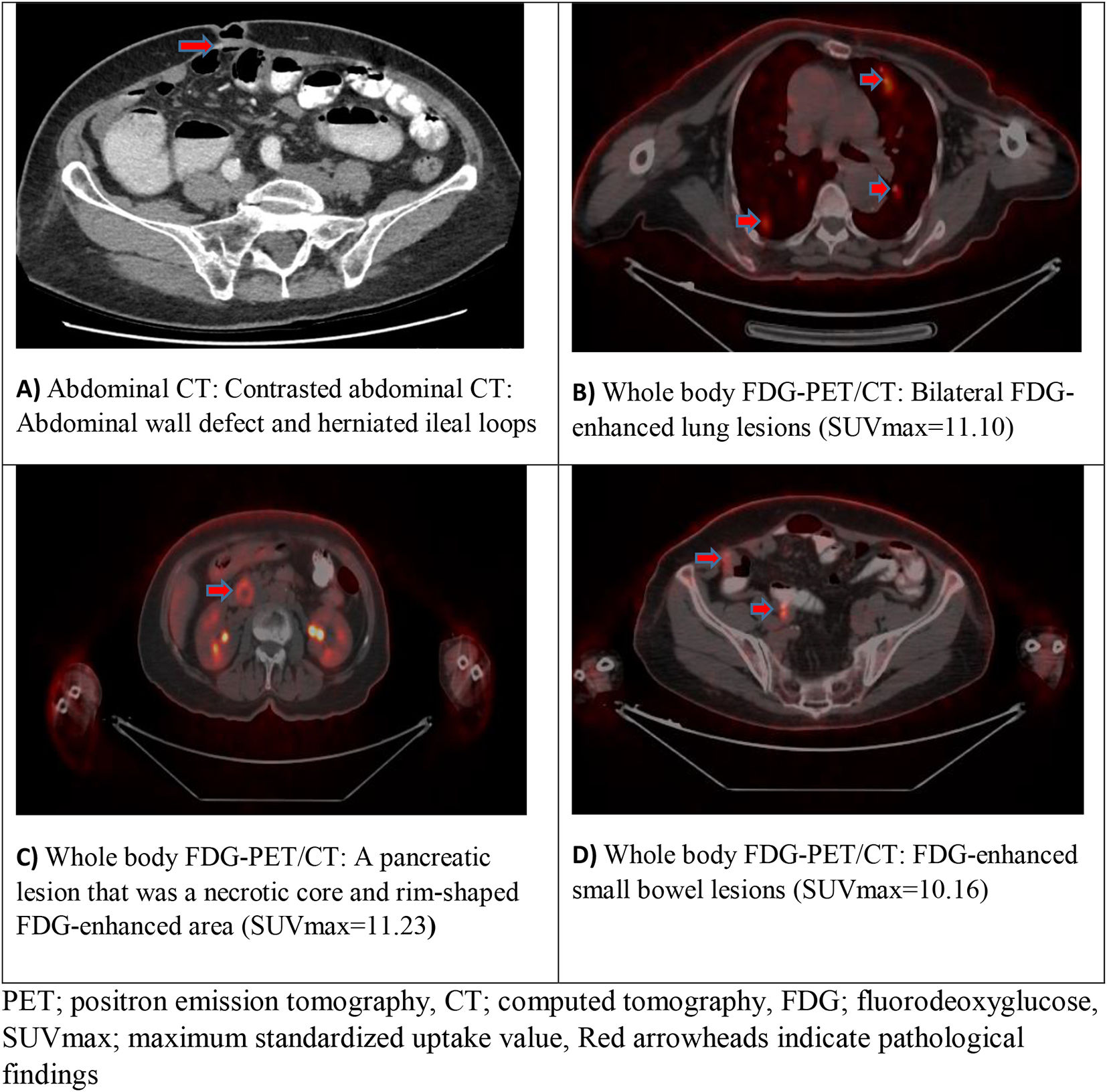
Case presentation81 yr-old female patient was admitted to our clinic with the complaints of persistent nausea and vomiting lasting for 3 months. On admission, the patient's vital signs were within normal ranges. An incisional hernia beneath the umbilicus was detected on palpation, and there was no organomegaly or lymphadenopathy. The past medical history revealed that the patient was treated for hypertension, and she had undergone a right hemicolectomy and ileotransversostomy operation due to 3-5 cm locally advanced (T3N1M0) CRC 8 years ago. Histopathologically, the tumor had been moderately differentiated (G2) and invaded the vascular and neural structures. So the patient had received adjuvant chemotherapy with capecitabine for 7 months. The laboratory tests on admission were as follows: Hgb: 11.4 g/dl (NR:12-16 g/dl), MCV: 75.4 f. (NR: 80-99 fl), MCH: 24 pg (NR: 22.2-33.5 pg), MCHC: 31.7 g/dl (NR: 32-36 g/dl), RDW 17% (NR:12-15%), CRP: 7.3 mg/dl (NR: <5 mg/dl), CEA: 2.09 ug/L (NR: <5 ug/L). A contrasted abdominal CT scan showed a hypointense lesion at the head of the pancreas, and its size was 20x18 mm. There were also multiple lesions at the basal segments of the lungs suggesting metastases. There was a fascial defect of 2 cm diameter at the right side of the umbilicus, ileal loops protruded from this defect, and proximal loops were dilated (diam: 4,5 cm), distal loops were collapsed (Fig. 1A). Although the intraluminal passage was slow, it was detactable. Thus, the treatment of small bowel obstruction was started: the patient's oral intake was stopped, a nasogastric tube was placed, and parenteral nutrition was started. A whole-body PET scan revealed multiple FDG-enhanced lung lesions (SUVmax=11.10) (Fig. 1B) and a pancreatic lesion that was a necrotic core and rim-shaped FDG-enhanced area (SUVmax=11.23) (Fig. 1C). There were also some lesions in the small intestine showing pathologic FDG enhancement (SUVmax=10.16) (Fig. 1D). Upon these findings, an endosonography-assisted fine-needle aspiration biopsy (FNAB) was obtained from the pancreatic lesion. Immunohistochemical examination of the biopsy specimen showed CDX2 (+), cytokeratin 7 (focal +), cytokeratin 20 (+), MUC1 (+), MUCSAC (focal+), MUC2 (-). Therefore, CRC metastasis was considered, and colonoscopy was performed. There was no polyp or mass lesion on colonoscopy, the area of anastomosis was normal. Because the patient's condition deteriorated despite non-surgical approach for small bowel obstruction, laparotomy was performed to repair the hernia. During the operation, a mass lesion in the outpouching small intestine was discerned and the involved jejunal segment was resected. Histopathologic examination of resected material showed CRC metastasis with lymphovascular and perineural invasion. Surgical borders were clear, and metastasis was detected in 2 of the 3 lymph nodes removed. After the surgery, the patient's performance status improved from ECOG (Eastern Cooperative Oncology Group) 4 to 2, and her oral intake increased. So that, the patient became eligible to receive chemotherapy, and the FOLFOX regimen (5-fluorouracil, folinic acid, and oxaliplatin) was planned with medical oncology department.
DiscussionThere were a few cases regarding small bowel metastasis in the literature. Stamopoulos et al. reported a case of intraluminal rectal cancer metastasis to the small bowel5. A 71 yr-old male patient who had a past medical history of anterior resection due to rectosigmoid cancer was diagnosed incidentally during the laparotomy for the repair of incisional hernia at the 6-month postoperative follow-up. Unlike our case, the patient had not shown the symptoms/signs of intestinal obstruction. PET confirmed local recurrence, and the patient underwent colonoscopy and endoscopic biopsy of the lesion, which was positive for adenocarcinoma. As in our case, the immunohistochemical staining pattern was compatible with CRC, in which strong positive staining for anti-cytokeratin 20, focal positive staining for anti-cytokeratin 7. He received adjuvant chemotherapy (FOLFIRI + bevacizumab) followed by tomotherapy-based image-guided radiotherapy5. Thoma et al. reported three cases of metastatic CRC to the small bowel, which presented with obscure gastrointestinal bleeding4. Like our case, all of those patients had low hemoglobin levels upon admission. Therefore, our patient's anemia, which improved after the operation, may be associated with obscure and intermittent bleeding from small bowel metastases4.
Although the vast majority of pancreatic cancer originates from the pancreas, some extrapancreatic cancers can also metastasize to the pancreas, and CRC makes up just a small proportion of them. Bachmann et al. reported two cases of recurrent rectum cancer presented with pancreas metastasis6. Unlike our case, which was diagnosed by FNAB, both cases underwent distal pancreatectomy. Moreover, both patients had elevated CEA levels at presentation. The first patient was 61 yr-old woman who had a past medical history of low anterior resection that had been performed two years before presentation for a poorly differentiated (G3) rectal adenocarcinoma. The patient had received neoadjuvant radiotherapy, and no adjuvant treatment had been administered. The patient was complaining of abdominal pain in the left upper quadrant. An abdominal CT scan showed a cystic structure in the pancreatic tail. Although FNAB had been tried, the cytopathological analysis showed only necrotic tissue. Presumably, the localization of the lesion influenced the diagnostic ability of FNAB. Since the lesion was located in the head of the pancreas in our case, we were able to perform FNAB with high diagnostic accuracy. As in our case, no signs of local recurrence were observed in colonoscopy. However, tumor markers CA 19-9 and CEA were elevated. Finally, the patient underwent a distal pancreatectomy. Similar to our case, immunohistochemically, the tumor cells showed expression of cytokeratin 20 and CDX2. The second patient was a 64 yr-old woman in good general condition who had been operated on for rectal cancer two and a half years ago and subsequently received chemoradiotherapy. Histological examination at that time had shown a moderately differentiated (G2) adenocarcinoma. The patient presented with elevated CEA, and magnetic resonance imaging showed hypodense structures in the pancreatic body/tail. A tumor of approximately 5 cm was found in the body/tail of the pancreas in the surgical exploration. Thus, distal pancreatectomy with splenectomy was performed. As in our case, immunohistochemically, the moderately differentiated tumor cells were positive for cytokeratin 20 and CDX26.
To date, underlying mechanisms of tissue tropisms of cancer metastasis remain to be fully elucidated. However, it has been shown that chemokines and their cognate receptors play critical roles in cancer behavior7. Their altered expression in malignancies dictates leukocyte recruitment and activation, angiogenesis, cancer cell proliferation, and metastasis7. Since most of the previous cases were recurrent cancers, their alterations in recurrent CRC may have affected the tissue tropisms of metastases and have led to metastases in atypical localizations as in our case.
There have been several proposed predictors for distant metastasis in CRC. Guo et al. found that CEA, histopathological grade, N classification, age at diagnosis, and tumor size were significant risk factors for T1 cancer8. According to this study, patients aged 65-79 had a significantly lower risk for distant metastasis than patients aged 18-49. In other parameters, a high score was a risk factor8. Emile et al. suggested that being younger increases the risk of distant metastasis in mucinous CRC9. On the other hand, they found that the female sex and T4 tumors were significant predictors for distant metastasis9. An umbrella review showed that vascular invasion is the only risk factor convincingly classified for lymph node metastasis in pT1 tumors10. Understandably, most of the studies have been performed to reveal the risk of distant metastasis in earlier stages. However, we consider that some features of the primary tumor may be related to recurrence with distant metastasis in our patient: invasion (neurovascular), stage (T3N1M0), grade (G2), tumor size (≥ 3 cm) and patient's gender (female).
ConclusionsThe development of novel treatment strategies for CRC prolonged the life expectancies of most patients. Thus, these tumors had the opportunity to exhibit manifestations not previously reported in the literature. CRC that presented with both pancreas and small bowel metastases is an extremely rare situation. However, this potentially will lead to changes in our understanding of tumor pathogenesis and behavior, especially in recurrent cancers.
Ethical considerationsWritten informed consent was received from the patient for publication
Conflict of interestThe other authors declare no competing interests.
FundingNo funding was received.
Consent to participateNot applicable
Conset of the patientWritten informed consent for publication was received from the patient
Consent for publicationApplicable
Availability of data and materialNot applicable
Code availabilityNot applicable
Author ContributionsTumay Ak followed the patient and wrote the manuscript. Mehmet Copur and Selcuk Candan followed the patient. Selcuk Candan and Ali Ibrahim Hatemi helped establish the general message of the manuscript and contributed to the design of the manuscript. Tumay Ak, Mehmet Copur, Selcuk Candan, and Ali Ibrahim Hatemi provided critical review, integrity, and clarity to the manuscript. All authors discussed the conclusions and contributed to the final version of the manuscript.
The authors would like to thank Cerrahpasa Medical Faculty Department of Nuclear Medicine and Radiology for their contributions with radiologic images of the patient.