Allergic rhinitis is a common disorder. Intranasal corticosteroid sprays are used to control symptoms. However, incorrect use of these sprays can decrease efficacy and lead to side effects such as nose bleeding. We studied if watching an age-adjusted instruction video is effective to improve administration technique.
Materials and methodsWe invited children who used intranasal corticosteroid sprays. We examined their administration technique before, directly after, and one month after showing them an age-adjusted instruction video. We compared their administration technique with the instructions in the patient information leaflet. We assessed whether the children performed the seventeen maneuvers mentioned in the patient information leaflet and the eight we considered essential.
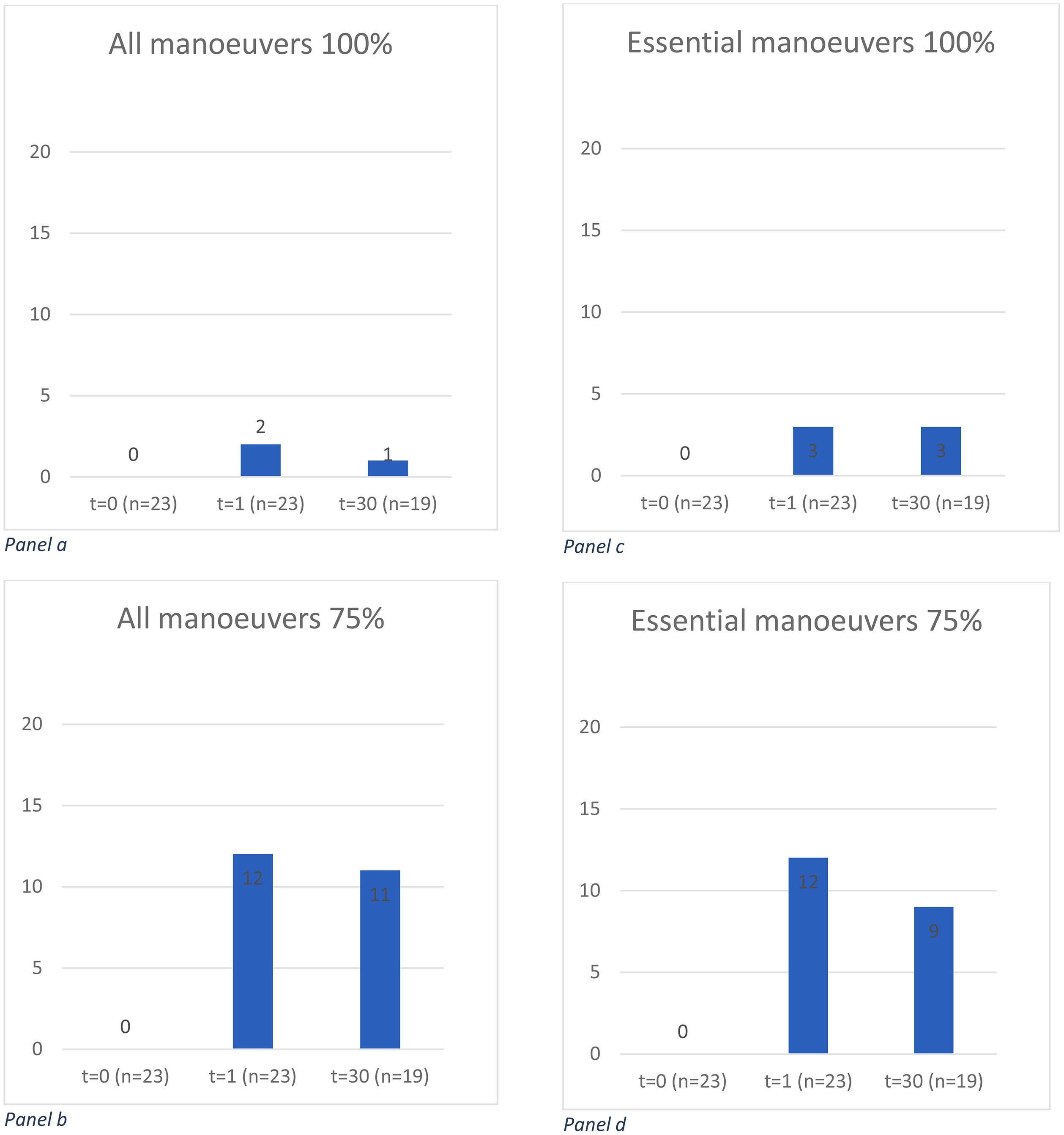
ResultsOf the 99 eligible children, 23 (15 boys, median age nine years) participated. Before watching the instruction video none of them administered according to all maneuvers in the patient information leaflet or showed all essential maneuvers. One month after seeing the instruction video, three children demonstrated correct inhalation as per the patient information leaflet. Three performed the essential maneuvers. When a 75% threshold level for carrying out all 17 maneuvers was used, still none showed 75% of all or of the essential maneuvers before watching the video. Yet, after one month 12 children showed sufficient administration technique (52%, 95% confidence interval (CI) 31%–73%, p = 0.004). Nine showed all essential manoeuvres (47%, 95%CI 24%–71%, p = 0.004).
ConclusionsAn age-adjusted instruction video is a useful and easy method to teach children to administer nasal intranasal corticosteroid sprays correctly.
Allergic rhinitis is a common disease, affecting about 10% of children in Western countries.1 Allergic rhinitis and allergic asthma often occur simultaneously in the same patient and improvement of allergic rhinitis leads to improved asthma control.2 Allergic rhinitis can be treated with systemic and intranasal antihistamines and corticosteroids. For an optimal effect, correct administration of intranasal corticosteroids (INCS) is paramount. Incorrect use of INCS is associated with less efficacy and more adverse effects such as nose bleeding.3 Contrarily to the quality of inhalation technique of inhaled corticosteroids in asthma, the quality of applying INCS has not been studied extensively.
Recently, we studied the administration technique in a group of children and adults and found that only 11% of the patients administered the INCS according to the instructions in patient information leaflets (PILs). Blowing the nose is important to enhance deposition of the spray on the mucosa. We found that 48% of the patients did this correctly. To prevent nose bleeding, it is advised to point the end of the nozzle slightly outwards and away from the septum. This was done by 44%. When patients exhale through the nose the spray is blown out. To prevent this, it is advised to exhale through the mouth and about half of the patients did this correctly.4
Therefore, we decided to make an instruction video for the use of INCS, aimed at children of eight to 12 years of age. We studied whether watching this instruction video improved children’s administration technique of INCS directly and after one month.
Patients and methodsWe sought children aged eight to 12 years in the database of this large teaching hospital in the Northern part of The Netherlands, who had been prescribed INCS as outpatients and we invited them to participate. Children not fluent in Dutch or with physical or cognitive impairment, based on information in the medical records, were excluded. The local ethical committee waived this study. All participants and their caregivers gave written informed consent. Care was taken to protect patients’ privacy by processing the data anonymously.
After inclusion, the children were asked to demonstrate the administration of their INCS before, directly after watching the instruction video, and one month later. The technique demonstrated in the instruction video was based on information in the PILs and literature.3 The video was made by a director who is experienced in making television programs for children on national TV.
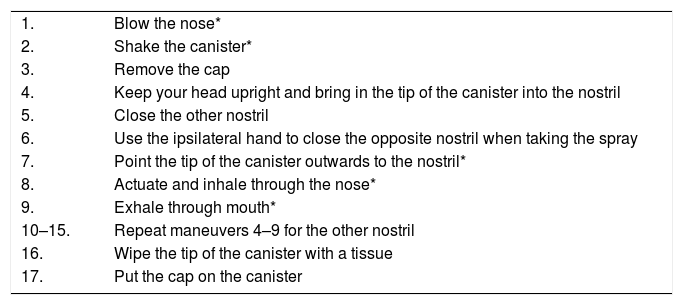
Participants were observed face-to-face or using streaming facilities such as FaceTime® or Skype® by the same observers. These observers were trained medical students. The administration technique was assessed in two ways. In the PIL we identified 17 maneuvers (Table 1), and we assessed if participants showed these. Secondly, based on literature and earlier experience, we made a list of eight maneuvers, which we deemed essential. By direct observation we assessed if the participants showed these (Table 1). Every maneuver was scored as carried out (1) or not (0). We studied if 100% and 75% of the maneuvers in the PIL or the essential maneuvers were carried out. We speculated that only a few children would carry out all maneuvers and therefore arbitrarily choose the 75% level. Thus, in the second (75% level) analysis we accepted a score of 13–17 of performing the maneuvers mentioned in the PIL and 6–8 of the essential maneuvers as sufficient.
All maneuvers as described in patient information leaflets for taking intranasal corticosteroid sprays.
| 1. | Blow the nose* |
| 2. | Shake the canister* |
| 3. | Remove the cap |
| 4. | Keep your head upright and bring in the tip of the canister into the nostril |
| 5. | Close the other nostril |
| 6. | Use the ipsilateral hand to close the opposite nostril when taking the spray |
| 7. | Point the tip of the canister outwards to the nostril* |
| 8. | Actuate and inhale through the nose* |
| 9. | Exhale through mouth* |
| 10–15. | Repeat maneuvers 4–9 for the other nostril |
| 16. | Wipe the tip of the canister with a tissue |
| 17. | Put the cap on the canister |
The items marked with an asterisk (*) are deemed essential.
The earlier study showed that about 11% of the patients administered the INCS correctly as described in the essential steps.4 We expected that one month after watching the instruction video, 54% of children would correctly use the INCS. Under the assumptions of using a McNemar test for paired proportions with the discordant pairs being 1% (correct before video - not correct after video) and 44% (not correct before video - correct after video), with a significance level of 5% and a power of 80%, at least 18 patients should be included (PASS, version 11, NCSS, LLC. Kaysville).
The basic characteristics of the study sample were described with median (range) and number (percentage), as appropriate. At each time point, the number and proportion (with 95% confidence interval based on the Clopper–Pearson method) of children sufficiently performing the maneuvers is given. To assess whether watching the video improved the proportion of children correctly using the inhalator for INCS, a McNemar test for paired proportions was used. All analyses were performed with SPSS (version 26, IBM Corp. Armonk, NY, USA). We considered p-values < 0.05 statistically significant.
ResultsA total of 99 children were eligible for this study and 23 of them consented to participate. Due to several reasons, such as no time or forgotten to participate, 19 of them joined the last assessment after one month. The median age was nine years (eight to 12 years) and 15 participants (65%) were boys. The indication for use of INCS was allergic rhinitis in all.
None of the children showed a correct administration technique before watching the instruction video, assessed in either way (Fig. 1). Directly after seeing the video, only two of them carried out all maneuvers (9%; 95% confidence interval (CI) 1%–28%), mentioned in the PIL, and three showed all essential maneuvers. After one month, only one child carried out all maneuvers (5%; 95%CI 0%–26%) and three exhibited all essential maneuvers (13%; 95%CI 3%–34%). When the threshold for sufficient administration was laid on exhibiting 75% of all and essential maneuvers, after one month 11 (58%;95%CI 34%–80%) and nine (47%; 95%CI 24%–71%) exhibited these respectively. Compared with the results before seeing the video, the differences between the results before seeing the instruction video and after one month are statistically significant.
Proportions of the 23 children who fulfilled the criteria for sufficient administration of nasal corticosteroids.
Panel a: number of children showing 100% of all maneuvers before, directly after, and one month after watching the instruction video.
Panel b: number of children showing 75% of all maneuvers before, directly after, and one month after watching the instruction video. The difference between t = 0 and t = 30 is statistically significant (p = 0.001)
Panel c: number of children showing 100% of the essential maneuvers before, directly after, and one month after watching the instruction video.
Panel d: number of children showing 75% of the essential maneuvers before, directly after, and one month after watching the instruction video. The difference between t = 0 and t = 30 is statistically significant (p = 0.004).
In this study of the use of INCS for allergic rhinitis, aimed at children of eight to 12 years of age, we found that none of the patients took their INCS correctly before seeing the instruction video. One month after seeing the instruction video, specifically aimed at this age group, the number of children showing the correct administration technique increased.
In an earlier study we found that only four of 64 patients (6%) inhaled the medication according to all instructions in the PIL and only seven (11%) showed all maneuvers considered essential.6 Obviously, correct administration of INCS spray is difficult to do.
In recent years much attention has been given to the correct inhalation technique of inhaled corticosteroids in asthma.5 Incorrect administration of inhaled corticosteroids is associated with less asthma control. Compared with the interest in inhalation technique in asthma, data on the correct administration for INCS is scarce. However, incorrect use of INCS could lead to lower efficacy and more side effects.3 Probably one of the reasons for this difference in interest for inhalation technique in asthma and allergic rhinitis is that the effects of insufficient administration of INCS are more difficult to establish. Insufficient inhalation of asthma medication influences firm outcome measures such as lung function, use of betamimetics, and exacerbations. For incorrect use of intranasal steroids, such outcome measures are not readily available. Moreover, there is no consensus on the correct administration technique of INCS. Also, in earlier studies in The Netherlands as well as in the United Kingdom, we found that PILs are not uniform and incomplete.6 Benninger et al. reviewed the literature on studies assessing the correct use of intranasal steroids.3 Based on their study, we identified essential maneuvers.
We found only one study on methods to improve the administration of INCS in children. That study showed that the combination of a cartoon with a verbal explanation was successful.7 However, in this study the administration technique was assessed immediately after instruction. Whether the successful instruction retains for a longer period remains uncertain.
In asthma, Arumugom et al. compared the effect of a video instruction of taking asthma medication in children with a verbal explanation. They found that children who had seen the video inhaled their medication significantly better in comparison with the verbal instruction, even after one month.8 Comparably, Shah found that watching instruction videos was more effective than reading written instruction in adults.10 Shaw et al. found that using instruction videos enhances the inhalation technique of pulmonary medications in asthmatic children.9 Whether the beneficial effects of the instruction video remain after one month and results in better clinical efficacy and less adverse effects, such as nose bleeding in children with allergic rhinitis, remains to be elucidated.
This study has some limitations. First, the number of participants was lower than expected, so only about a quarter of the patients invited were included. However, we do not think that the children who did not participate administer their nasal sprays better. Also, we did not check the clinical efficacy. Clinical improvement is a result of many steps, including medication adherence, effective administration technique, avoidance of allergens and irritants. Because we learned from earlier studies that the administration technique was insufficient in many patients, we aimed to study this first.
In conclusion, we showed the beneficial effects of an age-adjusted instruction video on administering INCS in children, at least after one month. This is an easy-to-use method to teach children to take INCS correctly.
Further studies should elucidate whether these beneficial effects remain in the longer term. These studies should also reveal whether the improvement in successfully using the INCS results in beneficial clinical responses, and whether the intervention effect is similar in subgroups.
Conflict of interestThe authors have no conflict of interest to declare.
We thank Eric Blom for production of the instruction video.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.