American cockroach is a common aeroallergen sensitization in allergic rhinitis (AR) patients. Association between skin prick test (SPT) and specific immunoglobulin E (sIgE) to American cockroach allergen remains uncertain. This study aimed to evaluate the association between SPT and sIgE to American cockroach allergen in patients with AR.
Materials and methodsThis cross-sectional study was conducted in Thai AR patients aged 6–25 years from September 2013 to October 2014. SPT and sIgE to American cockroach allergen were performed and the correlation was calculated using SPSS Statistics version 18.
ResultsSixty-seven AR patients, with median age of 15 years were included in this study. SPT and sIgE to American cockroach allergen showed a positive result in 68.7% and 58.2% cases, respectively. Positive SPT or positive sIgE to American cockroach was found in 79.1%. Thirty-two patients (47.8%) tested positive for both SPT and sIgE to American cockroach allergen. Fourteen from a total of 67 cases (20.9%) with negative sIgE had positive SPT to American cockroach, while seven cases (10.4%) with negative SPT had positive sIgE to American cockroach. Moderate correlation was observed between mean wheal diameter (MWD) and sIgE level to American cockroach (r=0.465, p=0.001). No significant correlation was found between MWD of SPT or sIgE level to American cockroach and AR severity.
ConclusionA moderate correlation was observed between MWD of SPT and sIgE level to American cockroach. If SPT is negative in allergic rhinitis patients highly suspected of having American cockroach allergy, serum sIgE should be considered and vice versa.
Allergic rhinitis (AR) is a health problem that affects millions of people around the world. The prevalence of AR was reported to have risen to 38% in the Thai population.1 AR is not life-threatening, but it adversely affects daily activity and quality of life — especially sleep patterns. Diagnosis of AR is based on clinical manifestations and positive specific immunoglobulin E (sIgE) reaction to antigen.2 Skin prick test (SPT) or serum sIgE is performed to identify the causative aeroallergens. The most common aeroallergen sensitization in Thai AR patients (adults and children) is house dust mites (89.1%).3,4 The second most common allergen is cockroach (50.9%).3,4 SPT is the diagnostic test used to evaluate IgE-mediated reaction. In the hands of a specialist, SPT is inexpensive, safe, and easy. However, SPT is insufficiently accurate in young infants and it has some limitations in patients with skin lesion at the test area and in patients who cannot stop taking antihistamines for symptom control. The measurement of sIgE in serum is another way to evaluate IgE reaction. This method is more expensive and takes longer to perform, but it can be performed in young infants, in patients with skin lesion, and in patients who cannot stop taking antihistamine. A previous study showed that symptom severity had the highest odds ratios (OR) associated with decision to perform sIgE measurement in AR patients (OR: 12.11, 95% CI: 7.1–20.7).5
A previous study in 158 AR patients reported the accuracy, sensitivity, and specificity of the ImmunoCAP system to be 0.810, 0.819, and 0.872, and the same parameters for SPT to be 0.780, 0.741, and 0.862, all respectively.6 The accuracy was similar between the two systems (p>0.05), but the ImmunoCAP had higher sensitivity and SPT had higher specificity.6 The association between SPT and sIgE to American cockroach antigen has not been previously evaluated in Thai patients with AR.
The most common allergy-causing cockroach in Thailand is the American cockroach (Periplaneta americana), followed by the German cockroach (Blatella germanica).7 The American cockroach accounts for approximately 60–70% of all cockroaches with Per a 9 being identified as a major allergen in Thailand.7–9 Among AR patients in Thailand, 40–60% of cases showed positive SPT to American cockroach.10 In a previous study, a very high degree of IgE-mediated cross-reactivity between allergens derived from American and German cockroach was demonstrated.11 Furthermore, earlier studies demonstrated the 52–72% identity of amino acid sequence among Bla g 1 and Per a 1.12,13
The objective of this study was to evaluate the association between SPT and sIgE to American cockroach allergen in Thai patients with AR. Correlation between AR severity and mean wheal diameter (MWD) of SPT and between AR severity and level of serum sIgE to American cockroach were also studied.
Materials and methodsThis cross-sectional study was conducted from September 2013 to October 2014. Patients between the age of 6-25 years with physician-diagnosed AR were included to the study. The protocol for this study was approved by the Siriraj Institutional Review Board (SIRB), Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand. Written informed consent and/or assent was obtained from patients and/or guardians prior to inclusion.
Allergic rhinitis was diagnosed when a patient had symptoms of rhinorrhea, sneezing, itchy nose and/or eyes, or nasal congestion together with clinical signs, such as allergic shiner, adenoid face, or swollen and pale inferior nasal turbinate.2 Severity of AR was classified as mild intermittent, mild persistent, moderate to severe intermittent, or moderate to severe persistent, according to Allergic Rhinitis and its Impact on Asthma (ARIA) guideline.2 Included patients had no other systemic diseases, severe skin diseases, severe and uncontrolled allergic diseases, or pregnancy. Clinical characteristics of patients were collected and recorded. SPT to American cockroach antigen (ALK-Abello, Port Washington, New York, USA) was performed at the patient’s back after antihistamine and local and systemic corticosteroid (more than 20mg/day) were discontinued for at least seven days. Buffered saline and 10mg/mL histamine dihydrochloride were used as negative and positive controls, respectively. A MWD of more than 3mm at 15min after SPT was interpreted as positive SPT. Specific IgE to American cockroach, measured by ImmunoCap (UniCAP 100; Instrument Pharmacia Diagnostic AB, Uppsala, Sweden), was concurrently performed. Specific IgE was interpreted as positive when the level was >0.35kUA/L.
Statistical analysisAll statistical analyses were performed using SPSS Statistics version 18 (SPSS, Inc., Chicago, IL, USA). Correlation between MWD and level of sIgE was calculated using Spearman’s rank correlation coefficient. Linear correlation between MWD and level of sIgE was calculated using linear regression analysis. Patient demographic and clinical characteristics are presented as number and percentage. MWD severity data are given as mean±standard deviation (min, max). A p-value <0.05 was regarded as being statistically significant.
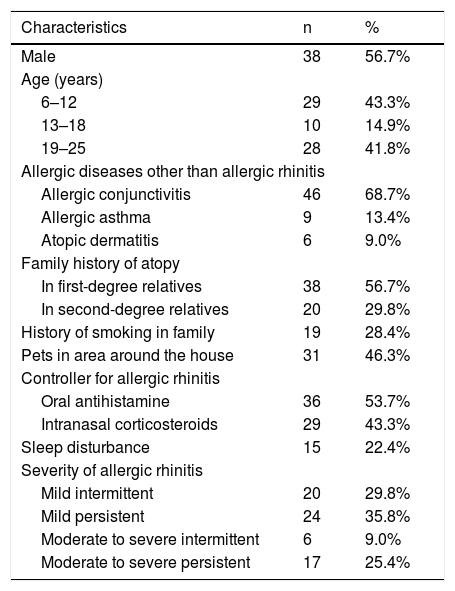
ResultsSixty-seven AR patients were included in this study. Median age of patients was 15 (range: 6–25) years and 38 of them (56.7%) were male. The most common age group was 6–12 years (43.3%), followed by 19–25 years (41.8%). Allergic conjunctivitis was the most common associated allergic disease (68.7%), followed by allergic asthma (13.4%), and atopic dermatitis (9%). Mild persistent AR (35.8%), and mild intermittent AR (29.8%) were the most common severity that were found. Intranasal corticosteroid was used in 43.3% of cases. Sleep disturbance was reported in 22.4% of cases. Demographic and clinical characteristics are shown in Table 1. Four AR patients with American cockroach sensitization had a history of seafood allergy.
Demographic and clinical characteristics of the study population (N=67).
| Characteristics | n | % |
|---|---|---|
| Male | 38 | 56.7% |
| Age (years) | ||
| 6–12 | 29 | 43.3% |
| 13–18 | 10 | 14.9% |
| 19–25 | 28 | 41.8% |
| Allergic diseases other than allergic rhinitis | ||
| Allergic conjunctivitis | 46 | 68.7% |
| Allergic asthma | 9 | 13.4% |
| Atopic dermatitis | 6 | 9.0% |
| Family history of atopy | ||
| In first-degree relatives | 38 | 56.7% |
| In second-degree relatives | 20 | 29.8% |
| History of smoking in family | 19 | 28.4% |
| Pets in area around the house | 31 | 46.3% |
| Controller for allergic rhinitis | ||
| Oral antihistamine | 36 | 53.7% |
| Intranasal corticosteroids | 29 | 43.3% |
| Sleep disturbance | 15 | 22.4% |
| Severity of allergic rhinitis | ||
| Mild intermittent | 20 | 29.8% |
| Mild persistent | 24 | 35.8% |
| Moderate to severe intermittent | 6 | 9.0% |
| Moderate to severe persistent | 17 | 25.4% |
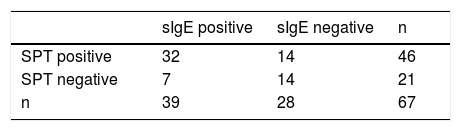
Forty-six cases (68.7%) had positive SPT and 39 cases (58.2%) had positive sIgE to American cockroach. Thirty-two patients (47.8%) showed positive result to both SPT and sIgE to American cockroach, and 14 patients (20.9%) showed negative result to both SPT and sIgE to American cockroach. Fourteen out of a total of 67 cases (20.9%) with negative sIgE had positive SPT to American cockroach, while seven cases (10.4%) with negative SPT had positive sIgE to American cockroach (Table 2). When SPT to American cockroach was negative, sIgE was positive in 33.3% (7/21 patients) of cases. When sIgE to American cockroach was negative, SPT was positive in 50.0% (14/28 patients) of cases. When SPT to American cockroach was positive, sIgE was negative in 33.3% (14/46 patients) of cases. When sIgE to American cockroach was positive, SPT was negative in 18.0% (7/39 patients) of cases. If we interpreted sensitization to American cockroach allergen as positive by either SPT or sIgE, sensitization was found in 53 cases (79.1%). Median size of the MWD of AR patients with positive SPT to American cockroach was 4.5 (range: 3–10.5)mm. Median level of sIgE to American cockroach was 2.8 (range: 0.48–62.3)kUA/L.
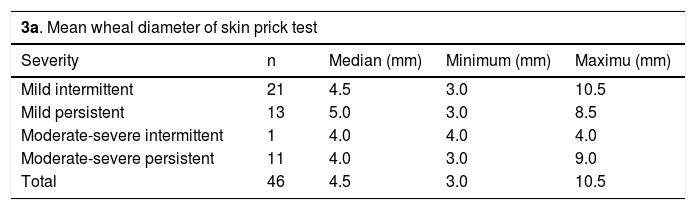
There were no significant differences between MWD size of SPT, and levels of sIgE to American cockroach and the four different severities of AR (Tables 3a, 3b). The maximum MWD of SPT to American cockroach was 10.5mm and the maximum sIgE level was 62.3kUA/L. There was moderate positive correlation between MWD of SPT and sIgE level to American cockroach (r=0.465; p=0.001)
Mean wheal diameter of skin prick test and levels of serum-specific IgE to American cockroach in different severities of allergic rhinitis.
| 3a. Mean wheal diameter of skin prick test | ||||
|---|---|---|---|---|
| Severity | n | Median (mm) | Minimum (mm) | Maximu (mm) |
| Mild intermittent | 21 | 4.5 | 3.0 | 10.5 |
| Mild persistent | 13 | 5.0 | 3.0 | 8.5 |
| Moderate-severe intermittent | 1 | 4.0 | 4.0 | 4.0 |
| Moderate-severe persistent | 11 | 4.0 | 3.0 | 9.0 |
| Total | 46 | 4.5 | 3.0 | 10.5 |
| 3b. Serum-specific IgE | ||||
|---|---|---|---|---|
| Severity | n | Median (kUA/L) | Minimum (kUA/L) | Maximum (kUA/L) |
| Mild intermittent | 13 | 2.80 | 0.93 | 62.30 |
| Mild persistent | 13 | 3.53 | 0.63 | 20.00 |
| Moderate-severe intermittent | 2 | 4.60 | 2.02 | 7.18 |
| Moderate-severe persistent | 11 | 1.49 | 0.48 | 19.00 |
| Total | 39 | 2.80 | 0.48 | 62.3 |
Slight male predominance was found in this study of AR patients aged 6–25 years. Allergic conjunctivitis was found in nearly 70% of patients, while asthma was found in 13.4% of cases. A previous study from Thailand reported asthma in 36% of AR children.14 In Western countries, the overall prevalence of asthma was reported to range from 10% to 40% in AR patients.2,15 Allergic rhinitis is normally diagnosed based on clinical symptoms. However, identification of the causative allergens facilitates improvement in AR symptoms via allergen avoidance and immunotherapy. The gold standard test for identifying causative allergens is intranasal allergen challenge test. This test is not commonly used in general practice, because it is time consuming, difficult to perform, and causes patient discomfort. Therefore, the most practical procedures for evaluating causative allergens in general practice are SPT and/or serum sIgE.
This study found moderate correlation between mean wheal diameter of SPT and level of serum sIgE to American cockroach (r=0.465; p=0.0001). A previous study reported very low agreement between SPT and sIgE to cockroach (kappa=0.17), and advised that diagnosis should be made only in patients with high sIgE and positive SPT.16 In addition, a previous study from Sookrung et al.17 reported low concordance between SPT and sIgE to cockroach using the same commercial allergen extracts as our study, and they suggested that sIgE to in-house ELISA, Per a 9 could be considered in order to diagnose cockroach sensitization among allergic rhinitis patients. A study from Kuwait18 showed some correlation between SPT and serum sIgE to cockroach in asthmatic patients (r=0.254), and found more cases with positive SPT (MWD>3mm) than positive sIgE (level >0.35kUA/L). Our study supported this result by showing more positive SPT than positive sIgE to American cockroach (68.7% vs. 58.2%, respectively). A study from Nigeria19 reported a different result. That study found a weak negative correlation between sIgE and SPT to cockroach (r=−0.084).
Most studies showed that SPT had higher sensitivity than sIgE.20,21 In clinical practice, the sensitivity of sIgE was 60–95%, and the specificity ranged from 30% to 95%.21 Based on comparative studies, the sensitivity of sIgE is approximately 25–30% lower than that of skin testing.21 Our study found the rate of positive SPT to be about 10% higher than the rate of positive sIgE (68.7% vs. 58.2% of cases). When SPT to American cockroach was negative, sIgE was positive in 33.3% of cases. When sIgE to American cockroach was negative, SPT was positive in 50.0% of cases. If we used positive SPT or sIgE as the criteria for cockroach sensitization, 79.1% of AR patients would have been shown as having cockroach sensitization. Patients who are highly suspected of cockroach allergy may require both SPT and sIgE to conclusively detect cockroach allergy.
In this study, four AR patients with American cockroach sensitization had coexisting seafood allergy. A previous study reported a high correlation between sIgE to shrimp and sIgE to cockroach in patients with positive sIgE to cockroach.22 This high correlation may be attributable to similarities in tropomyosins found in both shrimp and cockroaches.22,23
We found no correlation between MWD or sIgE level to cockroach and severity of AR. This may be due to the fact that the number of cases with moderate to severe intermittent AR was lower than the number of cases in the other groups, and that patients were also allergic to other allergens. We attempted to evaluate the association in the cases with mono-allergy to cockroach, but the number of cases was too small. Previous studies reported that the factors that influence severity of cockroach allergy are the volume of cockroach allergen exposure.24,25 and the age of the patient at the time of exposure.26 Early cockroach exposure (age <2 years) might increase proliferative response.26
The strengths of this study are that SPT was performed by an experienced technician and that sIgE measurement was performed in an accredited laboratory with ISO 15189:2012 and ISO 15190:2003 certification using ImmunoCap from the Bureau of Laboratory Quality Standards, Thailand Ministry of Public Health. This study also had some mild, but mentionable limitations. First, the age range of subjects was only 6–25 years. As such, important age groups, both younger and older than our study cohort, were not evaluated. Second, we limited our study to the American cockroach only. We did so because the American cockroach was found and reported to be the most common cockroach in Thailand and that it caused sensitivity in allergic Thai patients.3,4,7–10 Another reason that we chose to focus on the American cockroach only was because a very high degree of IgE-mediated cross-reactivity was reported between allergens derived from American and German cockroaches.11–13
In conclusion, we recommend that AR patients aged 6–25 years with suspected American cockroach allergy that have negative SPT or sIgE to American cockroach allergen should undergo both SPT and sIgE testing to confirm the causative agent.
Funding disclosureThis study was supported by a Research Development Fund and a Chalermprakait grant from the Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand and by NSTDA Chair Professor grant (P-1450624) funded by Crown Property Bureau.
Conflict of interestThe authors hereby declare no personal or professional conflicts of interest regarding any aspect of this study.
The authors gratefully acknowledge Mr. Suthipol Udompunturak for assistance with statistical analysis.