Asthma is such a heterogeneous concept that it proves difficult to clearly define. Patients with typical asthma are easy to diagnose by any experienced clinician, but when the condition is less typical, the limits become somewhat diffuse. In simplistic terms we could classify individuals into three theoretically excluding situations: no asthma; asthma; and other disorders that look like asthma but are not asthma. In the real world, however, things are not so clear.
What is the boundary between having asthma and not having asthma, between very mild asthma and no asthma? Some people may have mild or very infrequent symptoms (even only cough), which makes it difficult to establish whether they are asthmatic or not. Even when asthma is manifest in an individual, it is difficult to know when it started and whether the patient had unidentified mild symptoms before asthma became evident. Moreover, if the patient shows spontaneous improvement, as often happens during the pediatric stage of life, it is difficult to know whether remission is complete or only apparent, and whether the disease may appear again or not. Can a patient be considered asthmatic for life even if he/she is asymptomatic or has been in disease remission for many years?
At the other extreme, we can have difficulties distinguishing between severe or atypical asthma and other disease conditions. In elderly individuals this problem is particularly debated in relation to chronic obstructive pulmonary disease (COPD).1 In childhood, the differential diagnosis of asthma is very broad and must be considered when the asthmatic syndrome exhibits atypical features, a poor response to treatment, or proves particularly severe. However, more than one diagnosis may coexist in the same patient when the alternative diagnosis is unable to explain all the clinical manifestations and instead contributes to the atypical behavior of asthma (comorbidities).
Asthma is increasingly conceived of as a syndrome, i.e., as a series of signs and symptoms that are the manifestation of variable lower airway obstruction, with a presumed inflammatory substrate in most cases.2,3 Despite this relatively loose concept of asthma, many guides insist on the need to objectively demonstrate airflow lability or the presence of inflammation.2,4 Mallol et al., in a study published in the current number of Allergologia et Immunopathologia, once again question the usefulness of lung inflammation or function studies in confirming the diagnosis of asthma.5,6 Many asthmatic patients - understood as such when an expert physician diagnoses the disease on the basis of clinical criteria - exhibit characteristic lung function alterations, particularly bronchial hyperresponsiveness. However, a significant number of individuals (up to 10% in the study by Mallol et al.) yield normal results in all the lung tests. In this case, who establishes a wrong diagnosis: the professional who places priority on the clinical condition or the one that relies on objective testing? What diagnosis should be made in the case of a patient with even typical asthmatic syndrome but with normal lung tests? Is it a mistake to diagnose asthma in these cases? Many investigators believe the answer to be yes, and that the misdiagnosis rate is quite high when attempts are made to confirm the diagnosis using objective tests.7
Despite their objective nature, lung function tests are not without problems that must be taken into account. In addition to the technical aspects needed for correct testing to be performed, adequate patient cooperation is necessary, and this is not always possible. Moreover, the spirometric values may be normal in the more stable phases or remission periods of the disease. In contrast, the lung function alterations may reflect other different pulmonary disorders, or can simply correspond to variants of normal.
A population group that is particularly sensitive to this problem is young children, who because of their age are unable to undergo lung function tests requiring patient cooperation. A systematic review found that the clinical guides on asthma accept that the diagnosis could be established in preschool children based on clinical criteria.8 In agreement with the conclusions of Mallol et al., this viewpoint may be extended to other age groups, with a diagnosis of asthma being established in patients that meet the following three clinical criteria:
- •
Symptoms of bronchial obstruction, of a recurrent or fluctuating nature, evidenced by a physician.
- •
Marked variability of such symptoms, either spontaneously or with asthma treatment.
- •
The indicated symptoms cannot be fully explained by other disease conditions that can manifest in a similar way.
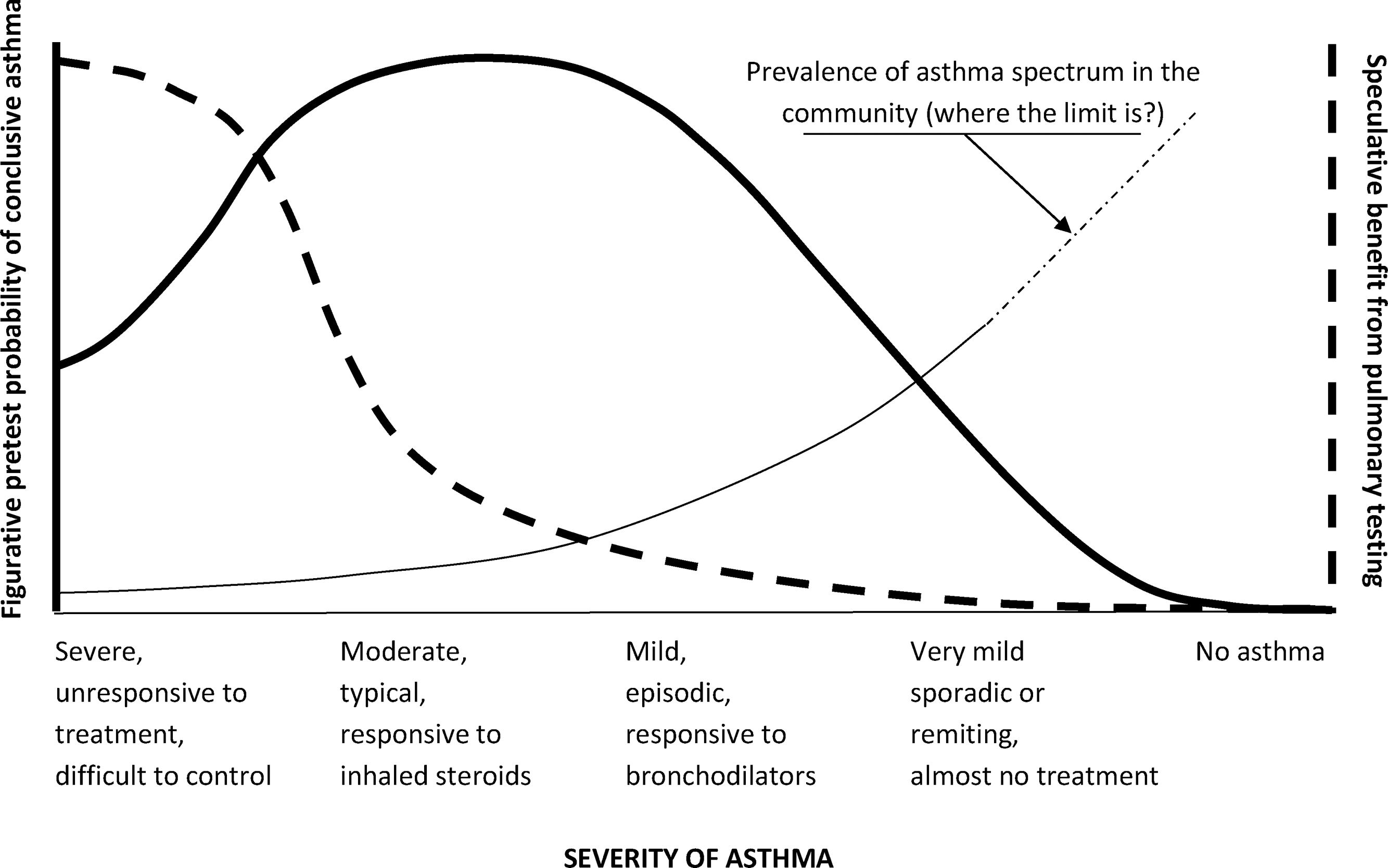
The role of lung testing in the diagnosis of asthma is questionable, as inferred from many of the studies cited by Mallol et al. Such tests may prove useful in patients with severe or difficult to control asthma, in order to help clarify the diagnosis and the presence of comorbidities. In typical asthma, the usefulness of lung testing for diagnostic purposes is questionable, although such tests are important for patient follow-up and management. It is more difficult to define their role in the case of asymptomatic patients or individuals with mild symptoms or in remission, where the discrepancies between the symptoms and the test results can be maximum. The diagnosis of asthma at this mild extreme of the disease is controversial and can mark a great difference in the prevalence of asthma in the community (Fig. 1). For the investigator, asthma over- or under-diagnosis is a great problem conditioned by the criteria used to define the disorder.9 However, for the clinician, the diagnosis of asthma is relatively simple in most cases, and greatly facilitates communication with the patient family, in all cases accepting the uncertainty of the prognosis, especially during childhood.
Schematic representation of the asthma severity spectrum and the potential role of pulmonary testing for asthma diagnosis (thick dashed line) according to pretest (or clinical) diagnosis of asthma (thick continuous line), and its implication in asthma prevalence (thin line). Pulmonary testing is especially useful in the infrequent cases of severe, difficult-to-control asthma, when a proper diagnosis must be confirmed. Pulmonary testing may lose sense in typical and responsive cases with a very high pretest probability of asthma. There is doubtful usefulness in pulmonary testing for most of the very large proportion of mild or very mild asthmatics in the community. Anywhere we place the mark at this end is arbitrary, and can make a big difference for asthma prevalence in the community.