With the help of a routine clinical case about delayed urticaria induced by drug, we have analyzed the scientific societies reports published during the last 5 years on this topic.
We highlighted the differences between the EAACI consensus and documents on drug allergy, commenting their positions and some of their definitions on delayed urticaria.
However, the question of disagreement between definitions of delayed urticaria can generate confusion. It would be beneficial to have more and “official” clearness about this topic because of its important clinical application to our patients.
V. is a 7-year-old girl who, at the age of 8 months, had an episode of hives that appeared 6h after receiving a weight-based dose of amoxicillin. An amoxicillin allergy was suspected and this antibiotic was never administered to V. again. More than 6 years after that episode, the girl's parents approached our pediatric allergy clinic to try to clarify the situation. Skin test with amoxicillin was negative, and V. performed, while she was in good health, an oral amoxicillin challenge that was negative for immediate cutaneous allergic reaction. She continued the intake of the antibiotic at home, in order to increase the sensitivity of the challenge test to delayed allergic reactions, assuming a total of 12 doses of amoxicillin. After about 30h from the last dose of antibiotic, and 5 days after the first dose, V. presented itching hives on the right arm, at the level of the front face of the elbow. Considering that urticarial rash 6h after the last intake of a drug is unusual, and its very modest intensity in the case of V., in order to have further confirmation of possible allergy, we performed a second oral amoxicillin challenge 2 months after the first one, V. was always healthy. This second challenge showed onset of itching hives after 3h from the last dose of amoxicillin and two days after the first dose. Both in the case of the first and the second challenge the rash disappeared after administration of an antihistaminic drug and antibiotic suspension.
Consent for publication: Informed consent was obtained from the participant included in the study.
Can a drug induce delayed urticaria? To resolve this doubt, we have analyzed the scientific societies reports published in the last 5 years.
According to the “International Consensus on drug allergy” of the European Academy of Allergy and Clinical Immunology (EAACI) of 2014,1 drug hypersensitivity reactions (DHRs) can be:
- -
Immediate (urticaria, angioedema, rhinitis, conjunctivitis, bronchospasm, gastrointestinal symptoms, anaphylaxis, anaphylactic shock), that typically occur within 1–6h after the last drug administration.
- -
Non-immediate (delayed urticaria, maculopapular eruptions, fixed drug eruptions, vasculitis, toxic epidermal necrolysis, and Stevens–Johnson syndrome, drug reaction with eosinophilia and systemic symptoms (DRESS), acute generalized exanthematous pustulosis and symmetrical drug-related intertriginous and flexural exanthemas, that typically occur at any time as from 1h after the initial drug administration.
Then, at least in the 2014 and according to EAACI consensus1, a delayed urticaria exists. Particularly in a table of their document, the authors attribute an immunological type III reaction and a time of onset after 7-8 days after the start of the eliciting drug to delayed urticaria.
This indication is reaffirmed in another EAACI document of 2016, the Position Paper “In vitro tests for Drug Hypersensitivity Reactions”.2 Curiously, in both documents of EAACI, it is reported that the tables we have mentioned are adapted from a review of Pichler WJ,3 but delayed urticaria is not mentioned at any point in that review. Contrary to what has been reported until now,1,2 in a table of the most recent EAACI position paper on “How to classify cutaneous manifestations of drug hypersensitivity” of 2018,4 the definition of delayed urticaria disappeared. In this case, the authors refer to a guideline of the German Society for Allergology and Clinical Immunology (DGAKI),5 where in type III immunological reactions are reported only cytopenia, serum sickness and vasculitis. One year later, the delayed urticaria reappears in Table 2 of another EAACI consensus paper about the diagnosis of hypersensitivity to beta-lactams.6
Beyond the contradictions in EAACI documents, other papers of leading researchers in the last 5 years are not sufficiently clear in answering that specific question: “Does delayed urticaria induced by drug allergy exist?”.
For example, in a recent review on antibiotics allergy,7 urticaria is cited only as an immediate cutaneous reaction that typically appears within 1-6h of drug exposure and, in the same document, type III immunological reactions include only the serum sickness or serum sickness-like reaction, described with fever, rash (not specifying what kind of rash), and arthralgia.
On the contrary, Romano et al.8 affirm that the most common non-immediate cutaneous reactions during beta-lactam treatments are maculopapular exanthemas and urticarial eruptions. Atanaskovic-Markovic et al.9 also confirmed that delayed urticaria exists by a prospective survey conducted in a group of 1026 children with histories of non-immediate reactions to beta-lactam antibiotics. In that study, children showed up an urticarial rash after a drug provocation test (DPT) to beta-lactam once they were back home doing the therapeutic course. The median time interval to the response in the DPT was 13h (2–48h after the last dose of drug).
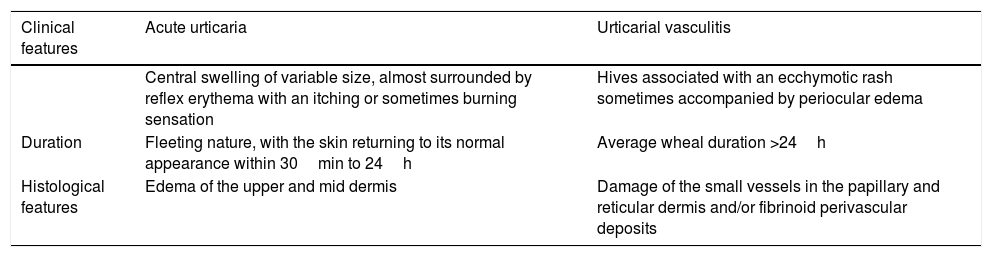
An explanation of these apparent discrepancies can be that in the literature it is well reported that the serum sickness-like reaction rash can be both urticarial and morbilliform. However, in this case, urticarial rash has different clinical features and it assumes the definition of urticarial vasculitis. In Table 1, we summarize the main characteristics of urticarial vasculitis rash compared with the classic acute urticaria.10,11 Despite these differences, is it perhaps possible that, in some classifications,4,7 delayed urticaria was included under the definition of “serum sickness-like reaction”? Maybe. However, this hypothesis, which can generate confusion anyway, is contradicted by the fact that in the 20141 and 20162 classifications serum sickness-like reaction, delayed urticaria and maculopapular exanthema are well distinguished, and are different diseases.
Main characteristics of acute urticaria and vasculitic urticaria.
| Clinical features | Acute urticaria | Urticarial vasculitis |
|---|---|---|
| Central swelling of variable size, almost surrounded by reflex erythema with an itching or sometimes burning sensation | Hives associated with an ecchymotic rash sometimes accompanied by periocular edema | |
| Duration | Fleeting nature, with the skin returning to its normal appearance within 30min to 24h | Average wheal duration >24h |
| Histological features | Edema of the upper and mid dermis | Damage of the small vessels in the papillary and reticular dermis and/or fibrinoid perivascular deposits |
It would be beneficial to have more and “official” clearness about this topic. In fact, the practical application of this issue is important: every time we visit a patient with an urticarial rash, do we need to ask if he took drugs in the previous eight days? And if so, do we need to perform diagnostic procedures for a possible drug allergy? In short, does delayed urticaria induced by drug allergy exist? We hope that the Scientific Societies will clarify this doubt.
DisclaimerWe declare that the work described has not been published previously, that it is not under consideration for publication elsewhere, that its publication is approved by all authors and tacitly by the responsible authorities where the work was carried out, and that, if accepted, it will not be published elsewhere in the same form, in English or in any other language, including electronically without the written consent of the copyright-holder.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributionsEster Del Vescovo conceived the design of the study and drafted the article. Giulia Bersani and Mariannita Gelsomino acquired the data and researched the scientific literature. Ester Del Vescovo and Stefano Miceli Sopo analyzed and commented on it. All authors revised the article and gave final approval of the version to be published.
Conflict of interestThe authors have no conflict of interest to declare.