Sensitisation to pan-allergens has become an interesting tool for the study of the allergenic profile of different populations. Profilins are one of the most common pan-allergens to be studied because they are responsible for a large number of sensitisations and are clearly related to cross-reactivity and co-sensitisation.
ObjectivesThe objective of this study was to investigate the profile of sensitisation to profilins and to correlate it with sensitisation to foods and pollens.
MethodsSix hundred and fifty-four consecutive patients were skin-prick tested with a battery of common allergens including pollens, epithelia, mites and moulds and profilin and divided into three groups depending on their sensitisation profile (non-atopic, atopic with pollinosis and atopic without pollinosis). Patients with symptoms were challenged and diagnosed with the offending food extracts. Profilin sensitisation was identified and analysed in detail.
ResultsAccording to the classification of the population, the prevalence of profilin sensitisation was estimated at 2.9% in patients suffering respiratory allergy, 4.2% in atopic patients, and 5.9% in pollen-sensitised individuals. Positive association was observed between pollen (except Cupressus and olive) and profilin but not with moulds, mites or epithelia. With respect to foods, positive association was only observed between profilin and melon sensitisation. Lastly, in terms of symptoms, positive association was only observed between profilin sensitisation and OAS.
ConclusionProfilin sensitisation seems to be a marker of pollen-related poly-sensitisation in our area. Pan-allergen diagnosis seems to be an essential tool for developing and improving selection of the correct treatment for allergic patients.
Profilins, with a molecular weight of approximately 12–14kDa, are ubiquitous proteins present in all eukaryotic cells and play a crucial role in regulating the activity in the microfilament system and intracellular calcium levels.1 Valenta et al.2 were the first to describe profilins as allergens, and they have now been recognised as an important family of pan-allergens,3 responsible for cross-sensitisation and co-sensitisation among pollens and between pollens and plant-derived food due to their high degree of homology.4 However, although profilins are also present in animals (humans included), they have only been identified as allergens in pollens and foods, probably due to the low degree of similarity and the method of exposure.5 To date, over 30 profilins have been reported as allergens on the IUIS website,6 in most cases identified as minor.
The use of skin prick tests containing a single purified profilin has been proposed as a diagnostic marker for profilin sensitisation.7 The prevalence of sensitisation has been studied in different regions and countries. Studies conducted in European regions have estimated skin sensitisation to date-palm-pollen profilin (Pho d 2) to be between 12.3% and 30% in patients with pollinosis.8–11 In vitro studies in Central Europe estimated that birch-pollen-profilin (Bet v 2) sensitisation is responsible for 10–20% of patients with pollen allergy.12,13 A similar rate (21%) was described in a study of 370 individuals in Portugal,14 and significant differences depending on geographical area were found in Spain.9,15
Despite high prevalence figures and the association of profilin sensitisation with other plants, the role of profilin as an allergen has long been questioned.16 The capacity of profilins to induce respiratory symptoms has recently been demonstrated17 and its role as an important allergen has been confirmed in patients exposed to high quantities of grass pollens.18 Moreover, Asero et al.8 demonstrated that over 50% of patients sensitised to profilins experienced symptoms with plant-derived foods, suggesting that profilins should be considered as a clinically relevant food allergen.19 Most of these patients, who were allergic to food allergens and sensitised to profilins, had only mild symptoms. These symptoms generally involved oral allergy syndrome (OAS), since profilins are rapidly degraded/inactivated by the enzymes present in the digestive tract.20,21
The objectives of this study were: to describe the prevalence of skin sensitisation to profilin with a skin prick test consisting of profilin from date-palm pollen (Pho d 2) in patients with suspicion of respiratory allergy (rhinoconjunctivitis and/or bronchial asthma) living in the southeast of Spain; to identify the clinical profile of profilin-sensitised individuals; and to calculate the correlation between profilin sensitisation and common aeroallergens and plant-derived food-allergen sensitisation.
Materials and methodsPatient populationSix hundred and fifty-four individuals (347 females, 307 males; mean age 24.4 years, range 3–82) who attended the Allergy Service and lived on Spain's Mediterranean coast (in the area of Cartagena, Murcia) were consecutively included in the study. Only patients reporting symptoms related to respiratory allergy such as rhinitis, rhinoconjunctivitis and/or asthma were included. All enrolled patients were asked about symptoms after contact with or ingestion of plant-derived foods. Individuals reporting skin symptoms or diagnosed with drug or venom allergy were excluded.
Detailed clinical data were collected for each patient. The study was conducted with the approval of the Complejo Hospitalario Universitario de Cartagena (Murcia) ethics committee and all patients included in the study gave their oral consent.
Skin prick testsAll individuals were skin-prick tested with a battery of common biologically standardised aeroallergens (30HEP/ml) including house-dust mites (Dermatophagoides pteronyssinus and Dermatophagoides farinae), moulds (Alternaria alternata, Cladosporium herbarum and Aspergillus fumigatus), epithelia (dog and cat), pollens (mixture of grasses, Cynodon dactylon, Olea europaea, Chenopodium album, Salsola kali, Parietaria judaica, Artemisia vulgaris, Platanus acerifolia, Plantago lanceolada, Cupressus arizonica, Phoenix dactifera and Betula alba) (Laboratorios Leti S.L., Madrid, Spain) and profilin (50mcg/ml) from date-palm-tree pollen.
Patients reporting symptoms to food were also skin-prick tested with the offending allergen extracts.
Skin prick tests were conducted on the volar surface of the forearm, following EAACI recommendations.22
Epidemiological studiesIn an initial epidemiological study, the total population was classified into three groups: (a) non-atopic; (b) atopic with pollinosis; and (c) atopic without pollinosis. Symptoms, pollen sensitisation and food sensitisation were determined in all the individuals. Pollen sensitisation was considered positive when wheal size to any of the pollen extracts included in the battery was ≥7mm2. Food-allergy sensitisation was considered positive when individuals reported symptoms after food ingestion and had a positive skin prick test (≥7mm2) with the offending allergen extract.
In a second study, we focused our attention on groups b and c (atopic individuals with pollinosis and atopic individuals without pollinosis) and profilin sensitisation. Atopic sensitised individuals were subdivided into two groups according to whether the skin prick test to profilin-enriched extract was positive or not.
Statistical analysisStatistical analyses were conducted using SigmaStat v.3.5 and SigmaPlot v.10.0 software. Proportions were analysed using contingency tables, and the non-parametric Fisher's exact probability test was applied. In all cases, a p value of ≤0.05 was considered statistically significant and p≤0.01 was defined as highly significant. Statistically significant results indicate a positive/significant association between the two variables considered in each case.
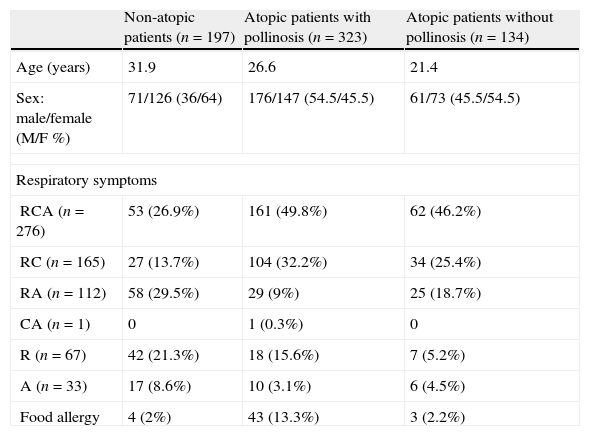
ResultsPatient descriptionAccording to the positive skin prick tests, patients were divided into non-atopic (197, 30.1%) and atopic (457, 69.9%). A total of 323 (49.4%) atopic individuals were sensitised to pollens and 134 (20.5%) exclusively to other aeroallergens, including mites, moulds or epithelia. Gender and mean age distribution are shown in Table 1.
Description of the population studied.
| Non-atopic patients (n=197) | Atopic patients with pollinosis (n=323) | Atopic patients without pollinosis (n=134) | |
| Age (years) | 31.9 | 26.6 | 21.4 |
| Sex: male/female (M/F %) | 71/126 (36/64) | 176/147 (54.5/45.5) | 61/73 (45.5/54.5) |
| Respiratory symptoms | |||
| RCA (n=276) | 53 (26.9%) | 161 (49.8%) | 62 (46.2%) |
| RC (n=165) | 27 (13.7%) | 104 (32.2%) | 34 (25.4%) |
| RA (n=112) | 58 (29.5%) | 29 (9%) | 25 (18.7%) |
| CA (n=1) | 0 | 1 (0.3%) | 0 |
| R (n=67) | 42 (21.3%) | 18 (15.6%) | 7 (5.2%) |
| A (n=33) | 17 (8.6%) | 10 (3.1%) | 6 (4.5%) |
| Food allergy | 4 (2%) | 43 (13.3%) | 3 (2.2%) |
In terms of the respiratory and ocular symptoms in the total population, 620 (94.8%) individuals suffered from rhinitis, 442 (67.6%) from conjunctivitis and 422 (64.5%) from bronchial asthma. The most common associations were found between rhinitis, conjunctivitis and bronchial asthma (276, 42.2%), and rhinitis and conjunctivitis (165, 25.2%). In contrast, just one patient reported only having conjunctivitis and asthma. Respiratory symptoms are also detailed in Table 1.
Fifty-nine (9%) individuals reported symptoms after contact or ingestion with plant-derived foods. However, only 50 (7.4%) of these were considered allergic since skin prick tests with the offending foods were negative on the remaining nine subjects. Table 1 shows the correlation between food allergy and airborne allergens established by the positivity of the skin prick test.
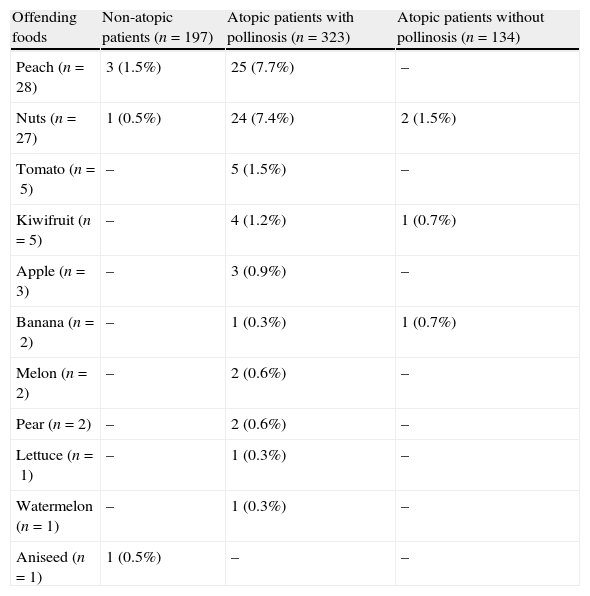
Peach and nuts were the most common offending plant-derived foods implicated in allergic reactions. A list of the foods associated with allergic symptoms in the population studied is provided in Table 2. Twenty-one (42%) patients had food allergy to more than one food: fifteen (30%) to two; and six (12%) to three. All patients allergic to more than two different plant-derived foods were also sensitised to pollens.
Offending plant-derived foods implicated in allergy reactions.
| Offending foods | Non-atopic patients (n=197) | Atopic patients with pollinosis (n=323) | Atopic patients without pollinosis (n=134) |
| Peach (n=28) | 3 (1.5%) | 25 (7.7%) | – |
| Nuts (n=27) | 1 (0.5%) | 24 (7.4%) | 2 (1.5%) |
| Tomato (n=5) | – | 5 (1.5%) | – |
| Kiwifruit (n=5) | – | 4 (1.2%) | 1 (0.7%) |
| Apple (n=3) | – | 3 (0.9%) | – |
| Banana (n=2) | – | 1 (0.3%) | 1 (0.7%) |
| Melon (n=2) | – | 2 (0.6%) | – |
| Pear (n=2) | – | 2 (0.6%) | – |
| Lettuce (n=1) | – | 1 (0.3%) | – |
| Watermelon (n=1) | – | 1 (0.3%) | – |
| Aniseed (n=1) | 1 (0.5%) | – | – |
Symptoms with plant-derived foods reported by patients were heterogeneous: 15 (30%) contact urticaria; 15 (30%) OAS; 10 (20%) urticaria/angio-oedema; eight (16%) angio-oedema; six (12%) urticaria; and four (8%) anaphylaxis. Nine (42.9%) of the 21 allergic patients reported symptoms with more than one food. The foods involved are shown in Table 2.
Prevalence of sensitisation to profilinNineteen individuals were sensitised to date-palm-pollen profilin, all of whom were atopic and sensitised to pollens. The prevalence of sensitisation to profilin in our area was 2.9% in patients suffering respiratory allergy, 4.2% in atopic patients; and 5.9% in pollen-sensitised individuals.
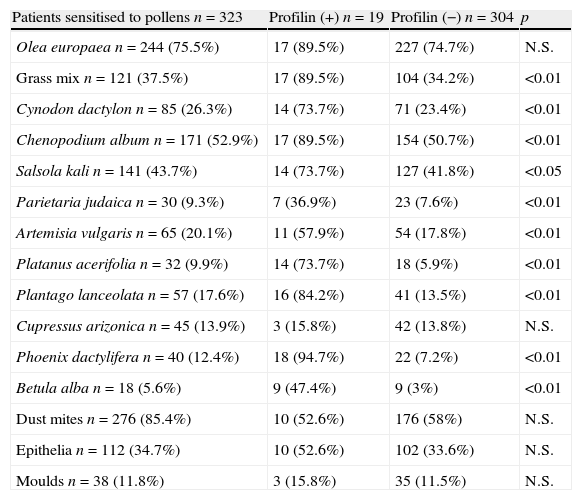
Skin prick tests with aeroallergens in atopic patients. Comparison of patients sensitised and not sensitised to profilinThree hundred and twenty-three (49.4%) patients were sensitised to at least one of the pollens studied. The results of the skin prick tests with aeroallergens in patients with pollinosis are shown in Table 3.
Skin prick tests with aeroallergens in patients sensitised to pollens. Association between pollen sensitisation and positive skin prick test to profilin.
| Patients sensitised to pollens n=323 | Profilin (+) n=19 | Profilin (−) n=304 | p |
| Olea europaea n=244 (75.5%) | 17 (89.5%) | 227 (74.7%) | N.S. |
| Grass mix n=121 (37.5%) | 17 (89.5%) | 104 (34.2%) | <0.01 |
| Cynodon dactylon n=85 (26.3%) | 14 (73.7%) | 71 (23.4%) | <0.01 |
| Chenopodium album n=171 (52.9%) | 17 (89.5%) | 154 (50.7%) | <0.01 |
| Salsola kali n=141 (43.7%) | 14 (73.7%) | 127 (41.8%) | <0.05 |
| Parietaria judaica n=30 (9.3%) | 7 (36.9%) | 23 (7.6%) | <0.01 |
| Artemisia vulgaris n=65 (20.1%) | 11 (57.9%) | 54 (17.8%) | <0.01 |
| Platanus acerifolia n=32 (9.9%) | 14 (73.7%) | 18 (5.9%) | <0.01 |
| Plantago lanceolata n=57 (17.6%) | 16 (84.2%) | 41 (13.5%) | <0.01 |
| Cupressus arizonica n=45 (13.9%) | 3 (15.8%) | 42 (13.8%) | N.S. |
| Phoenix dactylifera n=40 (12.4%) | 18 (94.7%) | 22 (7.2%) | <0.01 |
| Betula alba n=18 (5.6%) | 9 (47.4%) | 9 (3%) | <0.01 |
| Dust mites n=276 (85.4%) | 10 (52.6%) | 176 (58%) | N.S. |
| Epithelia n=112 (34.7%) | 10 (52.6%) | 102 (33.6%) | N.S. |
| Moulds n=38 (11.8%) | 3 (15.8%) | 35 (11.5%) | N.S. |
N.S.: non-statistically significant differences; p<0.05, significant differences; p<0.01, highly significant differences.
Olive was the most recognised allergen extract. A total of 244 individuals (75.5%) were sensitised to olive pollen, 64 (26.2%) of these only to this pollen, although some showed positivity to other aeroallergens (dust mites, moulds and/or epithelia). A non-statistically significant association was found between olive pollen and profilin.
Profilin sensitisation was statistically significant with all the pollens included except Cupressus and olive.
Non-significant differences were obtained between profilin sensitisation and moulds, mites and epithelia (see Table 3).
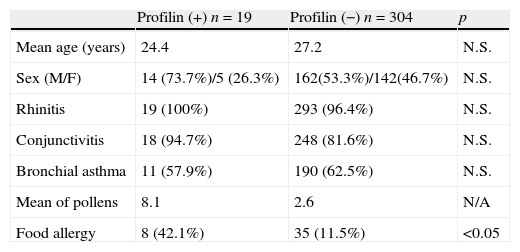
Association between profilin sensitisation and clinical symptoms. Clinical profile of patients sensitised to profilinProfilin sensitisation showed a positive correlation with food allergy (p=0.001) (Table 4). Individuals with positive skin prick test to profilin were sensitised to a higher proportion of pollens in comparison with non-sensitised individuals. Non-significant differences were found between the two groups with regard to mean age, gender and respiratory symptoms (Table 4).
Comparison of clinical profile of patients with pollinosis sensitised and non-sensitised to profilin.
| Profilin (+) n=19 | Profilin (−) n=304 | p | |
| Mean age (years) | 24.4 | 27.2 | N.S. |
| Sex (M/F) | 14 (73.7%)/5 (26.3%) | 162(53.3%)/142(46.7%) | N.S. |
| Rhinitis | 19 (100%) | 293 (96.4%) | N.S. |
| Conjunctivitis | 18 (94.7%) | 248 (81.6%) | N.S. |
| Bronchial asthma | 11 (57.9%) | 190 (62.5%) | N.S. |
| Mean of pollens | 8.1 | 2.6 | N/A |
| Food allergy | 8 (42.1%) | 35 (11.5%) | <0.05 |
Forty-three pollen-sensitised individuals showed food allergy, eight (18.6%) of whom were sensitised to profilins. The offending plant-derived foods implicated in allergic reaction in patients with pollinosis are listed in Table 2. Twenty-one (48.8%) of these individuals (n=43) reported symptoms with more than one food: 15 (34.8%) with two; and six (13.9%) with three. Five (62.5%) patients with food allergy and sensitised to profilins reported symptoms with more than one food: three (37.5%) with three; and two (25%) with two.
Food-allergic patients also sensitised to profilin were more frequently sensitised to more than one food in comparison with those who had no food allergy and showed no sensitisation to profilin: 5/8 (62.5%) versus 16/35 (45.7%).
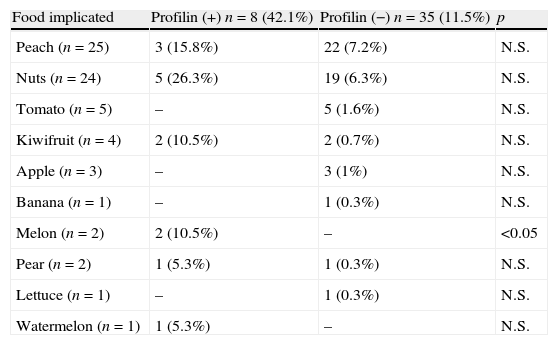
The association of foods implicated in allergic reactions with profilin sensitisation depended on the kind of food involved (Table 5). None of the profilin-sensitised individuals reported symptoms with tomato, apple, banana or lettuce. In contrast, all patients allergic to melon and watermelon were sensitised to profilin.
Plant-derived food allergy in pollinic patients sensitised and non-sensitised to profilin.
| Food implicated | Profilin (+) n=8 (42.1%) | Profilin (−) n=35 (11.5%) | p |
| Peach (n=25) | 3 (15.8%) | 22 (7.2%) | N.S. |
| Nuts (n=24) | 5 (26.3%) | 19 (6.3%) | N.S. |
| Tomato (n=5) | – | 5 (1.6%) | N.S. |
| Kiwifruit (n=4) | 2 (10.5%) | 2 (0.7%) | N.S. |
| Apple (n=3) | – | 3 (1%) | N.S. |
| Banana (n=1) | – | 1 (0.3%) | N.S. |
| Melon (n=2) | 2 (10.5%) | – | <0.05 |
| Pear (n=2) | 1 (5.3%) | 1 (0.3%) | N.S. |
| Lettuce (n=1) | – | 1 (0.3%) | N.S. |
| Watermelon (n=1) | 1 (5.3%) | – | N.S. |
A positive association was only observed between profilin and melon sensitisation.
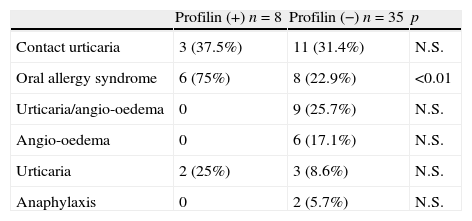
Association between symptoms and food/profilin sensitisationSymptoms with plant-derived foods reported by pollen-sensitised patients and profilin sensitisation are shown in Table 6.
Symptoms with plant-derived foods in patients sensitised or non-sensitised to profilin.
| Profilin (+) n=8 | Profilin (−) n=35 | p | |
| Contact urticaria | 3 (37.5%) | 11 (31.4%) | N.S. |
| Oral allergy syndrome | 6 (75%) | 8 (22.9%) | <0.01 |
| Urticaria/angio-oedema | 0 | 9 (25.7%) | N.S. |
| Angio-oedema | 0 | 6 (17.1%) | N.S. |
| Urticaria | 2 (25%) | 3 (8.6%) | N.S. |
| Anaphylaxis | 0 | 2 (5.7%) | N.S. |
Contact urticaria and OAS were the most frequently reported symptoms. Nine (47.3%) allergic patients had different symptoms with different foods. Five such patients allergic to more than one food were sensitised to profilins and two were sensitised to two foods. However, three patients sensitised to three foods reported OAS with all the allergens to which they were sensitised.
The distribution of reported symptoms and profilin sensitisation is summarised in Table 6. The only positive association observed was between profilin sensitisation and OAS (p=0.009). No patients with positive skin prick test to profilin reported anaphylaxis or angio-oedema.
DiscussionInterest in describing sensitisation to pan-allergens has increased significantly in recent years due to the importance of establishing patterns of sensitisation in order to improve recommendations for specific immunotherapy and to establish associations or cross-reactivity between foods and pollens. Profilins are important markers of this syndrome, and represent cross-reactive allergens for almost 20% of pollen-allergic patients. Moreover preliminary studies have demonstrated that actin-binding domains in plant and animal profilins are functionally highly conserved, although the overall sequence similarity is less than 25%.23 This is the first time that such a detailed study of this kind has been carried out in our area, and we believe it will prove to be very helpful in terms of making accurate diagnoses and consequently deciding on the most appropriate immunotherapy. There is no doubt that specific immunotherapy or products for the induction of immune tolerance with pan-allergens could be very useful for some specific groups of individuals.24
The prevalence of sensitisation to profilins in Spain, using molecular diagnosis of Mal d 4 as a marker for profilin sensitisation, has been estimated to be between 10% and 50% in pollen-sensitised individuals, depending on the area studied.20 These values are considerably higher than those observed in our study, where the prevalence of cutaneous sensitisation to date-palm profilin (Pho d 2) was estimated at 5.9% in pollen-sensitised individuals (n=323) and 2.9% in the study population overall (n=654). This value is high in patients with pollen allergy but can be considered low with respect to the 30% described in northern Italy8 and the rates observed in other parts of Spain (12.3% in central Spain10 and 23.5% in the south of the country11), where the authors used an extract with the same composition and similar methodology. The differences in these results may be explained by a number of factors. Firstly, in northern Italy and some areas of Spain, where the prevalence is significantly higher than that obtained in our area, the differences may be related to the high prevalence of sensitisation to grasses.10,11 A recent study reported that profilin content in grasses (Lolium perenne and Phleum pratense) is higher than in trees and weeds.18 These results also correlate with our population, where a positive association between grass and profilin sensitisation was found, confirming previous suggestions of an association between Phl p 5 and profilins.11 However, in the southeast of Spain, the most prevalent pollen is olive. In the case of olive (Ole e 1 and Ole e 9 are the most important region-specific allergens), as well as Cupressus (profilins have not been described as allergens), profilins are not relevant. In fact, we did not find a positive association between either Olea or Cupressus sensitisation, and profilins. Another explanation could be related to the constant water stress to which pollen grains are subject in our region. Low levels of humidity may be related to the synthesis of profilin and be responsible for the lower levels expressed in different climatic regions where the rainfall is much higher. The southeast of Spain is characterised by semi-arid conditions, with scant rainfall.
We also observed a significantly lower prevalence with respect to central Europe. In these regions, birch is the main sensitiser. Authors estimate that the prevalence of sensitisation ranges from 10% to 20%,12,13 although in this case, the values were also lower than the 30% found in northern Italy.8 Our studies confirmed a positive association between profilins and birch-sensitised individuals, probably related to cross-reactivity because of the absence of this tree in our area. The differences between these two regions may be explained by the fact that profilin has been described as a minor allergen in birch pollen and major allergen in grasses.19
A positive correlation was also found between Parietaria sensitisation and profilin, although previous studies have suggested no cross-reactivity between profilin from Parietaria and birch or grasses.25 Although Par j 1 and Par j 2 are considered the major allergens in Parietaria, the profilin Par j 3 has been identified as an important sensitiser. All these differences demonstrate that prevalence of sensitisation to profilin depends not only on the geographical conditions but also on differences in the correlation between profilin and pollens and the capacity of the allergens to co-sensitise. Lastly, positive association with other pollens, including Phoenix, Plantago, Platanus and Chenopodiaceae, are explained by the presence of profilins in these pollens and their capacity for sensitisation.
With respect to the relationship between profilins and foods, we observed a significant association between these two variables (p<0.05). In line with previously published papers,19 we found a high percentage of individuals (42%) sensitised to profilin with clinical symptoms following food ingestion or handling, confirming that profilin may be a clinically relevant food allergen. Moreover, as with pollens, profilin-sensitised individuals not only had higher rates of food allergy but they were also allergic to a higher number of foods with respect to negative individuals: 62.5% were sensitised to two or three foods respect to all the 25% and 45.7% negative individuals. In parallel, 75% individuals sensitised to profilins reported OAS, with a positive association (p<0.01). However, none of these subjects showed severe symptoms, including angio-oedema or anaphylaxis (non-statistically significant differences), confirming previous studies which demonstrate that profilins, as they are degraded by gastric acids, are not associated with generalised and severe symptoms.20
With regard to individual foods, nuts and peaches were the main foods involved in allergic reactions in our population, although no significant association was observed with profilin sensitisation. This would seem logical because, in spite of the presence of profilins in both foods, it is clearly a minor allergen. Asero et al. reported that 50% of reactions with food described in profilin-sensitised individuals were related to apple or tomato.8 In our population, we found no positive association with these two fruits and profilins, confirming previous studies where the involvement of lipid transfer proteins was demonstrated.26,27 Other studies have suggested that sensitisation to different fruits could be related with profilins as a marker of hypersensitivity in food-sensitised individuals.28 We only found a positive association with melon, confirming the results of a number of different authors.29 These results suggest that the correlation between profilin-sensitisation and food allergy depends on geographical area.
Lastly, as expected, no association was observed between profilin sensitisation and sensitisation to mites, moulds or epithelia.4
Nevertheless, it is important to note that cross-reactivity between profilins and carbohydrate determinants is capable of inducing cross-reactive IgE antibodies with little clinical relevance. Although the role of carbohydrate determinants has not been included nor considered in our study, some of the reactivity to our extracts could be mediated or influenced by this phenomenon; this has also been reported in other published papers in connection with different allergen extracts.21
In summary, the prevalence of sensitisation to profilin in our area is significantly lower than that observed in other regions of the Iberian Peninsula or Europe. Moreover, as a consequence of this lower prevalence, we have also found differences in the association between sensitisation to profilins and sensitisation to foods and pollens when our results are compared with other geographical areas. These results suggest that differences in the prevalence of sensitisation to profilins could be associated with a different clinical expression with regard to pollens and foods. We have also observed that profilin sensitisation is always related to polysensitisation to pollens. Consequently, and according to the observed results, we consider that other studies including more pan-allergens (LTPs, polcalcins or even carbohydrates determinants) could explain sensitisation profiles. The main challenge of this kind of studies is to establish the cause-effect of these allergens such as the agents responsible for an allergenic response, with highly purified specific proteins, through provocation tests. For that reason, we consider further in-depth study of pan-allergen sensitisation to be essential in order to improve/develop the treatment of allergic patients.
Ethical disclosuresConfidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Protection of human subjects and animals in researchThe authors declare that no experiments were performed on humans or animals for this investigation.
Conflict of interestThe authors have no conflict of interest to declare.