Migrants from developing to Western countries tend to become more sensitised to host than to origin country allergens, although substantial changes in migration patterns have occurred in recent decades.
MethodsWe investigated adult immigrants with respiratory allergy, first tested for allergic sensitisation between 1985 and 2012 in a highly industrialised area in Italy. A comparison was made of the sensitisation pattern between immigrants and a random sample of native-born subjects affected by a respiratory allergy, and among immigrants according to macro-region of origin and time period.
ResultsBetween 1985 and 2012, 480 immigrants with respiratory allergy had a first positive allergy test. Immigrants were sensitised mainly to grass (67.1%), house dust mites (HDM) (38.5%) and birch (27.5%), with a pattern of sensitisation very similar to that observed in Italians (native-born). An increase in the proportion of subjects with asthma and of subjects with polysensitisation was observed from the first (1985–2002) to the middle (2003–2007) and the most recent period (2008–2012). In recent years, the proportion of subjects with polysensitisation in immigrants is higher than in Italians (native-born) (53.3% vs. 40.1%). Among immigrants, the risk of sensitisation to grass was higher in those from Sub-Saharan Africa (odds ratio, OR=2.76) and Latin America (OR=2.49), whereas risk of sensitisation to HDM was higher among immigrants from South Asia (OR=2.71), compared to immigrants from Eastern Europe.
ConclusionsImmigrants develop multiple sensitisations more frequently than native-born people, and are especially sensitised to local allergens; the country of origin seems to play a role.
Atopy and asthma result from the effects of environmental factors on genetically susceptible subjects, and their prevalence varies markedly throughout the world, not just between regions and countries but even between locations in the same country and the same city.1,2
Nearly 5% of the world population are migrants. Migration involves social as well as intriguing medical issues. It involves not only exposure to a new set of pollutants and previously unknown allergens, but also several socioeconomic and cultural issues, such as housing conditions, diet and accessibility to medical services.3
Various studies have evaluated the prevalence of atopy and respiratory allergic diseases in child and adult immigrants in Western countries using either a questionnaire or clinical-based data.3 Overall, they showed a higher prevalence of allergic diseases among immigrants compared to their countries of origin, which is independent of ethnicity.3 This phenomenon is time- and age-dependent, since immigrants born on arrival in the host country tend, in their early years, to have a similar prevalence of atopy to that of native-born people.3 The pattern of sensitisation seems to depend on both host country and country of origin features.3 Some studies in the past decade have investigated the frequency of allergic diseases in immigrants to Italy using clinical data,4–7 but only one of them evaluated the pattern of allergen sensitisation by macro-area of origin4 and none of them evaluated the temporal changes in allergic pattern in immigrants to Italy in the last few decades.
We aimed to investigate the frequency of allergic respiratory diseases and sensitisation in adult immigrants who attended the main Allergy Unit in a highly industrialised area in North Italy between 1985 and 2012.
MethodsPatient populationImmigrants who were born outside the European Union (EU), had a respiratory allergy, were aged 15 years and over, lived in the province of Brescia and were first tested for allergic sensitisation at the Allergy Unit of the Spedali Civili hospital in Brescia, the main centre for allergic diseases in the area, between 1985 and 2012, were included in the study. The local Ethics Committee approved the study design and protocol.
The immigrants were referred by their general practitioners (GPs) or, more rarely, by an Emergency Unit. All patients were able to speak Italian or were accompanied by an Italian-speaking relative.
They were grouped into six macro-regions, based on the immigrants’ country of origin: Eastern Europe, North Africa, Sub-Saharan Africa, Latin America, South Asia (including India, Bangladesh, Sri Lanka and Pakistan) and Far East Asia (including China, Vietnam and the Philippines).
Respiratory allergy was defined by the presence of respiratory allergic symptoms (rhinitis and asthma) and a positive skin prick test or serum-specific IgE.
Skin prick tests (STPs) were done using a panel of commercial extracts of the allergens (Lofarma, Milan, Italy) of the most common allergens responsible for respiratory symptoms in Italy: pollens (Graminaceae mix 5: grass; Compositae mix; Parietaria mix: pellitory; Betula pendula: birch; hazelnut; olive, cypress), house dust mites (HDM: Dermatophagoides pteronyssinus and D. farinae), animal danders (dog, cat), feather mix and moulds (Alternaria alternata, Aspergillus fumigatus, Cladosporium herbarum, Penicillum mix). All SPTs were performed and read in accordance with standard methods.8 Serum-specific IgEs were detected by currently available commercial laboratory methods (RAST and ImmunoCAP; Pharmacia AB, Uppsala, Sweden, formerly Phadia AB, now Thermo Fischer Scientific).
In order to investigate temporal trends of sensitisation in immigrants, we classified patients according to the year of first diagnosis of respiratory allergy into the two most recent five-year periods (2003–2007 and 2008–2012) and the previous period (1985–2002).
For each subject, we collected data on age, gender, allergic symptoms, pattern of sensitisation, and country of origin. Furthermore, a random sample of immigrants with respiratory allergy, diagnosed from 2006 to 2012, were interviewed by telephone and were asked the year of their arrival in Italy and the year of onset of symptoms. In order to compare the pattern of sensitisation between immigrants and native-born population, we retrieved data on a random sample of Italian (native-born) patients with respiratory allergy admitted to our centre in the same period.
Official data on the immigrant population living in the province of Brescia in 2003–2011 were collected from the ISTAT web site.9
Statistical analysisCommon statistical methods were used for the analysis of proportions and associations between demographic and clinical features.
Some allergens which few people were reactive to (hazelnut, olive, Compositae, mould and cypress) and immigrants from Far East Asia were excluded from the statistical analysis owing to small numbers.
A comparison of the sensitisation pattern was performed among immigrants and between immigrants and native-born patients according to age, gender and macro-regions of origin. The associations between macro-region of origin, gender, age and sensitisation to some allergens were also analysed using logistic regression models. The results are reported as odds ratios (ORs) and their 95% confidence intervals (95% CIs).
For statistical tests, P values lower than 0.05 were considered significant in two-tailed tests. All the computations were carried out using the STATA programme for personal computer, version 12.0 (STATA Statistics/Data Analysis 12.0 – STATA Corporation, College Station, TX, USA).
ResultsBetween 1985 and 2012, 480 immigrants (49.2% males; mean age±SD: 33.6±8.6 years) with respiratory allergy had their first positive test at our centre. The majority of them were aged 35 years or less. The macro-regions of origin, in decreasing order, were Eastern Europe (22.5%), South-East Asia (20.6%), Sub-Saharan Africa (19.8%), North Africa (19.2%), Latin America (13.5%), and Far East Asia (4.4%).
The number of immigrants with respiratory allergy according to year of the first positive test was small up until the early 2000s, and subsequently increased sharply, approximating an exponential distribution (R-square=0.96) (Fig. 1A). Similarly, from 2003 to 2011 a steady increase was evident in the number of immigrants living in the province of Brescia (Fig. 1B).
The demographic and clinical characteristics of the immigrants according to macro-region of origin are set out in Table 1. The male:female ratio differed significantly among macro-areas (P<0.001): immigrants from North Africa and South Asia were mainly males (71.7% and 73.7% respectively), whereas the majority of those from the other areas were females. Almost all had allergic rhinitis (95.8%), 44.4% had bronchial asthma and 49.4% presented polysensitisation. No differences were found for age and presence of asthma, rhinitis and polysensitisation by macro-area of origin.
Gender, age, prevalence of asthma, rhinitis and polysensitisation in immigrants aged 15 years and over with respiratory allergy and a first positive test in 1985–2012, according to macro-area of origin and calendar period.
| Male No. (%) | Age mean (SD) | Asthma No. (%) | Rhinitis No. (%) | Polysensitisation No. (%) | Total No. (%)a | |
|---|---|---|---|---|---|---|
| Macro-area of origin | ||||||
| North Africa | 66 (71.7) | 32.1 (7.4) | 50 (54.3) | 86 (93.5) | 35 (38.0) | 92 (19.2) |
| Sub-Saharan Africa | 46 (48.4) | 33.3 (6.7) | 44 (46.3) | 94 (99.0) | 53 (55.8) | 95 (19.8) |
| South Asia | 73 (73.7) | 33.8 (9.0) | 38 (38.4) | 94 (94.9) | 48 (48.5) | 99 (20.6) |
| Eastern Europe | 28 (25.9) | 34.1 (10.0) | 49 (45.4) | 102 (94.4) | 58 (53.7) | 108 (22.5) |
| Far East Asia | 10 (47.6) | 37.0 (8.6) | 3 (14.3) | 20 (95.2) | 11 (52.4) | 21 (4.4) |
| Latin America | 13 (20.0) | 34.2 (9.0) | 29 (44.6) | 64 (98.5) | 32 (49.2) | 65 (13.5) |
| Calendar period | ||||||
| 1985–2002 | 38 (52.8) | 32.7 (7.0) | 38 (52.8) | 67 (93.1) | 29 (40.3) | 72 (15.0) |
| 2003–2007 | 70 (51.5) | 33.4 (8.7) | 68 (50.0) | 130 (95.6) | 63 (46.3) | 136 (28.3) |
| 2008–2012 | 128 (47.1) | 34.1 (8.9) | 107 (39.3) | 263 (96.7) | 145 (53.3) | 272 (56.7) |
| Total | 236 (49.2) | 33.6 (8.6) | 213 (44.4) | 460 (95.8) | 237 (49.4) | 480 (100) |
Percentages are computed on the row total (total immigrants for each macro-area of origin).
An analysis of the time trend of the immigrants’ demographic and clinical characteristics shows a statistically significant decrease in the proportion of males and of subjects with asthma and an increase of those with polysensitisation from the first (1985–2002) to the middle (2003–2007) and the most recent period (2008–2012). No statistically significant change was observed in age distribution of immigrants in the different periods.
When comparing the proportion of immigrants from each area of origin by time, a substantial increase was found in the proportion of people from Eastern Europe, from 11% in 1985–2002 to 22% in 2003–2007 and 26% in 2008–2012. Reciprocally, we observed a decrease in the proportion of people from North Africa (from 26% to 13% and 20%) and Sub-Saharan Africa (from 32% to 16% and 18%) (data not shown in tables).
The pattern of sensitisation by geographic area and time is shown in Table 2. Immigrants were sensitised mainly to grass (67.1%), followed by HDM (38.5%), birch (27.5%) and Parietaria (12.3%). There were statistically significant differences by area of origin in sensitisation to grass (P=0.001), Parietaria (P=0.01) and HDM (P<0.001). Using logistic regression models, with macro-area of origin, age and gender as independent variables, it was found that the risk of sensitisation to grass was higher among immigrants from Sub-Saharan Africa and Latin America, and similar for those from the other areas, compared to immigrants from Eastern Europe, considered as the reference (Table 3). On the contrary, the risk of sensitisation to HDM was higher among immigrants from South Asia and not different for people from the other areas. Sensitisation to grass in total immigrants did not vary with time, whereas the number of subjects sensitive to birch and composite showed a statistically significant increase from 1985–2002 to 2003–2007 and 2008–2012.
Pattern of sensitisation to allergens in adult immigrants according to macro-area of origin and calendar period.
| Allergen | ||||||||
|---|---|---|---|---|---|---|---|---|
| Grass No. (%) | HDM No. (%) | Parietaria No. (%) | Birch No. (%) | Animals No. (%) | Hazelnut No. (%) | Olive No. (%) | Composite No. (%) | |
| Macro-area of origin | ||||||||
| North Africa | 55 (59.8) | 39 (42.4) | 8 (8.7) | 21 (22.8) | 3 (3.3) | 1 (1.1) | 6 (6.5) | 3 (3.3) |
| Sub-Saharan Africa | 76 (80.0) | 28 (29.5) | 18 (18.9) | 22 (23.2) | 6 (6.3) | 3 (3.1) | 6 (6.3) | 5 (5.3) |
| South Asia | 58 (58.6) | 57 (57.6) | 8 (8.1) | 28 (28.3) | 7 (7.1) | 2 (2.0) | 12 (12.1) | 3 (3.0) |
| Eastern Europe | 64 (59.3) | 35 (32.4) | 21 (19.4) | 40 (37.0) | 7 (6.5) | 2 (1.8) | 13 (12.0) | 10 (9.3) |
| Far East Asia | 18 (85.7) | 2 (9.5) | 0 (0.0) | 8 (38.1) | 0 (0.0) | 0 (0.0) | 2 (9.5) | 2 (9.5) |
| Latin America | 51 (78.5) | 24 (36.9) | 4 (6.1) | 13 (20.0) | 7 (10.8) | 0 (0.0) | 7 (10.8) | 3 (4.6) |
| Calendar period | ||||||||
| 1985–2002 | 45 (62.5) | 26 (36.1) | 11 (15.3) | 12 (16.7) | 2 (2.8) | 2 (2.8) | 5 (6.9) | 2 (2.8) |
| 2003–2007 | 96 (70.6) | 44 (32.3) | 16 (11.8) | 30 (22.1) | 10 (7.3) | 1 (0.7) | 13 (9.6) | 3 (2.2) |
| 2008–2012 | 181 (66.5) | 115 (42.3) | 32 (11.8) | 90 (33.1) | 18 (6.6) | 5 (1.8) | 28 (10.3) | 21 (7.7) |
| Total | 322 (67.1) | 185 (38.5) | 59 (12.3) | 132 (27.5) | 30 (6.2) | 8 (1.7) | 46 (9.6%) | 26 (5.4%) |
Percentages are computed on the row total (total immigrants for each macro-area of origin).
The associations (odds ratios, ORs) between macro-region of origin, gender, age and sensitisation to grass and HDM in immigrants using logistic regression models.
| Variable | Category | Grass | HDM | ||
|---|---|---|---|---|---|
| OR (CI 95%)a | P value | OR (CI 95%)a | P value | ||
| Gender | Male vs. Female | 1.05 (0.67–1.63) | NS | 0.88 (0.5–3.28) | NS |
| Age (years) | ≤25 | Ref. | Ref | ||
| 25–35 | 1.61 (0.93–2.79) | 0.090 | 0.44 (0.26–0.76) | 0.003 | |
| >35 | 1.39 (0.80–2.40) | NS | 0.34 (0.19–0.58) | <0.001 | |
| Macro-area of origin | Eastern Europe | Ref. | Ref. | ||
| Sub-Saharan Africa | 2.76 (1.45–5.25) | 0.007 | 0.85 (0.46–1.58) | NS | |
| South Asia | 1.02 (0.56–1.86) | NS | 2.71 (1.47–5.01) | 0.001 | |
| North Africa | 1.03 (0.56–1.88) | NS | 1.46 (0.79–2.71) | NS | |
| Latin America | 2.49 (1.22–5.05) | 0.012 | 1.27 (0.66–2.45) | NS | |
The pattern of sensitisation by macro-area of origin was confirmed when restricting the analysis to monosensitised patients (Fig. 2). Immigrants from Sub-Saharan Africa, Latin America and Far East Asia showed a higher prevalence of sensitisation to grass (65.8%, 66.7% and 77.8% respectively), whereas immigrants from North Africa and South Asia were more sensitised to HDM (43.9% and 54.9%, respectively).
Demographic and clinical features in immigrants (n=272) and a random sample of Italians (native-born) (n=731) with a first positive allergy test in 2008–2012 are set out in Table 4. Males were 43.9% of Italians, less than the proportion observed among immigrants from North Africa (P=0.001) and South Asia (P<0.001), but more than among those from Eastern Europe (P=0.007) and Latin America (P=0.001). The mean age was similar in immigrants (34.1 years) and Italians (34.4 years), although most of the former were 26–45 years old (74.3%) whereas Italians showed a more uniform distribution, 20.1% of subjects being over 45 years of age, compared with 8.6% of immigrants (data not shown in table).
Gender, age, and prevalence of asthma and rhinitis and polysensitisation in immigrants, according to macro-area of origin, and in Italians (native-born) with respiratory allergic disease and a first positive test for allergy in 2008–2012.
| Male No. (%) | Age mean (SD) | Asthma No. (%) | Rhinitis No. (%) | Polysensitisation No. (%) | Total No. (%) | |
|---|---|---|---|---|---|---|
| Macro-area of origin | ||||||
| North Africa | 37 (67.3) | 32.5 (8.1) | 25 (45.5) | 52 (94.5) | 22 (40.0) | 55 (100.0) |
| Sub-Saharan Africa | 18 (36.0) | 34.3 (7.3) | 24 (48.0) | 49 (98.0) | 31 (62.0) | 50 (100.0) |
| South Asia | 45 (78.9) | 33.8 (8.3) | 18 (31.6) | 56 (98.3) | 30 (52.6) | 57 (100.0) |
| Eastern Europe | 19 (27.1) | 33.9 (9.9) | 27 (38.6) | 67 (95.7) | 38 (54.3) | 70 (100.0) |
| Far East Asia | 5 (45.4) | 39.1 (9.5) | 2 (18.2) | 10 (90.1) | 6 (54.6) | 11 (100.0) |
| Latin America | 4 (13.8) | 35.5 (10.9) | 11 (37.9) | 29 (100.0) | 18 (62.1) | 29 (100.0) |
| Total immigrants | 128 (47.1) | 34.1 (8.9) | 107 (39.3) | 263 (96.7) | 145 (53.3) | 272 (100.0) |
| Italians | 321 (43.9) | 34.4 (14.1) | 304 (41.6) | 672 (91.3) | 293 (40.1) | 731 (100.0) |
Percentages are computed on the row total (total immigrants for each macro-area of origin).
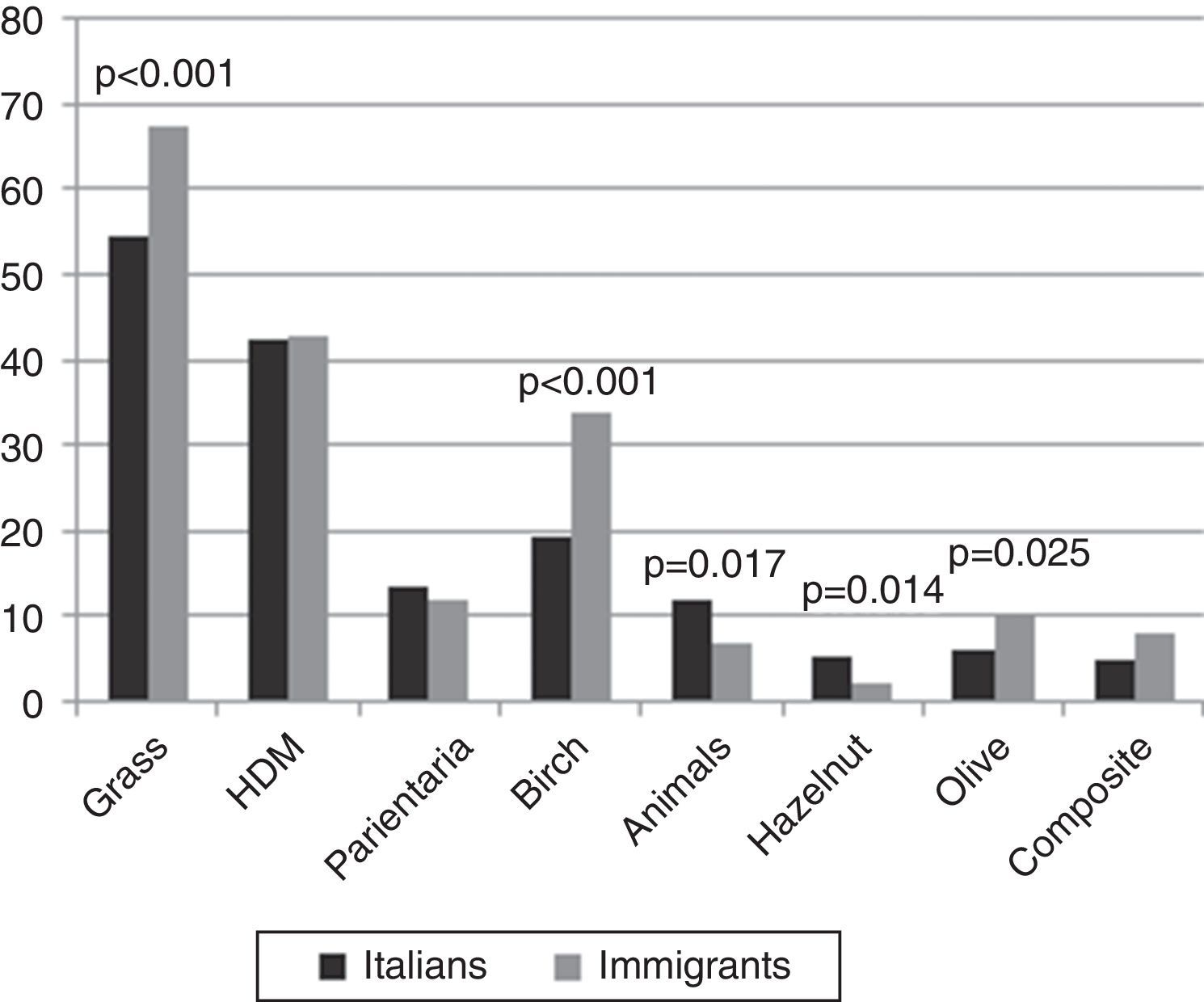
A similar proportion of asthmatic patients was present in the two groups, whereas the proportion of polysensitised subjects was higher in immigrants than in Italians (P<0.001), particularly those from Sub-Saharan Africa and Latin America. The pattern of sensitisation to the different allergens showed statistically significant differences between Italians and immigrants (Fig. 3). Of the three most common allergens, a higher proportion of sensitised subjects was found in immigrants than Italians for grass (67.5% and 54.4%, respectively, P<0.001) and birch (33.6% and 19.4%, respectively, P<0.001), although not for HDM (42.9% and 42.2%, respectively). Minor differences were observed for animals, hazelnut and olive.
A random sample of 52 immigrants with a first positive allergy test in 2006–2012 were interviewed by telephone. Forty-eight of them (92.3%) claimed that the allergy symptoms had appeared after their arrival in Italy, with a mean period of residence in Italy before the onset of allergy of 6.27 years (5.14–7.40).
DiscussionOur study showed a relatively high prevalence of respiratory allergy in adult immigrants living in the province of Brescia, a very polluted area in North Italy, with factories and farms, and a higher proportion of immigrants than the national average. About 150,000 official immigrants, including children, corresponding to 12.2% of the total population of 1.2 million, were living in the province of Brescia in 2009, compared to 6.5% in Italy as a whole.9
A sharp increase in the number of immigrants coming to the Allergy Unit due to respiratory allergy was found from the 1980s to the 2000s, parallel to the increase in immigrants coming to the province of Brescia in the period, suggesting that the increase in the absolute number of immigrants with respiratory allergy in recent decades depends mostly on the increase in immigrants living in the area and their length of stay.
The adult immigrant population was 11.9% of the adult population living in the area (975,232 inhabitants) in 2009. The distribution of immigrants with respiratory allergy by macro-area of origin is substantially similar to that of immigrant population, as shown in Table 5. Some differences, however, were noted: people from Eastern Europe were under-represented in the former group (25.4% vs. 37.0%), whereas those from Sub-Saharan Africa and Latin America were over-represented (18.3% vs. 13.2% and 10.8% vs. 3.6%, respectively). A selection bias of immigrants with respiratory allergy by area of origin seems unlikely, since all immigrants, including illegal ones, have access to free health care at any public hospital in Italy. These findings therefore suggest that immigrants from Eastern Europe have a lower, and those from Sub-Saharan Africa and Latin America a higher frequency of allergic disease than expected based on the distribution of the immigrant population living in the area, although further research is needed to confirm this hypothesis. A higher frequency of allergic disease in immigrants from Latin America has been observed in other studies in Italy.7,10
Immigrants with respiratory allergy and immigrant adult population living in the province of Brescia by macro-area of origin in 2009.
| Immigrants with respiratory allergy | Immigrant population | |||
|---|---|---|---|---|
| No. subjects | (%) | No. subjects | (%) | |
| Macro-area of origin | ||||
| North Africa | 55 | (20.5) | 21388 | (19.3) |
| Sub-Saharan Africa | 49 | (18.3) | 14601 | (13.2) |
| South Asia | 57 | (21.3) | 24968 | (22.5) |
| Eastern Europe | 68 | (25.4) | 41113 | (37.0) |
| Far East Asia | 10 | (3.7) | 4926 | (4.4) |
| Latin America | 29 | (10.8) | 4032 | (3.6) |
| Immigrants | 272 | (100) | 115785a | (100) |
Percentages per macro-area are computed on the total immigrants.
We found substantial differences in demographic characteristics between immigrants and Italians (native-born people) and among immigrants according to area of origin. Although no difference was found between immigrants and Italians in terms of mean age (34.1 vs. 34.4 years), Italians showed a more uniform age distribution, and a higher proportion of subjects aged over 45 years compared to immigrants (20.1% vs. 8.6%). These data are in agreement with other recent studies in Italy,4,7 which found that the mean age of immigrants was 30–35 years, because most of them are first-generation immigrants, who came to Italy to seek work. The male:female ratio in immigrants varied significantly by areas of origin: males were the majority of people from North Africa and South Asia, but the minority of those from East Europe and Latin America. Again, this is mostly due to the job that immigrants usually have in Italy according to their country of origin: housekeepers and nurses most commonly come from East Europe, peasants and farm hands from India, and factory workers from North Africa and South Asia.
In our study almost all the immigrants had rhinitis and 44.2% bronchial asthma, a proportion similar to that seen in Italians, in agreement with some7 European and Italian studies, although others reported a higher5,6,10,11 or a lower12 proportion of asthma in immigrants. A large Italian study using questionnaires13 found a lower prevalence of asthma in immigrant children compared to children born in Italy. This comparison is hampered, however, by the different prevalence of asthma in the country of origin and in the host country or both, although age at immigration and duration of stay in the host country seem to play a major role in asthma prevalence in immigrants,13–16 according to the proposed hypothesis of a role of epigenetics in the developmental origins of allergic disease.17
The pattern of sensitisation showed certain similarities but also differences between immigrants according to macro-area of origin and between immigrants and Italians.
A comparison between immigrants and Italians showed a higher frequency of polysensitisation in the former than the latter (54.5% vs. 41.6%) in the most recent period. It is noteworthy, however, that the proportion of polysensitised immigrants increased from 1985–2002 to 2003–2007 and 2008–2012. This is probably due to the fact that immigrants with respiratory allergy diagnosed in more recent years have been living in Italy longer than those assessed previously, and therefore have a longer duration of exposure to new allergens; it is well known that the longer the exposure time, the greater the tendency to become sensitised to more allergens.3
Among the immigrants, a higher proportion of subjects with polysensitisation was found among those from Sub-Saharan Africa (61.2%) and Eastern Europe (58.8%) compared to those from other areas.
Immigrants were mainly sensitised to the most common Italian allergens, i.e. grass and HDM, in agreement with other studies showing that immigrants are usually sensitised to allergens of the host country.4–7,12,18,19 However, immigrants showed a higher proportion of subjects sensitised to grass and birch, and minor difference for the other allergens, compared with Italians, in agreement with another recent study performed in North Italy.4 Furthermore, significant differences were found according to macro-area of origin: grass sensitisation was more common among immigrants from Sub-Saharan Africa, Far East Asia and Latin America than those from the other areas whereas frequency of HDM sensitisation was higher among immigrants from South Asia than those from other areas. This different pattern is similar to that seen in other studies performed in Italy.4–7
These findings may be due to various factors. In the host country, immigrants may be exposed to pollens they had never or less frequently met in their origin country, or to pollens already met, but that in the new environment are present in higher concentrations or together with chemicals with a more sensitising potential, i.e. diesel exhaust,20 or to pollens belonging to the same family and therefore highly cross-reactive, as shown by a recent study describing cross-reactivity between Indian and Italian common pollen allergens.21
The subtropical grasses are abundant in warmer regions including parts of Africa, India, Asia, as well as Central and South America22,23 and their distribution is likely to increase with pollution and global warming.24 Furthermore, Frenguelli et al.25 showed that late summer peaks in airborne grass pollen were observed to coincide with flowering of subtropical grasses including Cynodon dactylon in Italy. On the other hand, the higher HDM sensitisation among South Asia immigrants is in agreement with the fact that HDM and cockroaches are the most common allergens causing sensitisation in India.26
Finally, also shifts in composition of the intestinal microbiota caused by antibiotic use and dietary changes which may occur in immigrants moving to Western countries may lead to the development of atopic disease through a disruption in immune tolerance, as recently suggested.27,28
Overall, these findings suggest that exposure to allergens and possibly to inflammatory or sensitising agents in both origin and host country contribute to the pattern of sensitisation in immigrants in line with the endless debate of the role played by genetic background and environmental factors in allergy diseases. To evaluate the role of these factors in developing allergy in immigrants, more research is needed, possibly with a prospective design with enrolment of immigrants at the start of their coming to the host country.
Some limits of our study should be considered. First, as immigrants may attend other allergy clinics in our and other provinces, our hospital-based case-series depends on the hospital catchment area. Consequently, the increase in the number of immigrants observed at our centre from 1985 to 2011 may be due to an increase in the number of immigrants with allergic diseases, or to an increase in or those coming to our centre for their first allergy test, or both. However, the demographic and clinical characteristics, the sensitisation pattern and the distribution of subjects by country of origin in our study are similar to those observed in recent years in other allergy centres located in our5 and adjacent4,7 areas.
In conclusion, our study confirms that migration to a highly industrialised Western country favours the development of respiratory allergy in immigrants; that immigrants tend to develop sensitisation to local allergens and polysensitisation. However, some differences in the pattern of sensitisation according to country of origin suggest that also genetic factors or allergen exposure in the first years of life may play a role in developing atopy and allergic disease in immigrants.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
FundingNo funds were allocated for the study.
Conflict of interestThe authors declare they have no conflicts of interest.