There is no conclusive evidence regarding the effect of fasting on different features in asthmatic patients. In the present study, the effect of Ramadan fasting in asthmatic patients and healthy control was studied.
MethodsHaematological indices, inflammatory mediators, pulmonary function tests (PFT) and respiratory symptoms were evaluated in 15 asthmatic patients compared to 14 healthy matched control group before and after the one-month fasting period in Ramadan. The change in each parameter from the beginning to the end of Ramadan was calculated and referred to as “variation during Ramadan”.
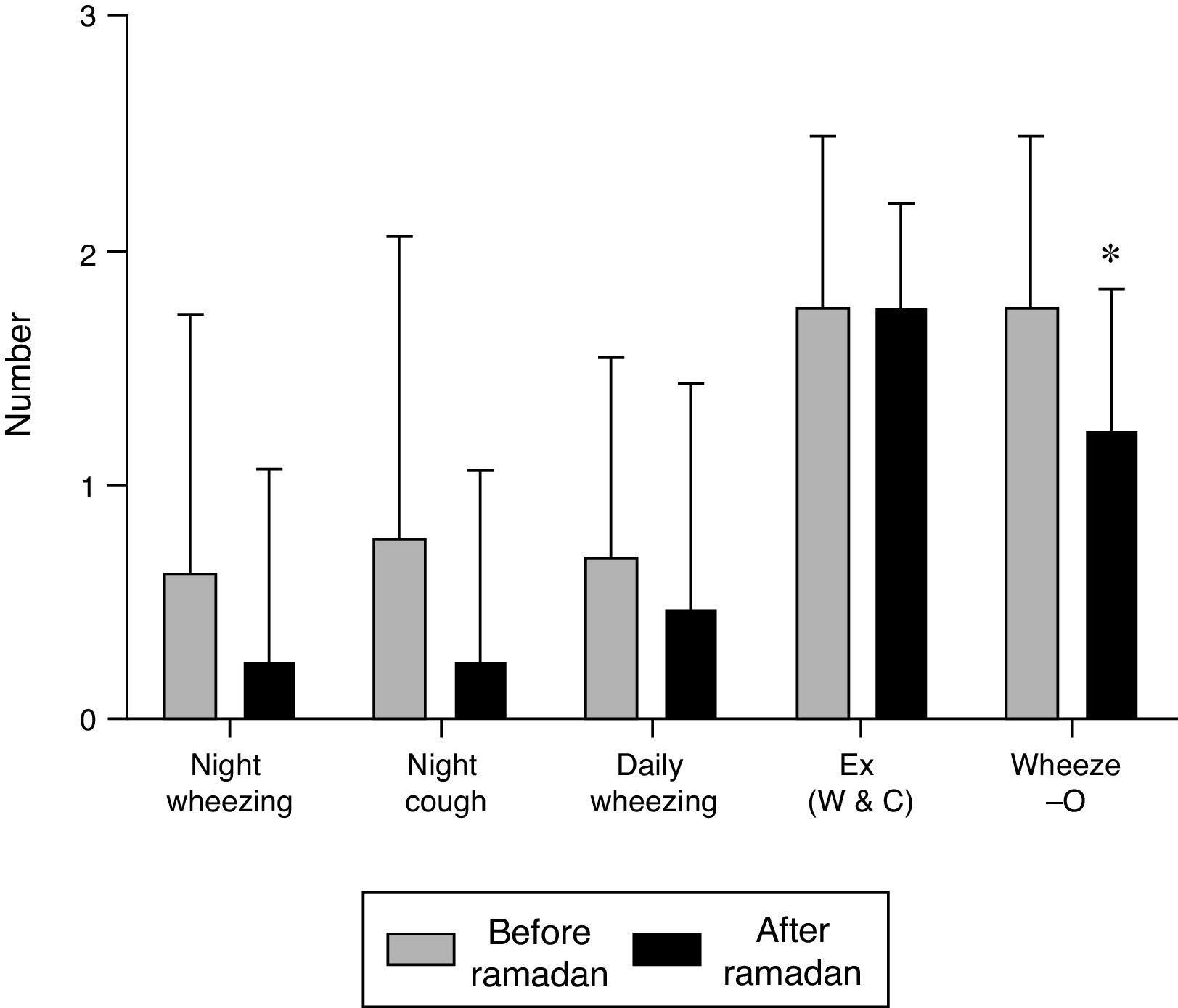
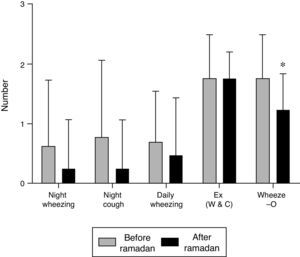
ResultsThe values of MCH, MCHC in both groups and monocyte counts in asthmatic patients, were significantly increased but platelet count was reduced in asthmatic and controls respectively compared to pre-Ramadan fasting period (P<0.05 to 0.001). Serum hs-CRP level in control and asthmatic groups was significantly reduced after Ramadan fasting month (P<0.001 for both groups). PFT values after Ramadan fasting month in both groups were non-significantly higher compared to pre-fasting values except FVC. Respiratory symptoms in asthmatic patients were non-significantly but wheeze-o was significantly reduced after Ramadan fasting period in asthma group (P<0.05). There was no significant difference in variations of different parameters during Ramadan fasting period between two groups, although reduction of hs-CRP in asthmatic group was non-significantly higher than control group.
ConclusionThese results show that Ramadan fasting period has no negative impact on asthma and may have some positive effect on asthma severity with regard to reduction of hs-CRP concentration and chest wheeze.
The holy Ramadan is the 9th month of the lunar calendar (Hejri), including 29–30 days. Ramadan has importance and great social value among Muslims all over the world that restrict them from some tasks consisting of drinking, eating, smoking, and sexual relationships, from pre sun rise (Sahar) to post sun set (Iftar).1,2 Because the duration of the lunar year (354 days) is lower than the Gregorian year (365 days), fasting time is variable3 from 12 to 18h and even 22h each day, depending on the geographical area, season and country; the end of spring, beginning of summer, the tropics and temperate locations being longer.4,5 However, in some conditions Muslims are exempt from fasting including; travelling, pregnancy, menstruation, breast-feeding women, patients given medication via oral and parenteral, sickness, pre-pubertal and pubertal children.6,7 Nevertheless, medicines used through breathing and inhalation route do not cancel this duty.
Asthma is a chronic and one of the most common respiratory diseases. Based on the Global Initiative for Asthma (GINA) report, the number of people who are suffering from asthma is more than 300 million.8 Likewise, according to the Iranian Asthma Society, the prevalence of asthma in the Iranian population is estimated to be about 8–12%,9 while in Mashhad and Isfahan, two large cities of Iran, it was reported as 2.8% of total population10 and 7.3% of high school children,11 respectively. Asthma is a complex respiratory condition with inflammation, hyper responsiveness, obstruction and remodelling of the airways. The nature of airway obstruction in asthma is fully or partially reversible.12
All guidelines for treatment of asthma suggest orderly use of medicines for relieving symptoms and prevention of development of disease, such as monitoring and education of patients as well as avoiding of risk factors. Correlation between health and various religious rituals is an important issue, but only limited, inadequate or controversial studies are available in this regard.2
The effect of one month fasting during Ramadan on various aspect of asthma was examined in several previous studies. Increased peak expiratory flow (PEF) due to one month fasting in asthmatic patients13 as well as maximal expiratory flow at 75% and 75–85% of vital capacity (MEF75, MEF75–85 respectively) in healthy subjects14 was shown previously. However, the absence of the effect of fasting in Ramadan on PFT values in asthmatic patients was demonstrated in another study.15 The effect of fasting and decrease in food intake on weight loss can decrease the constriction of airways,16 lead to changes in surfactant and elastin metabolism,17 increase in catecholamine which can cause airway dilation, as well as decreasing stomach volume and gastro oesophageal reflux18 all postulated as the possible mechanisms of fasting on asthmatic patients and PFT values. However, a change in circulating inflammatory mediators could be another possible mechanism responsible for the effect of one month fasting in Ramadan on asthmatic patients and PFT values.
Therefore, in the present study, the impact of Ramadan fasting period on respiratory symptoms, pulmonary function tests (PFT), haematological indices, total and differential white blood cells and inflammatory biomarkers on healthy and asthma subjects were examined.
Material and methodsSubjectsFourteen healthy volunteers (mean age±SD; 37.5±7.86 year, mean height±SD; 175.66±12.11cm) and fifteen asthmatic patients (mean age±SD; 49.28±12.54 year, mean height±SD; 166.38±8.66cm) with moderate to severe disease according to GINA guideline19 were studied with the following inclusion and exclusion criteria: (1) previously diagnosed with asthma by a physician; (2) two or more of the following symptoms: recurrent wheeze, cough or chest-tightness at rest; nocturnal or early morning wheeze, cough or chest-tightness; and wheeze or cough during exercise, (3) FEV1 and PEF less than 80% predicted values; (4) no history or symptoms of cardiovascular or other respiratory diseases that required treatment (excluding the common cold). Control subjects were healthy volunteers and had no history of respiratory complaints. Excluding criteria were: recent respiratory infection, chest X-ray (CXR) abnormality, smoking, high blood pressure and diabetes. Patients received their regular medications during the study period. The study was approved by the Ethical Committee of the Mashhad University of Medical Sciences (Code: 930520), and all subjects gave informed consent.
Blood sampling and assessment of haematological parametersTen millilitres of blood was collected from each control and asthma subject twice: (1) three to five days before and (2) after the end of Ramadan.
High sensitivity C-reactive protein (hs-CRP), an index of inflammation, was quantified using commercially available specific Enzyme Linked Immune Absorbent Assays (ELISA) according to the manufacturer's protocol (Antibodies-online; Catalog Number: ABIN366539).
Total red blood cell (RBC) and white blood cells (WBC) were counted in duplicate in a haemocytometer (in a Burker chamber) in blood stained with Turk solution (1:10 dilution, consisting of 1ml of glacial acetic acid, 1ml of gentian violet solution 1% and 100ml distilled).
Differential cell counts were done on thin smeared blood sample, using Wright-Giemsa's stain. According to staining and morphological criteria, differential cell analysis was carried out under a light microscope by counting 100 cells, and the percentage of each cell type was calculated.
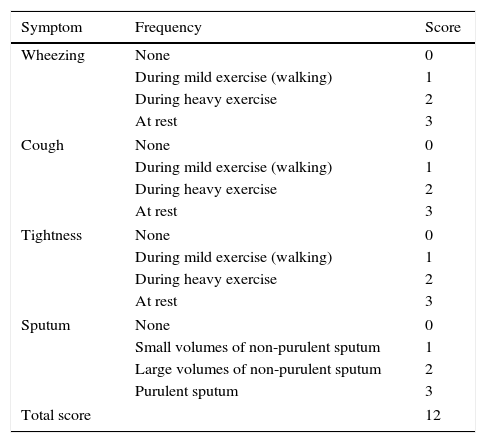
Evaluation of respiratory symptoms and pulmonary function testsA Farsi questionnaire was used to assess the prevalence and severity of respiratory symptoms (wheezing, tightness, cough and sputum) (Table 1). The questionnaire on respiratory symptoms was designed in accordance with several previous questionnaires of similar studies by expert groups.6,8,10,20,21 Common risk factors like smoking habit, atopy and history of allergic reactions were also assessed. The degree of wheezing on chest examination (objective wheezing=wheeze-o) was considered between 0 and 3 as follows: no wheezing=0, hardly heard wheezing=1, moderate wheezing=2 and loud wheezing=3.
The criteria for respiratory symptom severity score.
| Symptom | Frequency | Score |
|---|---|---|
| Wheezing | None | 0 |
| During mild exercise (walking) | 1 | |
| During heavy exercise | 2 | |
| At rest | 3 | |
| Cough | None | 0 |
| During mild exercise (walking) | 1 | |
| During heavy exercise | 2 | |
| At rest | 3 | |
| Tightness | None | 0 |
| During mild exercise (walking) | 1 | |
| During heavy exercise | 2 | |
| At rest | 3 | |
| Sputum | None | 0 |
| Small volumes of non-purulent sputum | 1 | |
| Large volumes of non-purulent sputum | 2 | |
| Purulent sputum | 3 | |
| Total score | 12 | |
Pulmonary function tests in asthmatic and control subjects were measured using a spirometer with a pneumotachograph sensor (Model ST90, Fukuda, Sangyo Co., Ltd., Japan). Prior to pulmonary function testing, the PFT measurement technique was demonstrated by the operator, and subjects were encouraged and supervised throughout test performance. Pulmonary function testing was performed using the acceptability standards outlined by the American Thoracic Society (ATS),22 with subjects in a standing position and wearing nose clips. Pulmonary function tests were performed three times in each subject. The highest level for forced vital capacity (FVC), forced expiratory volume in one second (FEV1), peak expiratory flow (PEF), maximal mid expiratory flow (MMEF) and maximal expiratory flow at 75%, 50%, and 25% of the FVC (MEF75, MEF50, and MEF25 respectively) were taken independently from the three measurements. All tests were also carried out in two time periods: (1) 3–5 days before starting Ramadan and (2) after the end of fasting period for 29/30 days.
StatisticsAccording to previous studies regarding the various effects of fasting in Ramadan, using the PPS sampling method, it was calculated that a minimum of 14 subjects in each group would be needed to detect a 4% difference with an α error of 1% and a power of 95%. The data of age, PFT values, haematological indices and serum concentration of hs-CRP were expressed as mean±SD and data of respiratory as percentage of each group having the corresponding symptom. Differences in the data of symptoms between asthmatic patients and healthy control group were tested by Chi-Squared analysis (2X2 contingency tables). The data of PFT values, haematological indices and serum concentration of hs-CRP between asthmatic and control groups were tested using unpaired t tests. Comparison of PFT values, haematological indices and serum concentration of hs-CRP between pre and post Ramadan fasting period in each group was tested using paired t tests. A two-sided P value of 0.05 was the criterion for statistical significance. All analyses were performed with SPSS software (version 11.5, SPSS Inc., USA).
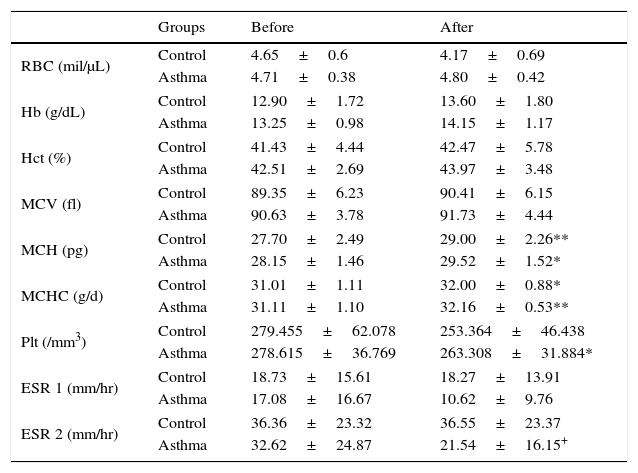
ResultsThe effects of Ramadan fasting on haematological parametersIn the healthy control group the values of RBC, platelet (Plt) and ESR 1 were decreased after the Ramadan fasting period, but these decrements were not statistically significant. However, the values of MCH and MCHC were significantly increased compared to pre-Ramadan fasting period (P<0.05 to 0.001, Table 1).
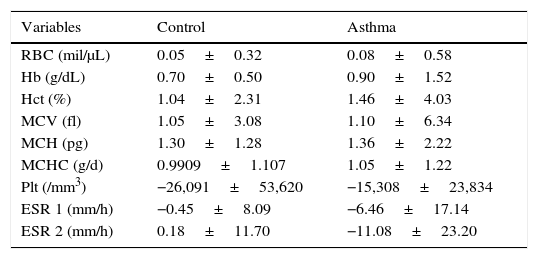
In the asthmatic group the MCH, MCHC values were also significantly increased but platelets were reduced compared to pre-Ramadan fasting period (P<0.05 to 0.001, Table 1). ESR 2 value was lower in asthmatic patients compared to healthy control group after the Ramadan fasting period (P<0.05, Table 1). There was no statistical difference in variations of haematological indices between asthmatic and healthy group during Ramadan (Table 3).
Comparison of haematological indices variations between asthmatic and healthy group during Ramadan.
| Variables | Control | Asthma |
|---|---|---|
| RBC (mil/μL) | 0.05±0.32 | 0.08±0.58 |
| Hb (g/dL) | 0.70±0.50 | 0.90±1.52 |
| Hct (%) | 1.04±2.31 | 1.46±4.03 |
| MCV (fl) | 1.05±3.08 | 1.10±6.34 |
| MCH (pg) | 1.30±1.28 | 1.36±2.22 |
| MCHC (g/d) | 0.9909±1.107 | 1.05±1.22 |
| Plt (/mm3) | −26,091±53,620 | −15,308±23,834 |
| ESR 1 (mm/h) | −0.45±8.09 | −6.46±17.14 |
| ESR 2 (mm/h) | 0.18±11.70 | −11.08±23.20 |
Values presented as mean±SD (for health and asthmatic group, n=14 and 15, respectively). Un-paired t test was performed and P<0.05 considered as statistically significant.
Abbreviations: RBC, red blood cell; Hb, haemoglobin; Hct, haematocrit; MCV, mean corpuscular volume; MCH, mean corpuscular haemoglobin; MCHC, mean corpuscular haemoglobin concentration; Plt, platelets; ESR, erythrocyte sedimentation rate.
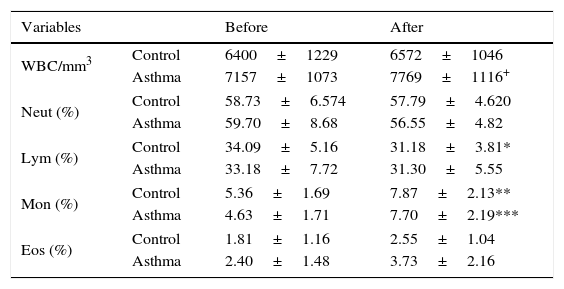
In the healthy group, total WBC and eosinophil non-significantly and monocyte significantly increased (P<0.01) but lymphocyte was reduced (P<0.05) after Ramadan compared to pre-fasting period (Table 4).
Comparison of total and differential white blood cells before and after Ramadan.
| Variables | Before | After | |
|---|---|---|---|
| WBC/mm3 | Control | 6400±1229 | 6572±1046 |
| Asthma | 7157±1073 | 7769±1116+ | |
| Neut (%) | Control | 58.73±6.574 | 57.79±4.620 |
| Asthma | 59.70±8.68 | 56.55±4.82 | |
| Lym (%) | Control | 34.09±5.16 | 31.18±3.81* |
| Asthma | 33.18±7.72 | 31.30±5.55 | |
| Mon (%) | Control | 5.36±1.69 | 7.87±2.13** |
| Asthma | 4.63±1.71 | 7.70±2.19*** | |
| Eos (%) | Control | 1.81±1.16 | 2.55±1.04 |
| Asthma | 2.40±1.48 | 3.73±2.16 | |
Values presented as mean±SD (for health and asthmatic group, n=14 and 15, respectively).
Abbreviations: WBC, white blood cell; Neut, neutrophil; Lym, lymphocyte; Mon, monocyte; Eos, eosinophil.
* P<0.05, ** P<0.01, *** P<0.001 compared to pre-Ramadan fasting period in each group using paired t test.
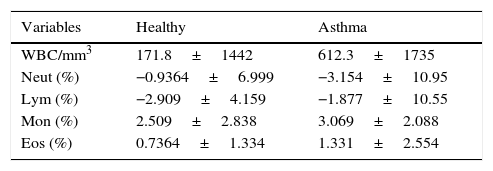
In asthma subjects, post Ramadan total WBC and eosinophil were increased, neutrophil and lymphocyte were declined non-significantly but monocyte count was increased significantly (P<0.001) and eosinophil non-significantly as compared to prior Ramadan fasting period (Table 4). Total WBC count was significantly higher (P<0.05, Table 2) in asthmatic patients compared to healthy control group after Ramadan fasting period (P<0.05, Table 4). In addition, the variations of lymphocyte and eosinophil in asthmatic group during Ramadan fasting period were higher, but neutrophil and monocyte were non-significantly lower than the healthy control group (Table 5).
Comparison of haematological indices before and after Ramadan fasting period in healthy and asthmatic group.
| Groups | Before | After | |
|---|---|---|---|
| RBC (mil/μL) | Control | 4.65±0.6 | 4.17±0.69 |
| Asthma | 4.71±0.38 | 4.80±0.42 | |
| Hb (g/dL) | Control | 12.90±1.72 | 13.60±1.80 |
| Asthma | 13.25±0.98 | 14.15±1.17 | |
| Hct (%) | Control | 41.43±4.44 | 42.47±5.78 |
| Asthma | 42.51±2.69 | 43.97±3.48 | |
| MCV (fl) | Control | 89.35±6.23 | 90.41±6.15 |
| Asthma | 90.63±3.78 | 91.73±4.44 | |
| MCH (pg) | Control | 27.70±2.49 | 29.00±2.26** |
| Asthma | 28.15±1.46 | 29.52±1.52* | |
| MCHC (g/d) | Control | 31.01±1.11 | 32.00±0.88* |
| Asthma | 31.11±1.10 | 32.16±0.53** | |
| Plt (/mm3) | Control | 279.455±62.078 | 253.364±46.438 |
| Asthma | 278.615±36.769 | 263.308±31.884* | |
| ESR 1 (mm/hr) | Control | 18.73±15.61 | 18.27±13.91 |
| Asthma | 17.08±16.67 | 10.62±9.76 | |
| ESR 2 (mm/hr) | Control | 36.36±23.32 | 36.55±23.37 |
| Asthma | 32.62±24.87 | 21.54±16.15+ | |
Values presented as mean±SD (for health and asthmatic group, n=14 and 15, respectively).
Abbreviations: RBC, red blood cell; Hb, haemoglobin; Hct, haematocrit; MCV, mean corpuscular volume; MCH, mean corpuscular haemoglobin; MCHC, mean corpuscular haemoglobin concentration; Plt, platelets; ESR, erythrocyte sedimentation rate; Control, healthy group; Asthma, asthmatic group.
* P<0.05, **P<0.01 compared to pre-Ramadan fasting period in each group using paired t test.
Comparison of total and differential white blood cells variation between asthmatic and healthy group during Ramadan.
| Variables | Healthy | Asthma |
|---|---|---|
| WBC/mm3 | 171.8±1442 | 612.3±1735 |
| Neut (%) | −0.9364±6.999 | −3.154±10.95 |
| Lym (%) | −2.909±4.159 | −1.877±10.55 |
| Mon (%) | 2.509±2.838 | 3.069±2.088 |
| Eos (%) | 0.7364±1.334 | 1.331±2.554 |
Values presented as mean±SD (for health and asthmatic group, n=14 and 15, respectively). Un-paired t test was performed and there was not statistically significant.
Abbreviations: WBC, white blood cell; Neut, neutrophil; Lym, lymphocyte; Mon, monocyte; Eos, eosinophil.
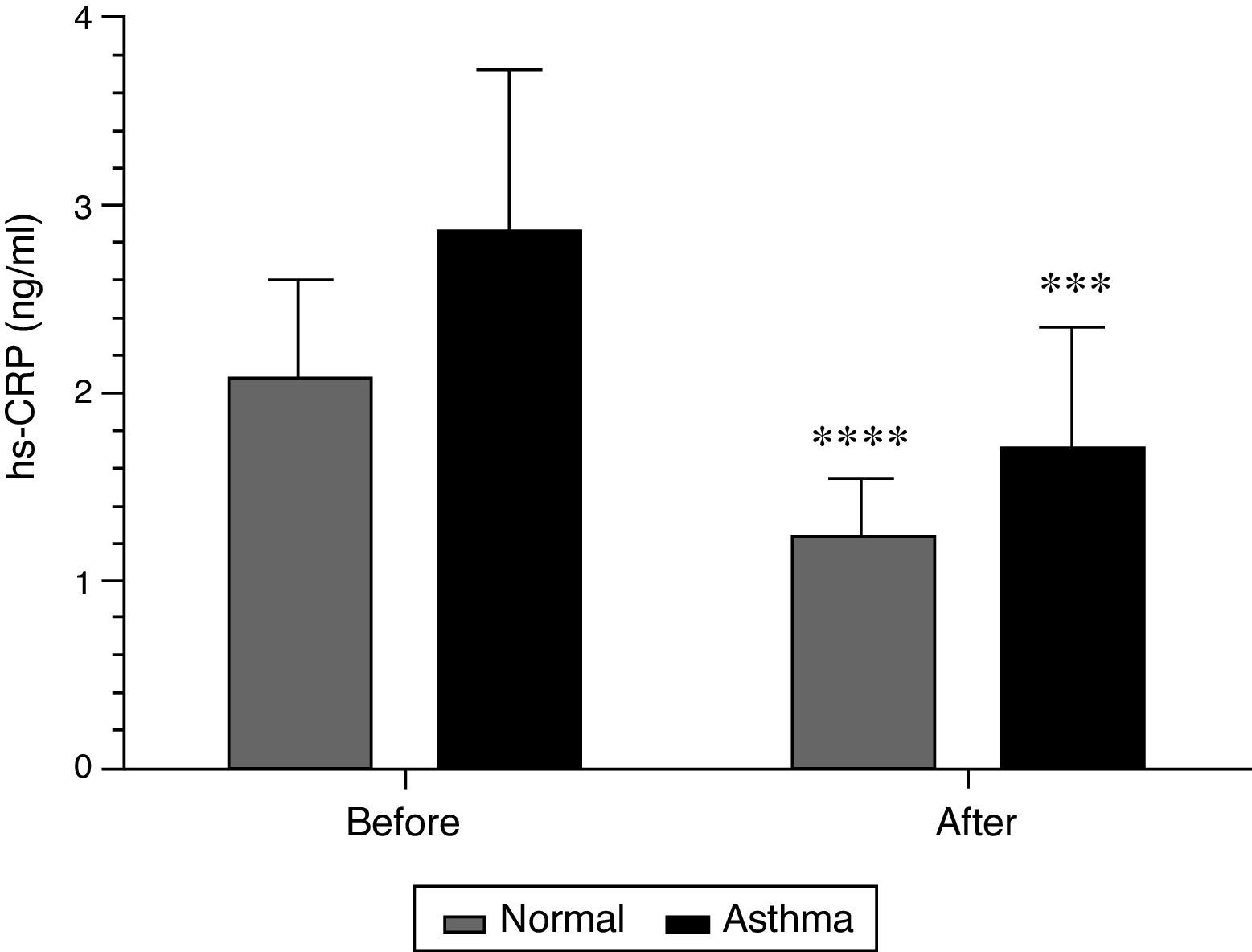
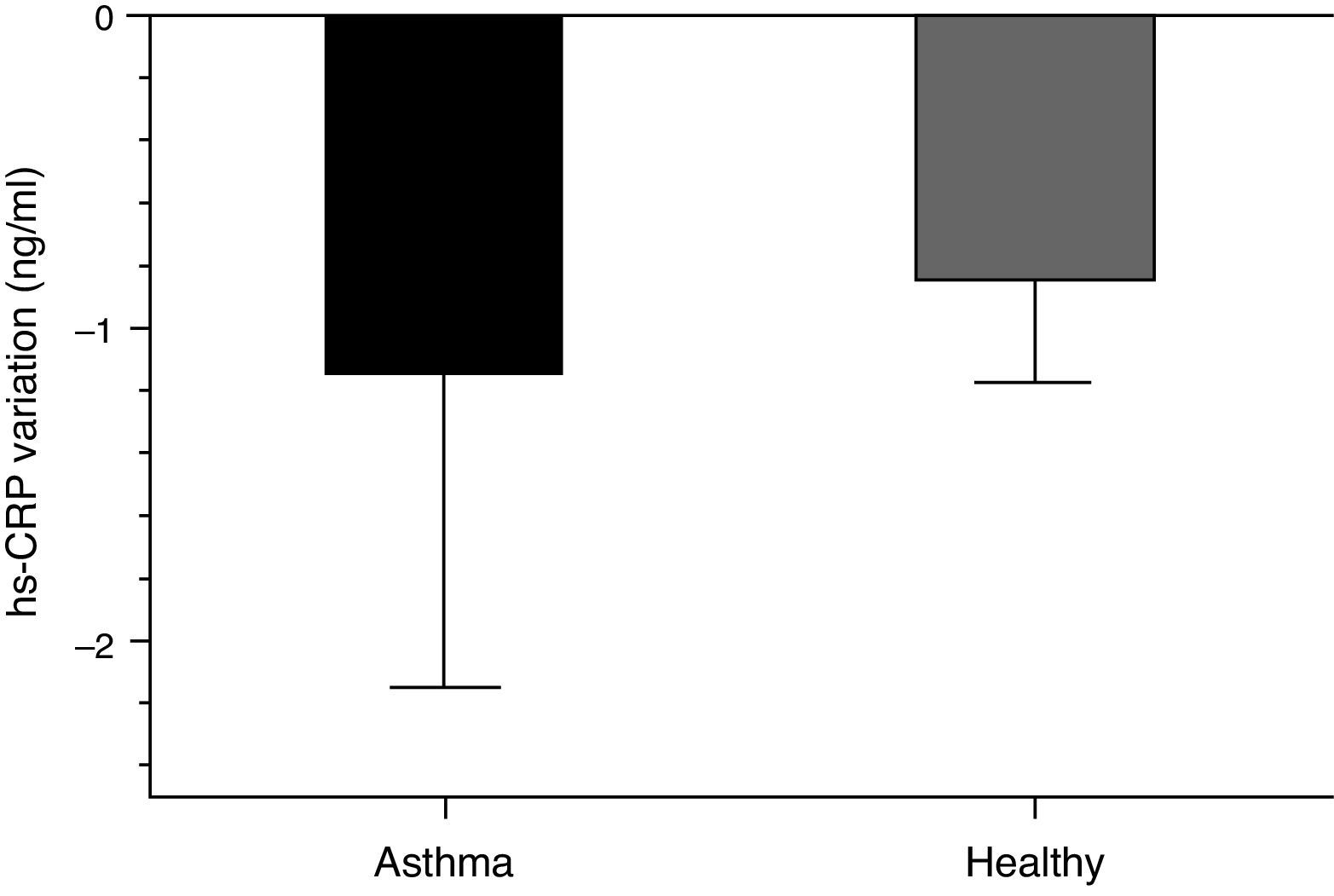
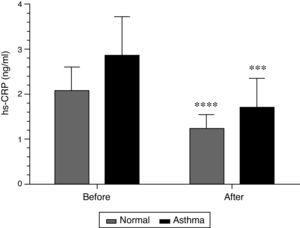
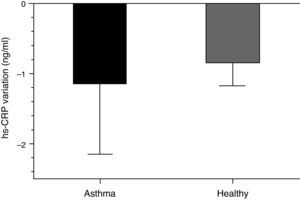
Serum hs-CRP concentration in healthy group was 2.08±0.52 and 1.24±0.29ng/ml before and after Ramadan, respectively (P<0.001). The value of hs-CRP in asthmatic patients was also significantly reduced after Ramadan fasting month, (2.86±0.82 vs. 1.71±0.63ng/ml, P<0.001, Fig. 1). Variation of hs-CRP of in the asthmatic group during Ramadan fasting period (−1.14±0.008ng/ml) was non-significantly higher than control group (−0.083±0.337ng/ml, Fig. 2).
Comparison of hs-CRP serum concentration between asthmatic and healthy control group before and after Ramadan (for health and asthmatic group, n=14 and 15, respectively). Values presented as mean±SD. *P<0.05, **P<0.01, ***P<0.001 and ****P<0.0001, compared to pre-Ramadan fasting period in each group using paired t test.
Comparison of hs-CRP serum concentration variation between asthmatic and healthy control group before and after Ramadan (for control and asthmatic group, n=14 and 15, respectively). Values presented as mean±SD. There was no significant difference between asthmatic and control group.
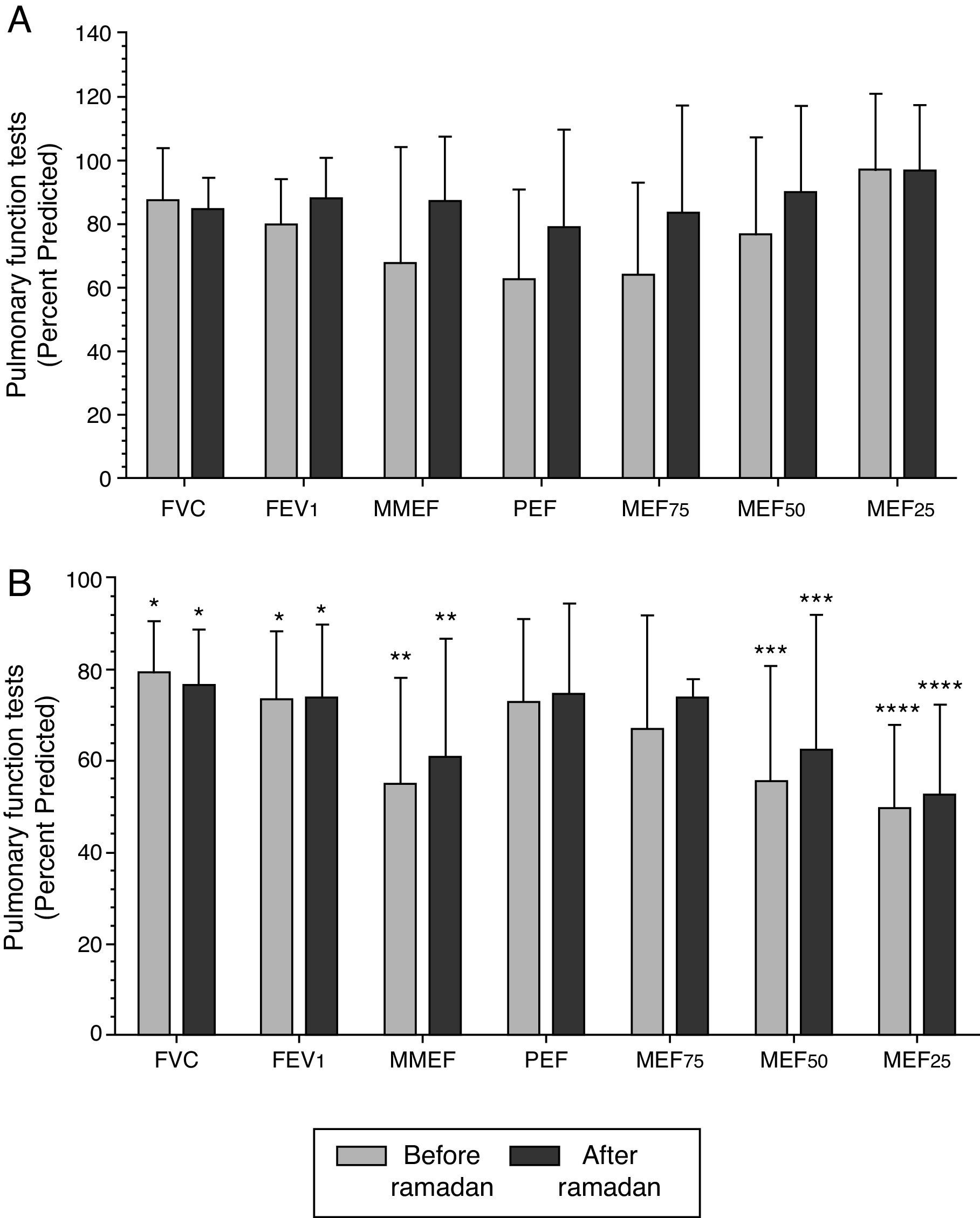
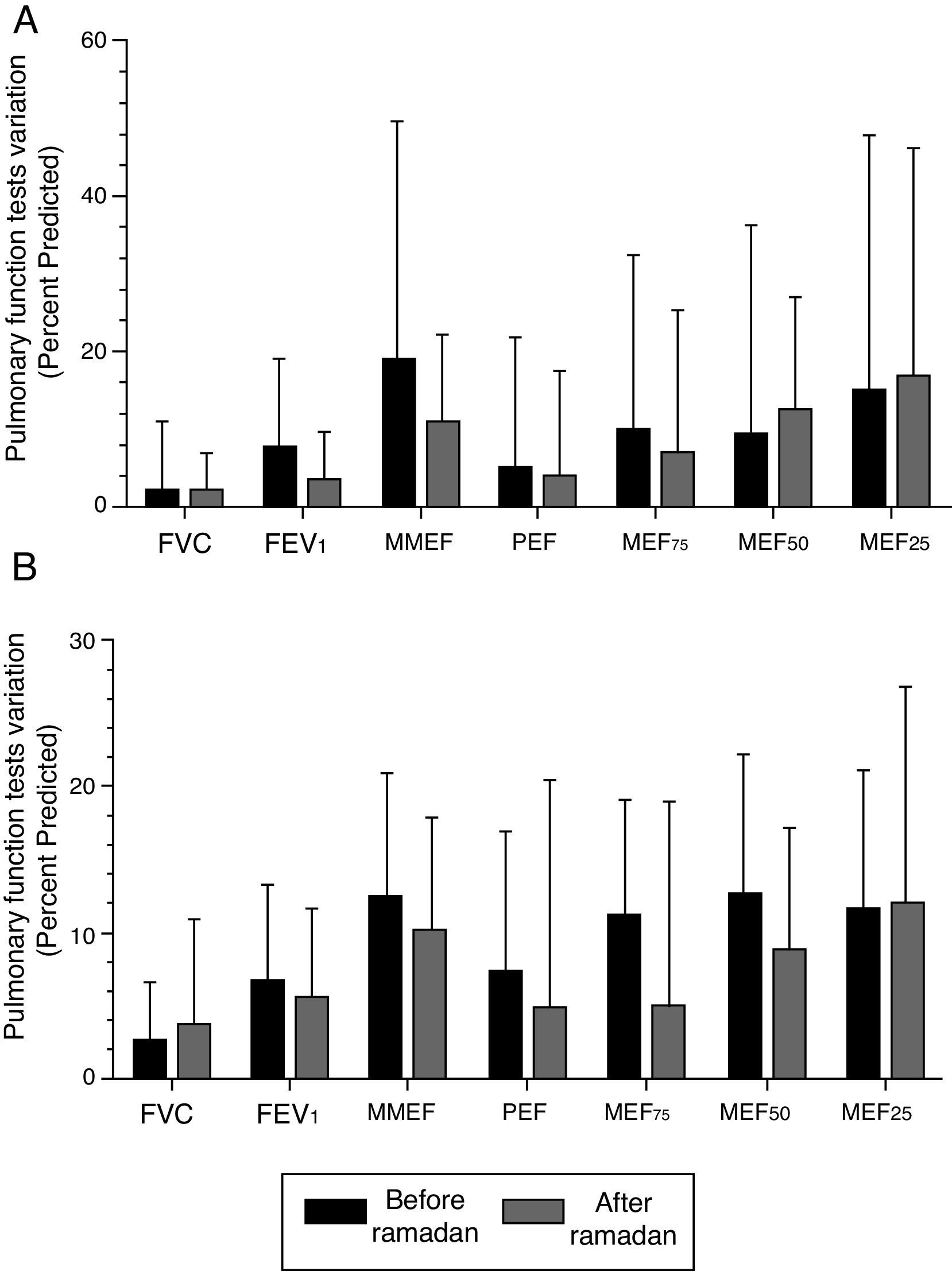
Most PFT values both prior and post fasting period in Ramadan were significantly lower in asthmatic patients compared to the healthy control group (P<0.05 to P<0.0001, Fig. 3). PFT values after Ramadan fasting month in both groups were non-significantly higher compared to pre-fasting values (Fig. 4). In addition, there were no significant differences in PFT variations during fasting period in Ramadan between asthmatic patients and healthy control group (Fig. 4).
Comparison of pulmonary function tests (PFT) between before and after Ramadan fasting period in healthy control group (A, n=14) and asthma patient (B, n=15). Values presented as mean±SD. Paired t-test was performed between each group and un-paired t-test performed in comparison to healthy control group. *P<0.05, **P<0.01, ***P<0.001 and ****P<0.0001 compared to healthy control group. Abbreviations: FVC, forced vital capacity; FEV1, forced expiratory volume in one second; MMEF, maximal mid expiratory flow; PEF, peak expiratory flow; MEF75, MEF50, and MEF25, maximal expiratory flow at 75%, 50%, and 25% of the FVC, respectively.
Comparison of pulmonary function tests (PFT) variation before and after Ramadan in healthy control group (A, n=14) and asthma patient (B, n=15). Values presented as mean±SD. Paired t-test was performed for each parameter. Abbreviations: FVC, forced vital capacity; FEV1, forced expiratory volume in one second; MMEF, maximal mid expiratory flow; PEF, peak expiratory flow; MEF75, MEF50, and MEF25, maximal expiratory flow at 75%, 50%, and 25% of the FVC, respectively.
Night cough, night and daily wheeze in asthmatic patients were non-significantly reduced after one month fasting during Ramadan (Fig. 5). However, wheeze-o was reduced significantly after Ramadan fasting period in asthma group (P<0.05, Fig. 5).
DiscussionIn the present study the effect of the one-month fasting period during Ramadan on haematological and inflammatory indices as well as on respiratory symptoms and PFT values in asthmatic patients compared to healthy control group was studied.
In healthy control and asthmatic groups, the values of MCH, MCHC and monocyte counts were significantly increased compared to pre-Ramadan fasting period. Lymphocyte and platelet count were also reduced compared to pre-Ramadan fasting period in controls and asthmatics, respectively. Total WBC count was also non-significantly increased during fasting period in Ramadan in both groups. ESR 2 value was lower but total WBC count was higher in asthmatic patients compared to healthy control group after Ramadan fasting period. In addition, there was no statistical difference in variations of haematological indices between asthmatic and healthy group during Ramadan. In 38 males and 44 females, aged 29–70 year, with a previous history of either coronary artery disease, metabolic syndrome or cerebro-vascular disease, there was a significant higher high- density lipoprotein-cholesterol (HDL-C), WBC, RBC and Plt count, and lower plasma cholesterol (Chol), triglycerides (TG), low-density lipoprotein-cholesterol (LDL-C), very-low-density lipoprotein (VLDL-C) after one month fasting during Ramadan.23 The results of a previous study showed that platelet count was significantly decreased during Ramadan while other parameters including haemoglobin, haematocrit, red blood cell count remained relatively stable in 57 Jordanian healthy females.24
The result of these two studies supports the findings of the present study. In addition, decreased MCV but increased MCHC and haematocrit were observed due to one month fasting during Ramadan fasting groups in another study which is also in agreement with the findings of our study.25 Increased MCH, MCHC values, monocyte and total WBC count are perhaps due to dehydration caused by one month fasting during Ramadan.
Serum hs-CRP concentration in both healthy and asthmatic groups was significantly reduced after fasting during Ramadan. Variation of hs-CRP in the asthmatic group during Ramadan fasting period was non-significantly higher than control group. The effect of fasting on inflammatory mediators and lipid profile was examined in several studies. In 56 patients of different stable cardiac illnesses, HDL-C decreased and LDL-C significantly increased during compared to before fasting period in Ramadan but there were no significant changes in total cholesterol (TC), TG, serum leptin, or hs-CRP. These results showed that Ramadan fasting in stable cardiac patients has no effect on serum leptin, or hs-CRP, but results in decrease in HDL-C, increase in LDL-C.26 It was shown that one month fasting during Ramadan can lead to an increase in neuropeptide Y and decrease in leptin but no significant change was found in insulin level during the study.27 Biochemical analysis also showed a significant reduction in serum TG after the middle of Ramadan. A slight but not significant increase in HDL-C was observed in 57 Jordanian healthy females.24 The favourable effect of fasting during Ramadan on the immune system was also suggested.28 Results of other study showed that the Malondialdehyde (MDA), TG and Chol levels decreased significantly during Ramadan in fifty healthy 30–60 year-old men which indicates that fasting for a month may have an important anti-oxidant property leading to a preventive effect on diseases associated with increased oxidant activity.29 All these studies support the results of the present study indicating reduction effect of fasting on serum hs-CRP concentration in both healthy and asthmatic groups.
The results of the present study also showed non-significantly increases of most PFT values after Ramadan fasting month in both groups. In addition, no significant differences in PFT variations during fasting period in Ramadan were seen between asthmatic patients and healthy control group. There were also non-significant reductions in night cough, night and daily wheeze but a significant reduction in wheeze-o after one month fasting during Ramadan in asthmatic patients. The results of a study evaluating the status of fasting and drug usage in asthmatic and COPD patients showed that in a Muslim population, the patients with asthma and COPD do not feel their diseases to be an inhibitory factor for fasting during Ramadan. However, fasting seems to be an important determining factor in medication compliance by modifying the drug use behaviours in each group in a different way. Therefore, the patients should be informed about the effects of fasting on their disease and the drugs allowed during fasting.30 Therefore, the present study was undertaken to show the effects of fasting on asthma disease. The results showed that one month fasting during Ramadan not only has a detour effect on asthma but also leads to non-significantly increased of PFT values and reduction of respiratory symptoms and a significant decrease of chest wheeze on examination. In fact in one study on a hundred and twenty-one fasting asthmatic patients, most Muslim asthmatic patients did not consider asthma to be a drawback to fasting, and they continued fasting by rearranging their medication consumption times.2 In addition, no significant changes in clinical symptoms were reported in twenty-nine well-controlled asthmatic patients asthmatic patients at the end of Ramadan fasting. Peak expiratory flow improved after Ramadan31 which supports the findings of the present study. In addition, respiratory symptoms and PFT values of 30 asthmatic patients were compared at the end of Ramadan with the months before and after Ramadan The results of this study did not show significant difference in respiratory symptoms and PFT values at the end of three months (Shaban, Ramadan and Shawwal) which supports the finding of the present study.18
The limitation of the present study is the low sample size of the studied subjects. In addition, other inflammatory mediators including inflammatory cytokines and oxidising factors should be also evaluated during fasting period in Ramadan. Therefore in further studies, inflammatory and oxidising factors as well as respiratory symptoms and PFT values should examine in a larger sample size population of asthmatic patients.
ConclusionRamadan fasting period caused significant reduction in serum hs-CRP concentration and chest wheeze. In addition the variations in all other measured parameters during Ramadan were not different in asthmatic patients compared to healthy control subjects. Therefore, these results showed that Ramadan fasting period has no negative effect on asthma and may have some positive effect on asthma with regard to the effect on hs-CRP concentration and chest wheeze.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Authors’ contributionsStudy concept and design: Vahid Reza Askari, Mohammad Hossein Boskabady; Collection, analysis and interpretation of data: Vahid Reza Askari, Mohammad Hossein Boskabady; Drafting of the manuscript: Vahid Reza Askari, Mohammad Hossein Boskabady; and Critical revision of the manuscript for important intellectual content: Vahid Reza Askari, Azam Alavinejad, Mohammad Hossein Boskabady.
Conflict of interestThe authors declare that they have no conflict of interest.
This work was supported by a grant from Research Council of Mashhad University of Medical Sciences (Code: 930520).