Post-traumatic pseudo-aneurysms of the femoral artery are a rare complication. They normally have iatrogenic causes and immediately appear. Less often, they appear at a later stage and are related with traumatisms, orthopaedic surgery, bone lesions, infections, etc.
This report presents a case of a patient with allergy to heparin, and pseudo-aneurysm of the superficial femoral artery and 1st portion of the popliteal artery secondary to remote trauma in an extremity with serious deformities as a sequel. We performed conventional surgery using a posterior approach, and obtained a satisfactory outcome and evolution.
Os pseudoaneurismas pós-traumáticos da artéria femoral são uma complicação rara. Normalmente têm causa iatrogénica e aparecem de imediato. Menos frequentemente surgem numa fase tardia e costumam estar relacionados com traumatismos, cirurgia ortopédica, lesões ósseas, infeções, etc.
Este artigo apresenta o caso de um paciente alérgico àheparina com pseudoaneurisma da artéria femoral superficial e primeira parte da artéria poplítea, secundário ao traumatismo remoto de uma extremidade com sérias deformidades como sequela. Realizamos cirurgia convencional com abordagem posterior e obtivemos um resultado e evolução satisfatórios.
Post-traumatic pseudo-aneurysms of the femoral artery (FA) are a rare complication. The most common etiologies are iatrogenic punctures.1 Nevertheless, there are cases that arise gradually causing pseudo-aneurysms at a later time. In these cases we should perform a differential diagnosis for other possible causes.2–10 The most common clinical expression appears immediately in the context of percutaneous procedures. They appear as pulsatile masses with ecchymosis near the puncture. This is accompanied by symptoms arising from compressing adjacent structures. When they appear later in time, they are generally asymptomatic. They are diagnosed incidentally or due to complications appearing from local compression, distal embolization, thrombosis or rupture. The therapeutic approach is similar to that used for atherosclerotic aneurysms at this level. Even though open surgery remains the treatment of choice, endovascular repair is becoming increasingly used due to its low morbidity and mortality and good patency.
We report a case of a patient that presented a femoropopliteal pseudo-aneurysm in a severely deformed limb with multiple cutaneous grafts, chronic osteomyelitis and complete paralysis of the external sciatic nerve as a sequel of a remote trauma. In addition he presented allergy to heparin, detail that made change our therapeutic attitude.
Case reportWe present the case of a 53-year-old male with a previous history of allergy to neomycin, hypertension, and dyslipidemia. The patient had quit smoking 4 years earlier. The patient had suffered a traffic accident 25 years before causing a supracondylar fracture of the right femur, open fracture of the tibia and fibula with secondary acute ischaemia. The patient needed stabilization of the tibia and fibula with a Hoffmann external fixator and osteosynthesis of the fracture using Kirschner needles. Another health centre performed this. The arterial reconstruction was unknown and needed multiple skin grafts to cover it. As a sequel, the patient suffered complete paralysis of the external sciatic nerve and chronic osteomyelitis of the tibia.
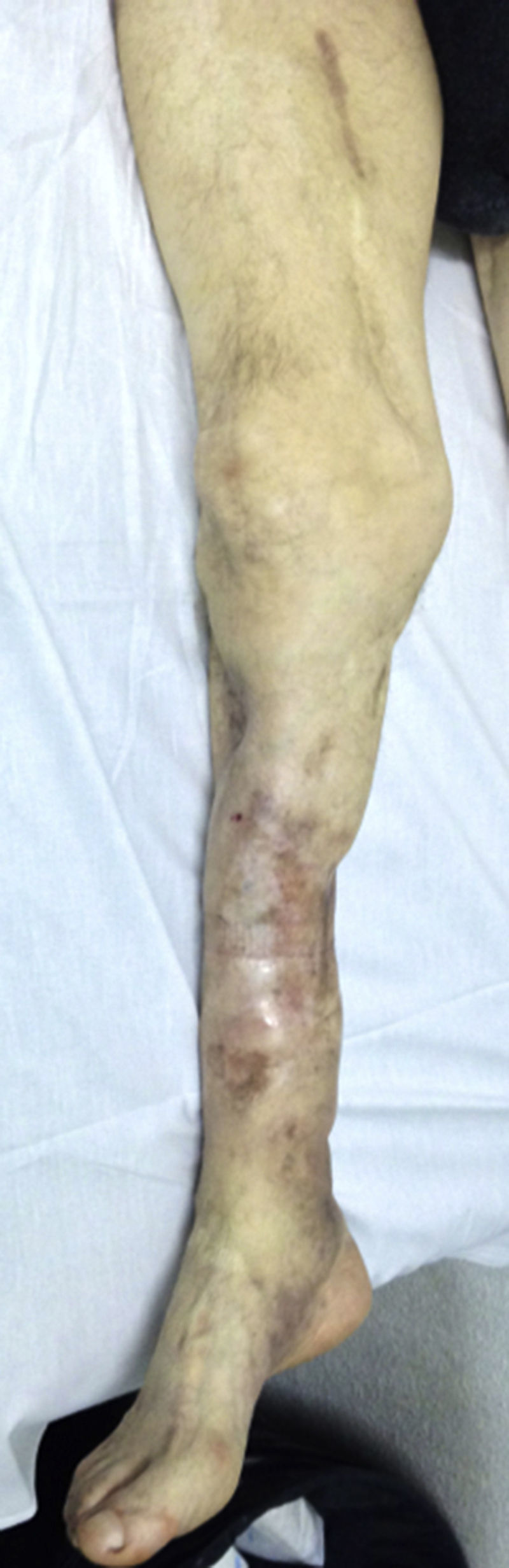
The patient was admitted to our service for a pulsatile lump, located on the inner face of the right thigh. This had appeared 18 months earlier and had increased in size. The clinical picture was accompanied by occasional discomfort in the limb and at the level of the lump; but without affecting the quality of ambulation. On physical examination we palpated a pulsatile lump on the inner face of the right thigh. This lump was about 7cm in length. The patient presented coldness in his foot, with slowed venous-capillary refilling, and on vascular exploration, he presented a femoral pulse, but absence of popliteal and distal pulses. The severe deformity of the limb after trauma with multiple cutaneous grafts is highlighted (Fig. 1).
The computed tomography angiography (CTA) revealed a roughly 76mm diameter pseudo-aneurysm of the distal superficial femoral artery (SFA), with mural thrombus and internal calcifications. The popliteal artery was difficult to see due to bone fixation material artefacts. The tibioperoneal trunk (TPT) was permeable with a peroneal artery as the only distal vessel. The anterior and posterior tibial arteries were occluded from the beginning (Fig. 2A, B).
CTA image. (A) Reconstruction showing a permeable pseudo-aneurysm of the distal SFA. Bone fixation material artefacts at the level of popliteal artery. TPT permeable with a peroneal artery as the only distal vessel. Anterior and posterior arteries totally occluded from the beginning. (B) Axial view showing the 76mm diameter pseudo-aneurysm with mural thrombus and calcification. (C) Diagnostic angiography showing the pseudo-aneurysm of the SFA – 1st portion of the popliteal artery, 2nd portion occluded with repermeabilisation of the 3rd portion. (D) The peroneal artery was the only outflow vessel.
Among the various therapeutic options, we initially chose placing a Viabahn® endoprosthesis since it is the less aggressive choice in a greatly deformed extremity (fractures, previous surgery, grafts, etc.). However, 4 days after admission, the patient suffered an allergic reaction to low molecular weight heparin (LMWH). We performed allergy tests (prick tests and intra-dermoreaction), which proved negative in the immediate reading and positive at 48h for sodium heparin, enoxaparin, Fraxiparine, and bemiparin and negative for Fondaparinux. We diagnosed the patient for delayed hypersensitivity reaction to sodium heparin and LMWH except for Fondaparinux.
Due to this diagnosed allergy, we discarded Viabahn® endoprosthesis placement, since this contains a heparin coating, and opted for surgical treatment. We decided to carry out a diagnostic arteriography (Fig. 2C, D) in which we observed pseudo-aneurysm of the SFA and 1st portion of the popliteal artery, occlusion of the 2nd portion, and repermeabilisation of the 3rd portion. The TPT was permeable with outflow from the peroneal artery as the only exit vessel.
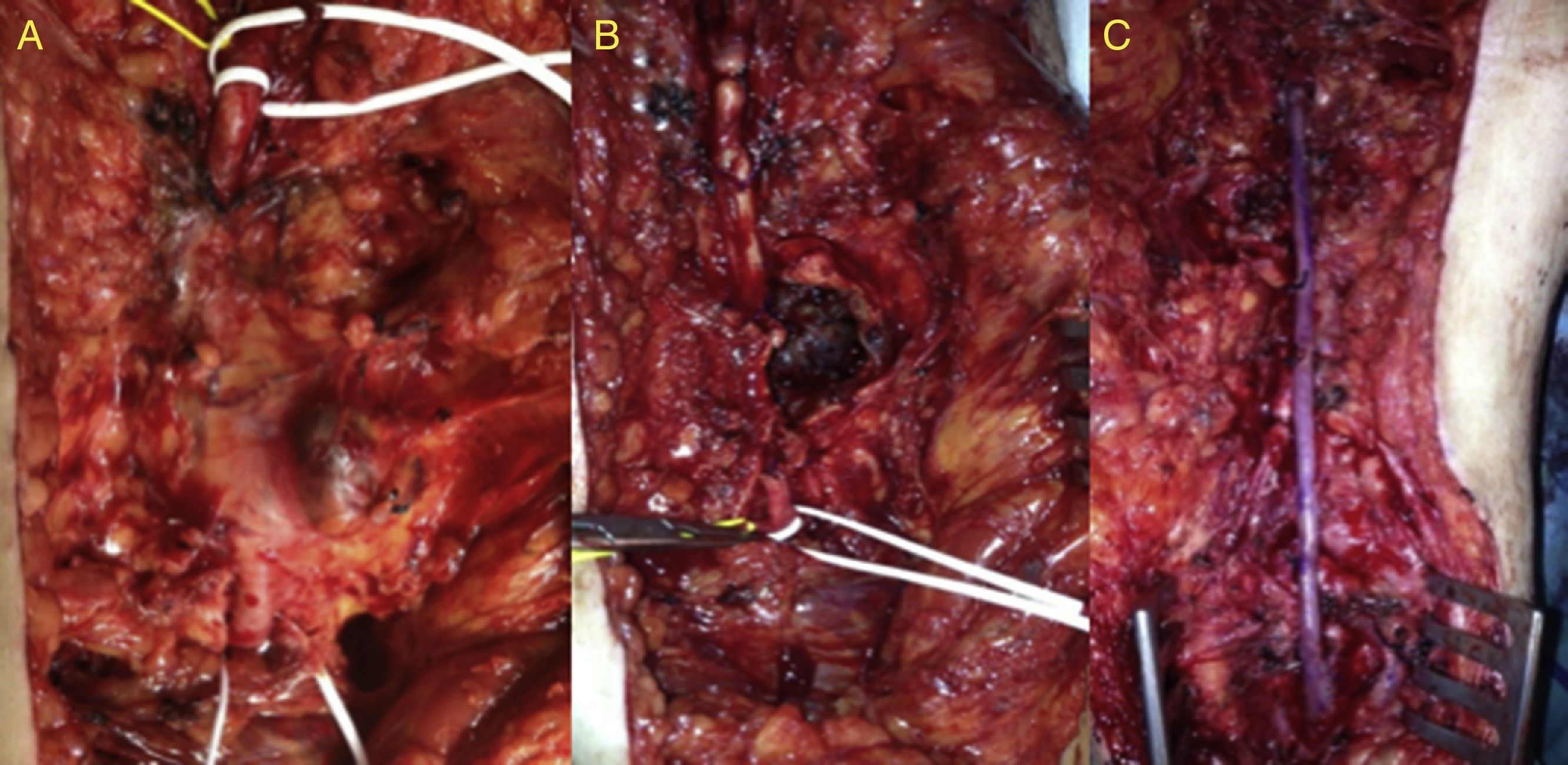
Considering the serious limb deformity and previous surgeries, we decided to use a posterior approach to the popliteal artery. We performed the pseudo-aneurysm resection and a bypass from the SFA to the 3rd portion of the popliteal artery with the inverted contralateral great saphenous vein (GSV) (Fig. 3A–C). During the procedure, we did not use systemic or local heparinisation, and only used an intraoperative plasma volume expander infusion (Voluven® 6% hydroxyethyl starch 130/0.4 in 0.9% sodium chloride).
Intraoperative images of the posterior approach with proximal control of distal SFA. (A) Fibrotic tissue surrounding the artery. (B) Pseudo-aneurysm dissection and arteriotomy revealing thrombus inside. (C) Pseudo-aneurysm resection and bypass from SFA to 3rd portion of the popliteal artery with inverted contralateral GSV.
The patient showed good postoperative evolution. Immediate complications included revascularization oedema that progressively remitted. The patient was discharged from hospital after 10 days, with a permeable bypass and good distal perfusion with conserved motility and sensitivity. After 30 months of follow-up, the patient remains asymptomatic and with a permeable bypass (Fig. 4).
DiscussionFemoral pseudo-aneurysms are a rare injury. They mostly occur from iatrogenic causes after performing percutaneous techniques of arterial catheterization. This is related to the increased use of these techniques.1 However, in late-appearing pseudo-aneurysms, we must perform a differential diagnosis for other possible causes such as previous injuries, orthopaedic surgery or others,2,4 bone lesions,3,6 infections (Salmonella, Escherichia coli, Staphylococcus aureus),5,7 diseases of the connective tissue (Ehlers–Danlos syndrome, Marfan Syndrome),8,9 inflammatory arteritis,10 etc.
Given the low incidence, both treatment and diagnostic strategy are based on clinical series which include atherosclerotic aneurysms at the femoropopliteal level.
Different imaging techniques are useful for diagnosis, such as Doppler ultrasound, computed tomography angiography (CTA), magnetic resonance angiography (MRA) and angiography.
Conventional surgery is the technique of choice, but endovascular techniques are becoming increasingly used as they are less aggressive and have good medium term results.11,12
Endovascular treatment has advantages such as a low mortality (0.6–3.5%), a success rate of 97% and a short hospital stay. Piazza et al. recently published long-term outcomes of endovascular exclusion of popliteal aneurysms.13 Retrospective revision finds 46 endovascular repairs of which 93% of the cases were elective and the rest due to rupture or acute thrombosis. The primary patencies at 1, 3 and 5 years were 82%, 79% and 76% respectively, while the secondary patencies were 90%, 85% and 82% respectively.
It does not need general or local anaesthesia; thus reducing cardiac risk, and may be performed percutaneously or with a minimal incision.14 It must, however, meet selection criteria, such as having proximal and distal anchoring areas of at least of 2cm, patency of at least one exiting blood vessel, avoid excessive tortuosity and avoid excessively long lengths of aneurysms. A >20cm segment coverage turns out to be a negative predictor of permeability (p<0.032) and could explain the greater failure of the stent.13 The longer the device, the greater the rigidity it exerts on the area distal to the landing zone. This is a probable cause of kinking or friction on the arterial wall over time.12,13 It is not recommended in patients who frequently flex their knees >90° due to working conditions (risk of fracture or thrombosis) or in patients with dual antiplatelet therapy contraindications.15 Also it is not recommended in young patients, good operative risk, one vessel run-off or popliteal occlusion. Surgical decompression may be necessary after time despite the aneurysm has been satisfactorily excluded. It is, therefore, a factor to consider when assessing open surgery versus endovascular treatment of long or ruptured aneurysms.13
In our case, because of multiple previous surgeries of the extremity, we decided to perform endovascular treatment by placing an endoprosthesis (Viabahn®) as this was the less aggressive choice. However, as this device is covered in heparin, we discarded this option after discovering heparin allergy. The patient presented a local skin reaction and delayed-type hypersensitivity which is the most frequently kind of reaction reported. Therefore Fondaparinux, a factor Xa inhibitor, was used instead of heparin. It is a safe alternative for heparin allergic patients due to its low allergic potential and lack of cross-reaction to heparins.
Surgical treatment is the classic technique of choice. It is indicated in patients with acceptable risk, with complex anatomy, symptoms or in the presence of more advanced degrees of acute ischemia.16 It presents an excellent primary patency at 1 year in 95.9% of cases,12,16–20 with a significantly lower rate of adverse events (greater amputation or reoperation) after 1 year.17 This suggests that it should be proposed as the first choice in all asymptomatic patients that are not otherwise contraindicated for surgery. The most frequently used surgical approach is the medial since it allows us to exclude larger aneurysms that need a more distal bypass allowing easy access to the GSV in its entire course. The main drawback is in aneurysms that affect the popliteal artery, as it does not allow their decompression after ligation. Numerous studies21 show that despite the proximal and distal ligature, in 30% of cases the aneurysm does not undergo thrombosis and continues to grow owing to the persistence of collateral patency. This causes pain, compression symptoms and rupture requiring reoperation. Some authors recommend the ligation of back-bleeding side branches, except in small aneurysms.15 This can usually be done from the supracondylar and infracondylar spaces.
The posterior approach is preferred for aneurysms confined to the popliteal space and represents the best choice to decompress aneurysms that have continued to grow after being treated as a result of the flow through genicular arteries. As a drawback it has more risk of nerve injury and is not recommended in cases of aneurysms that extend very proximally or distally.15
Here, in the case of a traumatic limb with numerous previous surgeries and skin grafts, the medial approach was inaccessible given the prior trauma. Thus, redissection would involve risk of nerve or muscle injury. Finally, we opted for the posterior approach since it represented a virgin approach, which, with a wide dissection, allowed us to deal with the aneurysm located in the distal SFA, and perform the distal anastomoses in the TPT.
Another challenging issue of this case was the necessity of Voluven® instead of heparin during vascular clamping reconstruction due to the heparin allergy diagnosed while his admission. Hydroxyethyl starches (HES) are synthetic colloids commonly used for fluid resuscitation to replace intravascular volume. First-generation HES have been reported to consistently decrease plasma concentrations of coagulation factor VIII and von Willebrand factor.22–23 HES also impair platelet function, likely via an extracellular coating mechanism.24 Several clinical trials have examined the effect of preoperative administration of third-generation HES on coagulation parameters after cardiac surgery and compared with other colloids.25 Schramko et al.26 assessed the effects of a short-term postoperative infusion of HES or human albumin on blood coagulation in primary elective cardiac surgical patients. Blood loss and transfusion requirements were similar in all groups. However, when compared with the albumin group, transient prolongation of clot formation times and decrease in clot firmness were observed in HES group.
ConclusionsPost-traumatic pseudo-aneurysms are a rare complication following trauma of extremities. Sometimes they are associated with serious deformities, which limit the surgical approach. Currently, the development of endovascular techniques allows us to treat them with a minimally aggressive approach, and with rates of patency approaching those of open surgery in selected patients (with favourable anatomy, high-surgical risk). However, it is not always applicable. Open surgery continues to be the treatment of choice, and the knowledge of both types of approach allows the treatment of complex cases.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.