The causes of abdominal pain in patients with liver cirrhosis and ascites are well-known but occasionally, atypical causes arise. We report the case of a patient with a ruptured, confined abdominal aortic aneurysm.
Abdominal pain in cirrhotic patients is a challenge. Clinical presentation can be non-specific and the need for early surgical exploration may be difficult to assess. Coagulopathy, thrombocytopenia, varices, and ascites need to be taken into account, since they can increase the surgical risk. Possible differential diagnoses include: Complicated umbilical, inguinal or postoperative incisional hernias, acute cholecystitis, spontaneous bacterial peritonitis, peptic ulcer bleeding, perforated ulcer, pancreatitis, penetrating abdominal wounds, acute appendicitis, spleen rupture, choledocholithiasis with cholangitis, bowel obstructions among others.1,2
The diagnosis of aortic aneurysm is established when a permanent and localized dilatation of an artery, greater than 50% of its normal diameter, is detected.3 It is classified as an abdominal aortic aneurysm (AAA), when it is restricted to the infra-renal part of the aorta (90% originates below the renal arteries).3 Its prevalence has been estimated between 2 to 5.9% worldwide,4 but in Mexico, limited information is available. Many AAA may remain asymptomatic for many years but after rupture, only one fifth of patients survive.4 In cirrhotic patients, little is known about the management of AAA.5
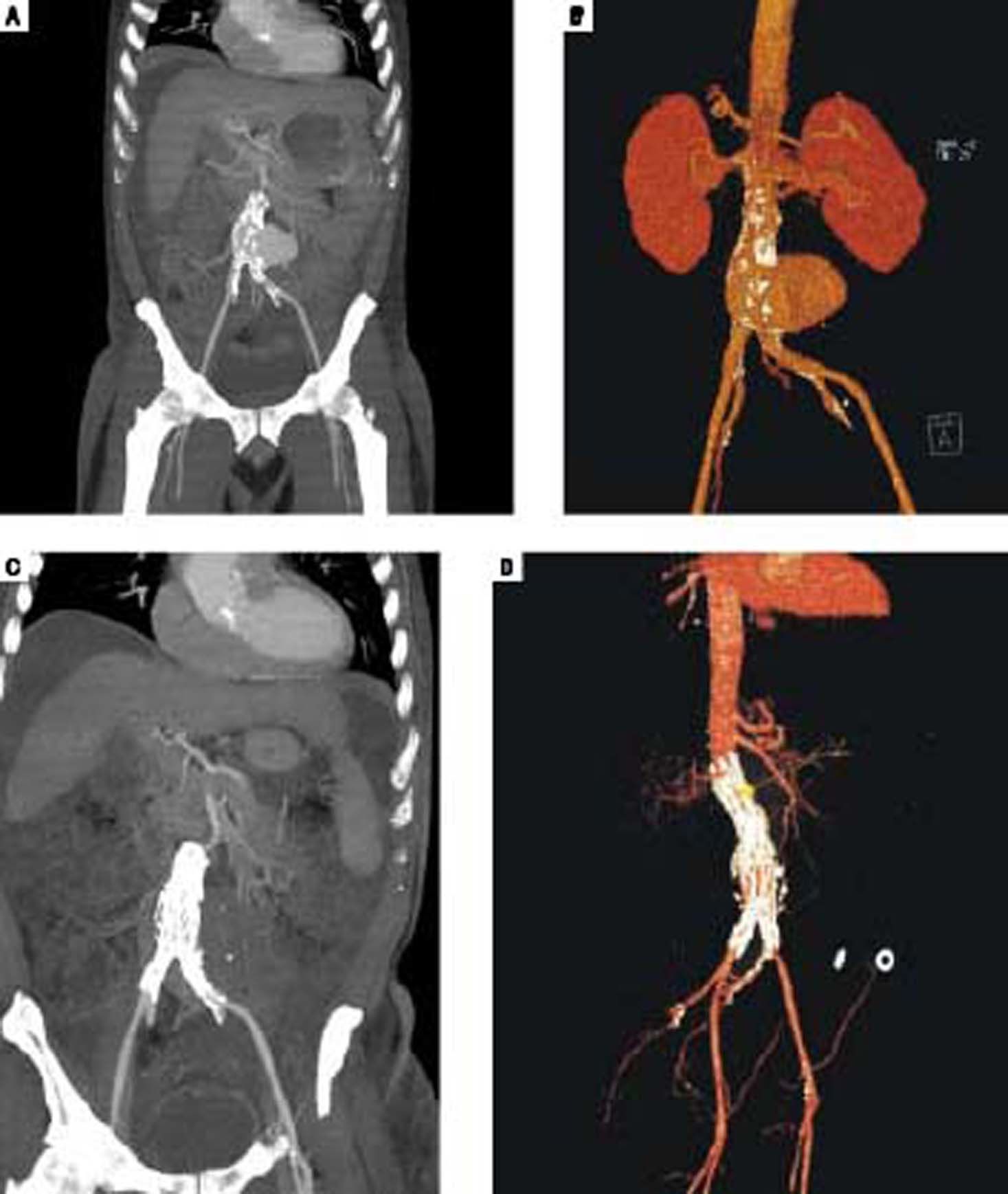
Case ReportA 47-year-old male with the established diagnosis of alcohol-related liver cirrhosis, presented to the emergency department for abdominal pain. He was classified as Child Pugh (CP) C stage (10 points) and had a model for end stage liver disease (MELD) -sodium (Na) of 21 points. The pain was referred to the left iliac fossa, with an intensity of 10/10. It was associated to low back pain with radicular stigmata (primarily S1). As part of the approach, an MRI revealed a fracture of the L5 vertebral body with no signs of radicular involvement and an image suggestive of an abdominal aneurysm. An angio-to-mography was performed, and a ruptured confined aneurysm of the abdominal aorta with a hematoma were observed (Figures 1A, 1B). The Vascular Surgery Department evaluated the patient, and due to the associated risk, a medicated aortic stent was preferred. It was implanted without complications (Figures 1C, 1D). During follow-up, no abdominal pain was reported. The patient was completely evaluated for liver transplant but during follow-up, alcohol consumption was documented. The patient died 6 months later due to variceal bleeding.
DiscussionCurrently, with improved care of cirrhotic patients, more cases with AAA and cirrhosis are to be expected. An association between alcohol consumption and arterial hypertension (AHT) with AAA has been documented.6 The severity and poor control of AHT is known to promote aortic dissection,6 as is the excessive alcohol consumption inducing holiday heart syndrome. Other theories suggest that ethanol may have a direct effect on the aortic wall,6 but little is known on this possible association.
In cirrhotic patients, abdominal surgery needs to be carefully considered. Multiple factors, as described above, coupled with severe liver dysfunction and pronounced metabolic acidosis can compromise the outcome.5 MELD
and CP score may aid in the decision and some reports have suggested that patients in a compensated state and a MELD score ≤ 18 or less, may undergo elective AAA open repair.3 Others advocate for endovascular aneurysm repair in patients with CPB or C,7 and the possibility of reconstruction at the time of liver transplantation is also an option.8 In this case, a ruptured confined aneurysm was found and was considered a vascular emergency due to a high CP and MELD score, so an endovascular approach was considered and was feasible.
FundingThe present study received no financial support.
Conflict of InterestThe authors report no conflicts of interest.