Back in March 1997, an international workshop was held in Dahlem, Germany, focusing on principles for eradication of infectious diseases.1 During the workshop the hierarchy of possible public health interventions for dealing with infectious diseases were described and defined (Table 1). All these interventions need three important prerequisites:
- a)
Effective intervention to interrupt transmission of the infectious agent;
- b)
Practical diagnostic tools with sufficient sensitivity and specificity to detect levels of infection that can lead to transmission; and
- c)
Humans being essential for the life cycle of the infectious agent.
Definition of Public Health Interventions for Infectious Diseases.
| Control | Reduction of disease incidence, prevalence, morbidity or mortality to a locally acceptable level following deliberate efforts with ongoing intervention measures to maintain this reduction. |
| Elimination of disease | Reduction to zero the incidence of a specific disease in a defined geographical area as a result of deliberate efforts with ongoing intervention measures. |
| Elimination of infections | Reduction to zero the incidence of infection caused by a specific agent in a defined geographical area as a result of deliberate efforts with continued measures to prevent re-establishment of transmission. |
| Eradication | Permanent reduction to zero of the worldwide incidence of infection caused by the specific agent as a result of deliberate efforts. |
| Extinction | The specific infectious agent no longer exists in nature or in the laboratory. |
At that same meeting, it was recognized that health resources are generally limited. Hence decisions had to be made early whether one would use elimination or eradication programs. The costs and benefits of global eradication programmes had to be measured with their direct effects on morbidity and mortality and eventually on the health care system. The participants of the Dahlem Workshop also recognized that success depended strongly on the level of societal and political commitment, with a key role for the World Health Assembly.
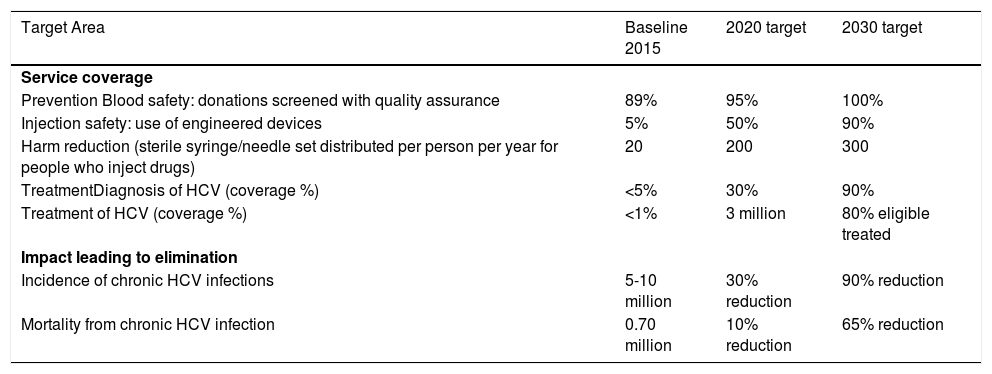
In 2016, twenty-seven years after the hepatitis C virus (HCV) was discovered, 194 member countries of the World Health Organization (WHO) adopted the first global health sector strategy on viral hepatitis to halt transmission of viral hepatitis and provide everyone living with viral hepatitis access to safe, affordable, and effective care and treatment.2 WHO published its advocacy brief for combating viral hepatitis to reach elimination by the year 2030. Table 2 provides summary of interventions and targets specific for HCV.3 Subsequently, all four leading professional organizations in liver disease endorsed elimination of viral hepatitis urging governments, healthcare organizations and non-governmental organizations to implement action plans to move this process forward.4
WHO Targets for Elimination of HCV from 2015-2030 (adapted from reference 3).
| Target Area | Baseline 2015 | 2020 target | 2030 target |
|---|---|---|---|
| Service coverage | |||
| Prevention Blood safety: donations screened with quality assurance | 89% | 95% | 100% |
| Injection safety: use of engineered devices | 5% | 50% | 90% |
| Harm reduction (sterile syringe/needle set distributed per person per year for people who inject drugs) | 20 | 200 | 300 |
| TreatmentDiagnosis of HCV (coverage %) | <5% | 30% | 90% |
| Treatment of HCV (coverage %) | <1% | 3 million | 80% eligible treated |
| Impact leading to elimination | |||
| Incidence of chronic HCV infections | 5-10 million | 30% reduction | 90% reduction |
| Mortality from chronic HCV infection | 0.70 million | 10% reduction | 65% reduction |
In this issue of the Annals of Hepatology, Francheville, et al. describe their experience from the first 12 months of multi-phase hepatitis C elimination strategy within the geographic confines of Prince Edward Island (PEI), the smallest of Canadian provinces. They demonstrate encouraging results for improved access to treatment, enhanced engagement by health care providers, and increased rates of cure for patients living with chronic hepatitis C genotype-1.
Prince Edward Island population is approximately 146,000. It is estimated there are 629 individuals infected with HCV on the Island. The current study reports the initial 242 referrals (comprising 38% of all HCV cases living in PEI), 123 patients (50% of referred) seen for intake assessments, and 93 (76% of assessed) started on direct-acting antiviral (DAA) therapy based on medical need. All of this occurred in the first year of the Program. Furthermore, sustained viral response was documented in more than 95% of subjects who completed treatment with DAAs.
The availability of DAAs for HCV provides opportunities to eliminate HCV but the latter also requires scaling-up of treatment with considerable cost. Bringing local health care providers, government, industry, and HCV community groups together created a province-wide model of care. This collaboration might have been the most important aspect of the Program. In spite high prices, PEI announced the decision to provide treatment for all persons infected with HCV. As a result of a collaborative procurement strategy between Government and industry, treatment regime with DAAs was provided to all eligible patients – a feat previously thought impossible. Any public health expert in infectious disease eradication or elimination will emphasize the need for societal and political commitment. The political commitment for elimination strategy goes hand-in-hand with appropriate advocacy. This article provides proof-of-principle for starting elimination program for HCV within a specific geographic area. The real success of the Program will be clearer with long-term monitoring.
As different jurisdictions start their individual HCV elimination strategies, new post-elimination challenges will arise. If PEI became HCV-negative jurisdiction, how would they enforce zero incidence for HCV? Will they require point-of-care testing at entry points to the Island? Will they be able to identify each asymptomatic carrier of HCV who may potentially transmit the virus and re-introduce HCV to the Island? Would there be viable vaccination programs for people who inject drugs? Or will the post-elimination strategy depend on post-exposure prophylaxis protocol for those potentially exposed to HCV? Even if HCV is eliminated from any jurisdiction, there will be global demand for further research into these questions and other medical or public health challenges.
Elimination programs for HCV are laudable, but carry awesome responsibility. Unlike eradication programs, elimination programs can handle some failure. Careful and deliberate evaluation of every program is a prerequisite to navigate the best strategies for elimination of HCV - the ultimate goal of public health. This article provides a blue-print.