There is increasing evidence that fatty liver may be the most frequent liver disorder in Western countries. However, the epidemiology of fatty liver is still not fully understood and there is a clear need of better assessing and defining the potential role of the risk factors identified by clinical series in the general population. This article reviews the available data on the epidemiology of fatty liver and addresses some important questions that should be answered in much needed future research.
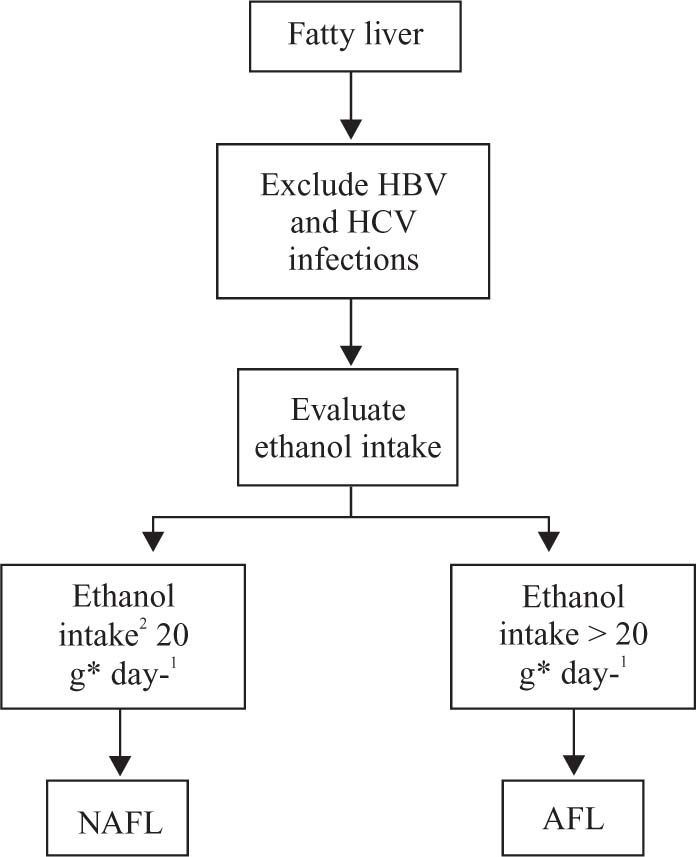
Fatty liver is an accumulation of fat inside the hepatocytes exceeding 5% of the weight of the liver; the excess fat is stored mainly as triglycerides.1 Fatty liver encompasses a wide spectrum of liver abnormalities, ranging from steatosis to steatohepatitis and fibrosis.1 While steatosis is usually associated with a benign prognosis, steatohepatitis and fibrosis may progress to cirrhosis.12 After exclusion of HBV and HCV infections, which may be associated with fatty liver (in particular HCV infection), the whole spectrum of abnormalities of fatty liver is currently classified as alcoholic (AFL) or non-alcoholic (NAFL) fatty liver on the basis of ethanol intake.2-4 AFL is diagnosed when ethanol intake is greater than 20 g*day-1 and NAFL when ethanol intake is equal to or lower than this value (Figure 1). This distinction, based on the assumption that quantities of ethanol under 20 g*day-1 are not toxic for the liver,2 is of paramount importance, because there are no clinical signs or histological lesions truly pathognomonic for AFL or NAFL.1,2 However, the distinction between AFL and NAFL is arbitrary from many viewpoints. In fact, besides the effect of the chosen cut-point of ethanol intake on the prevalence of AFL and NAFL,2 this distinction does not consider the possible coexistence of metabolic and viral causes of fatty liver1 and the interaction of alcoholic and metabolic causes in determining the risk of fatty liver.5 Despite these limitations, a consensus on an operational definition of AFL and NAFL has to be reached by researchers and clinicians worldwide if we want to be able to disentangle the natural history of fatty liver.2 As it happens for all operational definitions, also the definition of AFL and NAFL may undergo revision as new data accumulates. The acronyms AFLD and NAFLD – where “D” stands for disease – have recently been proposed as a replacement for the AFL and NAFL ones.3,4 However, it is controversial whether fatty liver should be considered a “disease” owing to its generally benign prognosis.5 This is why we prefer to use the acronyms AFL and NAFL in the first steps of clinical diagnosis, when fatty liver is most commonly diagnosed by means of ultrasonography. This technique is reported to have a sensitivity of 83% and a specificity of 100% for the diagnosis of fatty liver, defined as the presence of fat in more than 30% of each hepatic lobule, when a combination of four parameters is used: 1) diffuse hyperechoic echotexture (“bright liver”), 2) increased liver echotexture compared with the kidneys, 3) vascular blurring, and, 4) deep attenuation.3 Thus, about two out of ten patients with positive ultrasonography will not have fatty liver at biopsy and none of the patients with negative ultrasonography will have fatty liver at biopsy. However, only liver biopsy can diagnose fatty liver with certainty and, most important, it is needed for the diagnosis of alcoholic (ASH) and non-alcoholic (NASH) steatohepatitis.1 These are the stages of AFL and NAFL characterized by inflammation and fibrosis and may progress to cirrhosis.1 Due to our limited knowledge of the natural history of fatty liver, it is controversial whether all subjects with suspected fatty liver should undergo liver biopsy.6,7 Even if predictors of inflammation and fibrosis have been identified, especially for patients with NAFL, their diagnostic accuracy is not high enough to base the decision of performing a liver biopsy entirely on them.8
How frequent is fatty liver?For obvious ethical reasons, liver biopsy cannot be used in epidemiological studies of liver disease. This implies that the prevalence and incidence of fatty liver, and, most importantly, that of ASH and NASH, will remain undisclosed in the general population until a noninvasive method will be available to diagnose liver inflammation and fibrosis. While ultrasonography offers a reasonably accurate alternative to liver biopsy in population studies of fatty liver, this technique cannot be used to define the natural history of fatty liver due to its inability to assess inflammation and fibrosis. This explains why the available data on the prevalence of fatty liver are based on ultrasonography or on autopsy studies performed in selected populations.9 The prevalence of NAFL in Western Countries is estimated to be around 20-30%.4 In the population who took part to the Dionysos Study in 1991-1992,10 one third of cases of fatty liver can be classified as NAFL according to the current definition.1,2 Moreover, around 70% of individuals with increased alanine transaminase levels who underwent to hepatic ultrasonography had fatty liver (Figure 2). Much less data are available on AFL prevalence, also because the cut-point of 20 g*day-1 for ethanol intake was adopted only recently, and because it is crucial to adopt correct and reliable methods to calculate daily alcohol intake. According to the data collected in the years 1991-92, during the first part of the Dionysos Study, when alcohol intake has been measured with a validated semiquantitative colour-illustrated food questionnaire,10 the prevalence of AFL in the general population was 43% (Figure 2).
For the reasons stated above, the prevalence of ASH and NASH in the general population is unknown. On the basis of estimates obtained from selected series, NASH is expected to affect 2-3% of individuals in the general population.4 Some years ago, by pooling the results of various studies and using a cut-point of 30 g*day-1 for ethanol consumption, we estimated the prevalence of ASH to be comprised between 4 and 8% in Western countries.9 No data are available on the incidence of fatty liver. Preliminary results from a 10-year follow-up of a cohort of individuals who took part to the Dionysos study in 1991-199210 show that 20% of them developed liver steatosis, corresponding to an incidence of 2% per year.
Why is fatty liver frequent?Besides the quantity of ethanol ingested, genetic factors and other factors such as the pattern of drinking may explain why not all individuals who consume large quantities of ethanol develop steatohepatitis and fibrosis.11,12 It is important to bear in mind that the steatogenic effect of alcohol is substantially increased by the presence of obesity. We evaluated the degree of interaction between obesity and ethanol intake in determining liver steatosis in the general population.5 A representative sample of Dionysos individuals with fatty liver and without viral infection and any drug consumption in the last 6 months, were stratified in four groups according to body weight and ethanol consumption: 1) normal-weight teetotalers, 2) obese teetotalers, 3) normal-weight and heavy drinkers (i.e. drinking more than 60 g*day-1 of ethanol), and 4) obese and heavy drinkers. As compared to normal-weight teetotalers, the relative risk of steatosis was 2.8 in normal-weight heavy drinkers, 4.6 in obese subjects and 5.8 in obese heavy drinkers. Fatty liver was present in 95% of obese heavy drinkers. Thus, there is an interaction between obesity and alcohol intake in the general population and obesity is stronger than alcohol consumption as risk factor for liver steatosis. Equally interesting, however, is the observation that liver steatosis was present in 16% of lean subjects without any ethanol consumption, suggesting that other factors play a role in determining the accumulation of lipids in the liver. In addition, this figure points to the rather high prevalence of steatosis even in the absence of known risk factors for the condition. Even if population studies are lacking and are identified as a research priority,4NAFL is considered the most frequent form of liver disease in Western countries.3,4 However, there is substantial variability from one country to another. The high prevalence of NAFL in Western countries is probably due to the contemporary epidemics of obesity and associated metabolic complications. Obesity, type 2 diabetes and hyperlipidemia are recognized risk factors for NAFL. As reviewed be Angu-lo,13 the prevalence of obesity in patients with NAFL varies between 30 and 100%, that of type 2 diabetes between 10 and 75%, and that of hyperlipidemia between 20 and 92%. In the Dionysos study, the prevalence of NAFL was 4.6 times higher in obese than in non-obese individuals.5 Insulin resistance is common in obesity and is the hallmark of type 2 diabetes.14,15 It is also frequently detected in patients with NAFL, also in those without obesity and diabetes.15 Thus, insulin resistance has been proposed as the minimum common denominator of most cases of NAFL.3 Insulin resistance, impaired glucose tolerance, obesity and hyperlipidemia are all elements of the socalled metabolic syndrome so that NAFL has been proposed as another element of this syndrome. In a recent study, 18% of normal-weight and 67% of obese subjects had the metabolic syndrome.15 Eighty-eight percent of the patients with NASH had the metabolic syndrome as compared to 53% of those with simple steatosis. Even more interestingly, the metabolic syndrome was a predictor of liver fibrosis. These and other data suggest that insulin resistance may be a risk factor for the progression of simple steatosis to NASH, even if a cause-effect relationship can be disclosed only by prospective studies. Because the available data on insulin resistance, the metabolic syndrome and NAFL were obtained from selected clinical series, it is important to test the association of insulin resistance with NAFL in the general population. Obesity, type 2 diabetes, hyperlipidemia and insulin resistance can be considered nutritional risk factors in view of their substantial dependence from nutritional status. However, contrarily to cardiovascular and metabolic diseases, which are manifestations of the metabolic syndrome, there is no epidemiological evidence that dietary habits may be associated with fatty liver. A high intake of saturated fatty acids and cholesterol and a low intake of polyunsaturated fatty acids, fiber, ascorbic acid and tocopherol, have been described to be associated with NASH in a selected series of patients16 but these results need to be confirmed and possibly extended in larger series.
ConclusionAt present, there is enough evidence to consider fatty liver, and especially NAFL, the most frequent liver disease in Western countries. However, our knowledge of the epidemiology of fatty liver is still rudimentary and there is a clear need of testing the significance of the risk factors identified by clinical series in the general population. This will allow understanding better what is associated with fat deposition in the liver, from one end, and whether this condition is really benign as stated from the other. The answer to these questions is important and will certainly keep investigators busy in the years to come.
AcknowledgementsThe authors are grateful to Claudio Tiribelli for helpful discussions and critical reading of the manuscript. Data presented in this article were collected with the support of grants from Regione Friuli Venezia Giulia and Emilia Romagna and from Fondo Studio Malattie Fegato-ONLUS.