Dear Editor,
Alcoholic liver disease (ALD) encompasses a broad spectrum of liver pathology, from steatosis to alcoholic st-eatohepatitis, cirrhosis, and hepatocellular carcinoma. Alcohol has a synergistic effect with other chronic liver diseases leading to accelerated progression. Racial and ethnic differences have been documented for some chronic diseases, including hypertension, heart failure, and ALD. Women are more susceptible to ALD than men when exposed to similar amounts of alcohol, and Hispanics are more prone to develop ALD than blacks and Caucasians.1,2 Accordingly, the aim of this study was to characterize patients with ALD admitted to a community hospital that serves a predominantly Hispanic population in East Harlem in New York City to learn the spectrum of liver disease in hospitalized patients from the community.
We conducted a retrospective review of charts of patients aged 18 to 85 years admitted to the Medicine service at Metropolitan Hospital Center with a diagnosis of ALD identified by the use of ICD-9 codes from 2002, when the hospital instituted its electronic medical records, to 2011. Demographic data, co-morbidities, intensive care unit admission, and need for mechanical ventilation were recorded. The 3 months survival after discharge was also documented. Pregnancy, incomplete documentation, and anticoagulation therapy were the exclusion criteria. Statistical analysis was done by the use of χ2 and Fisher exact test for categorical data by the use of SAS program. A p value of < 0.05 was considered statistically significant. The study was approved by the New York Medical College Institutional Review Board.
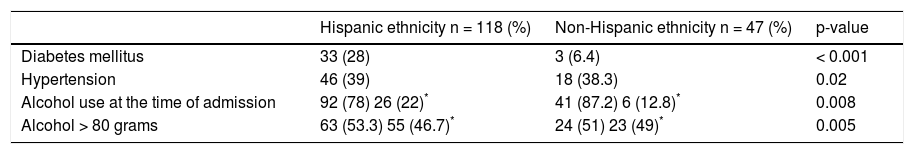
ALD was identified in 165 patients. The group was comprised of 138 males and 27 females, 118 of whom (71.5%) were of Hispanic and 47 (28.5%) were of non-Hispanic ethnicity, which was comprised of 34 blacks, 12 Caucasians and 1 Asian. The average age was 53 years. The comorbidities and alcohol use in the study group is provided in the table. The proportion of patients that reported drinking at the time of admission and the estimated daily grams of alcohol consumed by the subjects was higher in the non-Hispanic group than in the Hispanic group, both exhibiting a statistically significant difference; however, data on these two factors were not available in all patients (Table 1).
Comorbidities and alcohol use in the study group.
There was a significant difference between the number of non-Hispanic (n = 104) and Hispanic (n = 7) patients who did not require intensive care unit admission (p = 0.015). There was also a significant difference between non-Hispanic (n = 16) and Hispanic (n = 7) patients who did not require mechanical ventilation. In addition, a significant association was found for patients who did not require mechanical ventilation stratified by non-Hispanic (n = 132) population and Hispanic women (n = 10) (p = 0.0006) although, the need for mechanical ventilation was not different between Non-Hispanic (n = 9) and Hispanic women (n = 10) (p = 0.086). Eighteen of the 165 patients had died at 90 days post admission, 12 non-Hispanic and 6 Hispanic. In a stratified analysis, there was a significant association between mortality and the Hispanic women group and non-Hispanic patients (p = 0.0007); however, the 90 day mortality for Hispanic (n = 6) vs. non-Hispanic women (n = 1) was not significantly different (p = 0.20).
The study revealed that the majority of patients admitted to the hospital with ALD was of the Hispanic ethnicity. This finding may be a reflection of the population that uses the hospital for care; however, it raises the question of a potential increase in the prevalence of ALD in the Hispanic group.
An important finding of this study was that ALD was associated with heightened morbidity and mortality, as suggested by the increased number of intensive care unit admissions, and the need for mechanical ventilation in Hispanic patients. The reason for the increase in the severity of ALD in the Hispanic group is not apparent from the study. In this regard, the proportion of subjects that was drinking on admission and the grams of daily alcohol drunk by them was higher in the non-Hispanic group than in the Hispanic group; however, this information was not available for all subjects, thus, the data cannot be interpreted accurately. Ethnic disparities have been reported in some chronic health conditions3,4 although they are not well documented in ALD; in this context, it is possible that the increase in the severity of ALD in the Hispanic subjects was due to the ethnicity itself.
The inflammatory response to alcohol is reported to be increased in chronic alcohol users which may lead to multi-organ failure. In the lungs, alcohol impairs the host's innate pulmonary defense mechanism directly, by altering the normal alveolar barrier function, and indirectly, by affecting the circulating blood cells such as neutrophils, monocytes, and macrophages thus making ALD patients prone to infections, such as Klebsiella pneumoniae and increased risk for adult respiratory distress syndrome (ARDS) and mechanical ventilation support.5 This study showed that the non-Hispanic population did not require mechanical ventilation and intensive care unit admission as frequently as the Hispanic group. A similar observation was reported in a study on blunt trauma patients that documented that Hispanic as compared to black patients were associated with a higher mortality and case fatality rates for ARDS.6
This study also revealed that Hispanic women were at increased risk for mechanical ventilation as compared to the entire non-Hispanic population, however, there was no difference when compared to non-Hispanic women; the lack of significant difference of this finding may be due to the relatively small sample size of the study. Nevertheless, in general, women are more susceptible to alcohol hepatotoxicity which is reported to be secondary to a decreased in the enzyme alcohol dehydrogenase activity, heightened gut permeability leading to increased endotox-in levels in the blood which is associated with oxidative stress and inflammation, and enhanced body fat content, which is associated with augmented concentration of the substance.7
In East Harlem, a substantial proportion of the population is comprised of immigrants from Central and South America8 in whom metabolic syndrome, a risk factor for fatty liver, prevails. In this context, DM and HTN were significantly prevalent in the Hispanic group. Hispanic ethnicity, however, is heterogeneous thus nonalcoholic fatty liver disease (NAFLD) cannot be generalized to all subjects from this group. In support of this idea is a study that reported that persons of Central American background had a higher prevalence of NAFLD as compared to that from Caribbean origin (e.g. Puerto Rico, Dominican Republic, and Cuba) and these differences were not explained by modifiable factors such as diet or physical ac-tivities.9 Accordingly, we hypothesize that Hispanic ethnicity of a certain nature increases the vulnerability to ALD perhaps by genetic susceptibility to fatty liver that may be worsened by alcohol, the threshold of which to cause liver injury may be decreased in Hispanic subjects compared to other ethnic and racial groups.