A 77 years old male patient presented five years earlier with painless jaundice and symptomatic cholangitis requiring hospital admission. He was fit and well otherwise. An endoscopic retrograde cholangio-pancreatography (ERCP) showed intra- and extra-hepatic biliary stricturing and beading suggestive of sclerosing cholangitis. No apparent triggers such as gallstones or inflammatory pancreatitis were identified, and he had no other systemic symptoms. He continued to suffer from recurrent attacks of cholangitis despite treatment with ursodeoxycholic acid 500 mg twice daily (14 mg/kg). This was mostly managed at home using short courses of oral antibiotics. He subsequently developed recurring symptoms of lethargy, itching and loss of appetite which resulted in 5.5 kg weight loss. This required further hospitalization three years after the initial presentation. Bilirubin levels were mostly normal and alkaline phosphatase approximately twice the upper limit of normal. A magnetic resonance cholangio-pancreatography (1.5 Tesla MRCP) showed a new 3 cm long common hepatic duct (CHD) indeterminate stricture near the hilum along with sclerosing cholangitis-related features previously demonstrated on ERCP. Blood CA19.9 was 58kU/L (normal range 0–27) and IgG4 levels were normal. EUS showed a 10 mm hilar lymph node with benign cytology using 25G FNA. He was referred to our unit for further cholangioscopic characterisation using single operator peroral cholangioscopy (SOPC; Spyglass DS® Boston Scientific).
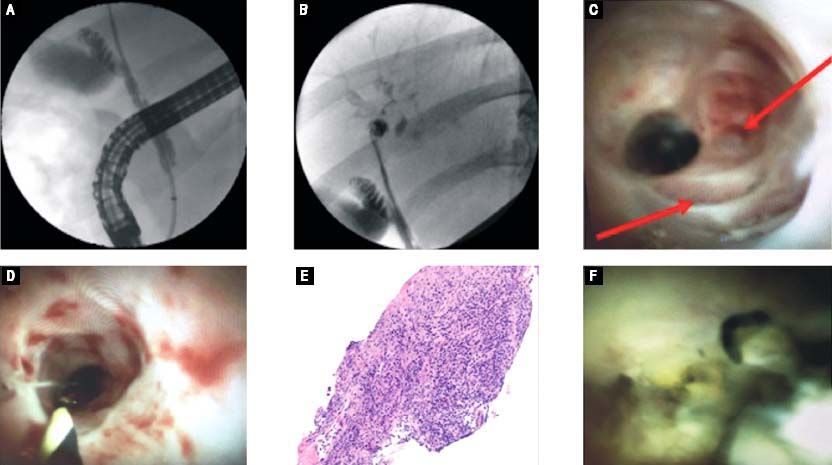
Initial cholangiography showed CBD indentations and a strictured CHD followed by prominent intra-hepatic beading of biliary radicles (Figures 1A and 1B). Common bile duct (CBD) intubation with SOPC did not show the usual smooth pearly appearance but instead demonstrated a fibrotic-appearing duct with numerous band-like scars and diverticulae, identified by the red arrows (Figure 1C). More proximally, stricturing was prominent in the common hepatic duct (CHD) and initially the 10.5Fr SpyGlass DS® cholangioscope could not pass. Following 6 mm intraductal balloon dilatation (Titan® balloon, Cook Medical) the cholangioscope could traverse the CHD stricture to access hilar structures. Post-dilatation disruption of the biliary mucosa can be seen post-balloon dilatation (Figure 1D). This revealed small stone fragments and debris, likely secondary to chronic cholestasis in the biliary tree (Figure 1F). Analysis of cytology brushings and biliary (Spybite®) biopsies confirmed benign appearances with no evidence of cholangiocarcinoma (Figure 1E). Balloon dilatation was performed in an attempt to access hilar ducts and improve biliary drainage. On follow up 1-year post-dilatation, the patient had an uneventful course with no further attacks of cholangitis.
A. ERCP cholangiography showing CBD indentations and strictured CHD. B. Prominent intra-hepatic biliary radicle beading. C. Cholangioscopy appearances of the distal CBD showing “trachealisation”, diverticulae (red arrows) and a narrow CHD stricture. D. cholangioscopic appearances of the CHD stricture post-balloon dilatation showing post dilatation disruption of the biliary mucosa. E. Biopsy obtained from the common hepatic duct stricture. F. Proximal cholangioscopic appearances showing small stone fragments and debris.
Primary sclerosing cholangitis (PSC) is a progressive disease of the liver. In the absence of a reversible causative factor it can result in cirrhosis and hepatic decompensation, as well as cause recurrent progressive suppurative cholangitis.1 Direct endoscopic examination and sampling using cholangioscopy may help to distinguish between malignant or benign causes of biliary structuring including IgG4 disease, secondary sclerosing cholangitis and cholanagiocarcinoma.2,3 However, understanding and interpreting cholangioscopic endoscopic images alone to make a diagnosis can be unreliable and further improvements in image and tissue acquisition (e.g. biopsy size) will make diagnosis more robust.4 Careful examination of the MRCP images in multidisciplinary team settings in this case triggered the referral for cholangioscopy. This lead to a definitive diagnosis and management after four years of cholangitis.
Competing Interest- •
WF: None declared.
- •
NT: None declared.
- •
MJ: Advisor to Boston Scientific and Cook Medical.
Not commissioned, internally peer reviewed.
ConsentPatient informed consent was obtained for publication.