Introduction. There is significant geographic variation in the etiology and prognosis of acute liver failure (ALF). Since, little information is available for Latin America. We analyzed ALF mortality trends in Mexico.
Material and methods. The rates of mortality attributable to ALF were obtained for 1998 to 2009 from the National System of Health Information in Mexico and analyzed according to date, etiology, sex, age and geographic characteristics through graphical assessment and joinpoint regression.
Results. From 1998 to 2009, 2,193 ALF-related deaths were reported. A threefold increase in ALF mortality was observed during the period from 1998 to 2009 (the global mortality rate increased from 13.1 to 40.2 deaths per 10,000,000 inhabitants). The most significant increase was observed for viral etiologies after 2006, affecting people 45 years old and over.
Conclusion. ALF-related deaths have increased since 2006. Although we cannot speculate on the specific causes of this increase, it may reflect improvements in the access of vulnerable populations to health care.
Acute liver failure (ALF) is an uncommon but life-threatening liver disease, characterized by the presence of acute liver damage, encephalopathy, coagulopathy and jaundice. ALF can be divided in hyperacute (less than seven days from the onset of encephalopathy), acute (more than eight days, but less than four weeks from the onset of encephalopathy) and subacute (more than four weeks from the onset of encephalopathy).1
The epidemiology of ALF is heterogeneous, being geographic variations and age the most relevant factors in the pattern of disease etiology. This etio-logical variation could affect the prognosis and therapeutic options.2 ALF is considered a rare disease, with an incidence rate of 10-60 cases per 10,000,000 inhabitants in developed countries.3,4 The ALF mortality rate fluctuates depending on its severity and on access to liver transplantation, and ranges from 13 to 33%.5,6 ALF has a significant impact on liver transplantation programs, accounting for 9-11% of transplants. Liver transplantation significantly reduces ALF mortality, but access to it is still limited.6 In developed countries, the consumption of acetaminophen and other drugs has overtaken viral infection as the primary cause of ALF, accounting for at least 50% of cases.2,7 However, in developing countries, information regarding the epidemiology of ALF is scarce. The aim of this study was to analyze the data for ALF from the nationwide statistics registry of Mexico.
Material and MethodsThe mortality databases were obtained from the National System of Health Information (available at http://www.sinais.salud.gob.mx/basesdedatos/index.html; accessed September 2, 2011) for every year from 1998 to 2009. The databases contained all deaths registered in Mexico, coded under the International Classification of Diseases version 10 (ICD-10) for the general cause of death, specific cause of death, place of death, age, sex and other socioeconomic variables. Census data from the National Population Council were used to estimate the Mexican population on July 1 in each year of the period examined, overall and by age groups, sex and region (available at http://www.conapo.gob.mx; accessed July 13, 2011).
The ALF-related deaths were classified into two general types based on the ICD-10 descriptors:
- •
B-codes. Including deaths caused by B150 (hepatitis A, with hepatic coma). B160, acute hepatitis B with delta agent, with hepatic coma. B162, acute hepatitis B without delta agent, with hepatic coma; and B190, unspecified viral hepatitis, with hepatic coma; and
- •
K-codes. Including deaths caused by K720 (acute and subacute hepatic failure), K760 (fatty change in the liver, not otherwise classified), K762 (central hemorrhagic necrosis of the liver) and K763 (infarction of the liver).
The mortality rates were calculated as the number of deaths per 10 million inhabitants per year. The calculated mortality rates were regressed over the calendar year using joinpoint regression to test for changes in mortality trends over time. Briefly, joinpoint regression uses an algorithm that tests whether a multisegmented line is a significantly better fit than a straight or less-segmented line, thus identifying break points in the trend, called joinpoints. Each joinpoint denotes a statistically significant (P = 0.05) change in the trend.8 In our analysis, a maximum of three joinpoints (four line segments) were allowed for each model. The data were analyzed using PASW® (PASW Statistics Version 18.0.9, 2009; IBM, Chicago, IL, USA) and the Joinpoint Regression Program, Version 3.5.9
Geographic differences in the ALF mortality rates were assessed using the regional divisions of the country proposed by the National Institute of Statistics, Geography and Informatics, as follows:
- •
Zone 1. Guerrero, Oaxaca and Chiapas.
- •
Zone 2. Campeche, Tabasco, Veracruz, Puebla, Hidalgo and San Luis Potosí.
- •
Zone 3. Michoacán, Guanajuato, Zacatecas, Durango and Tlaxcala.
- •
Zone 4. Morelos, Estado de México, Querétaro, Nayarit, Colima, Sinaloa, Yucatán and Quintana Roo.
- •
Zone 5. Tamaulipas, Chihuahua, Sonora, Baja California and Baja California Sur.
- •
Zone 6. Nuevo León, Coahuila, Jalisco and Aguascalientes; and
- •
Zone 7. Mexico City.
A separate linear regression line was fitted for each zone for the 1998-2006 and 2007-2009 periods to identify differences in the slopes of the ALF mortality rates between periods and regions.
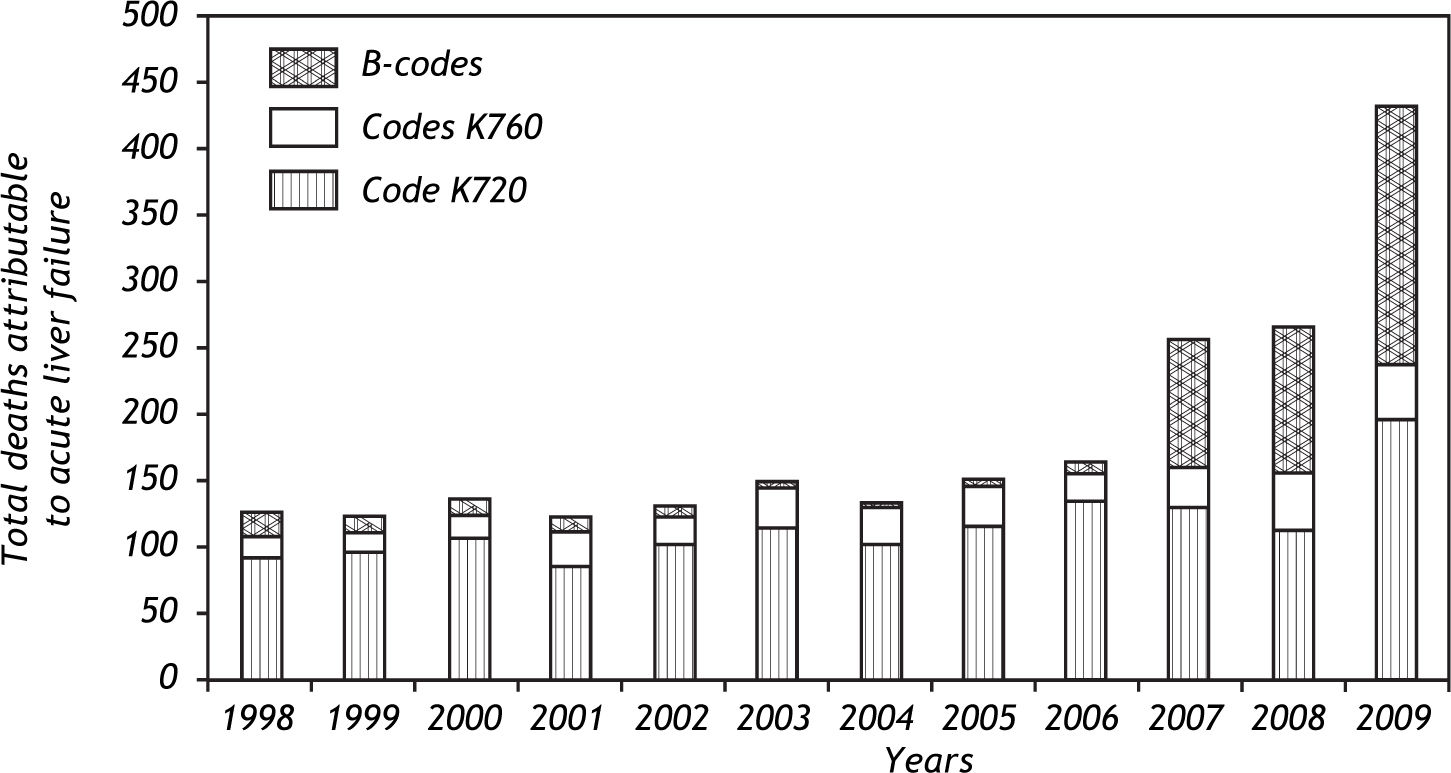
ResultsFrom 1998 to 2009, 2,193 deaths attributable to ALF were reported. From 1998 to 2006, the number of ALF-related deaths remained stable, averaging 137 deaths per year. After 2006, ALF-related deaths from all causes increased steadily, although viral etiologies showed a steeper increase, accounting for the highest number of deaths in 2009 (Figure 1).
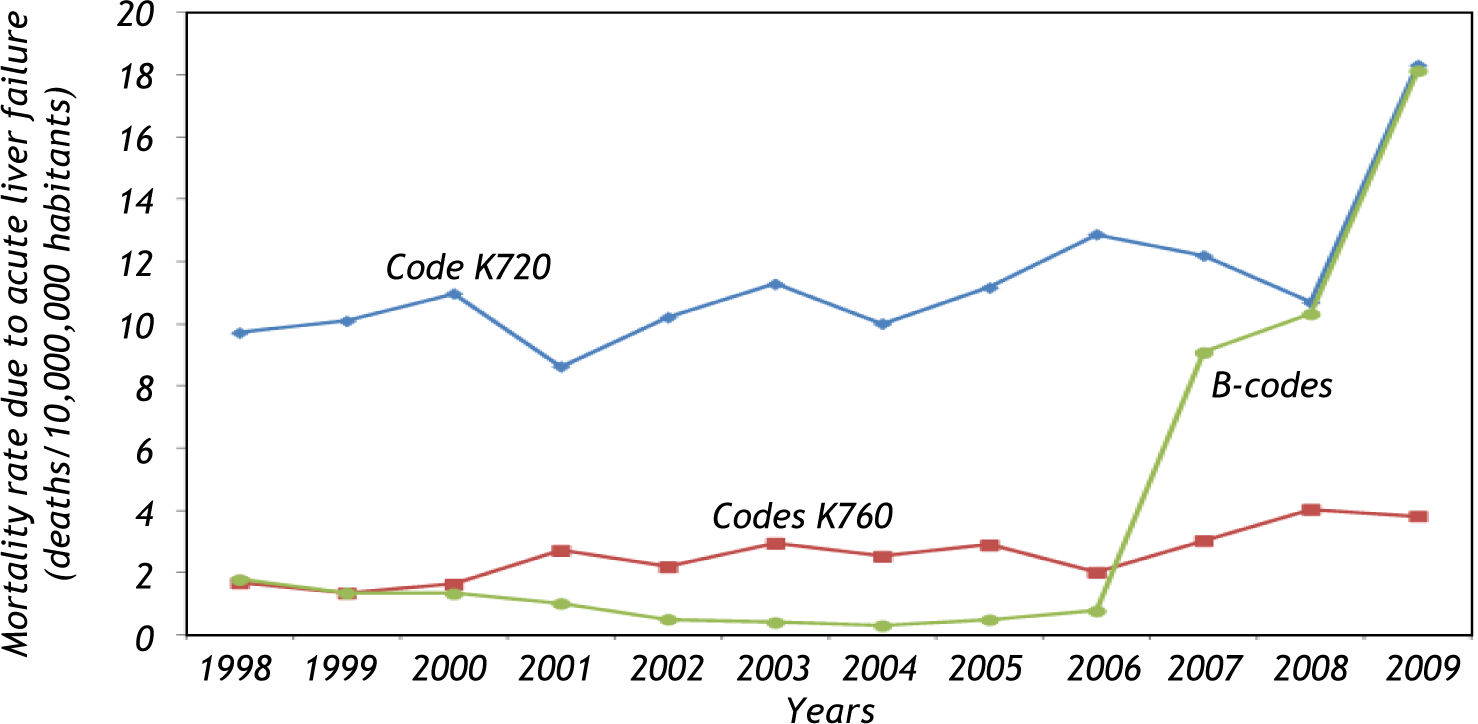
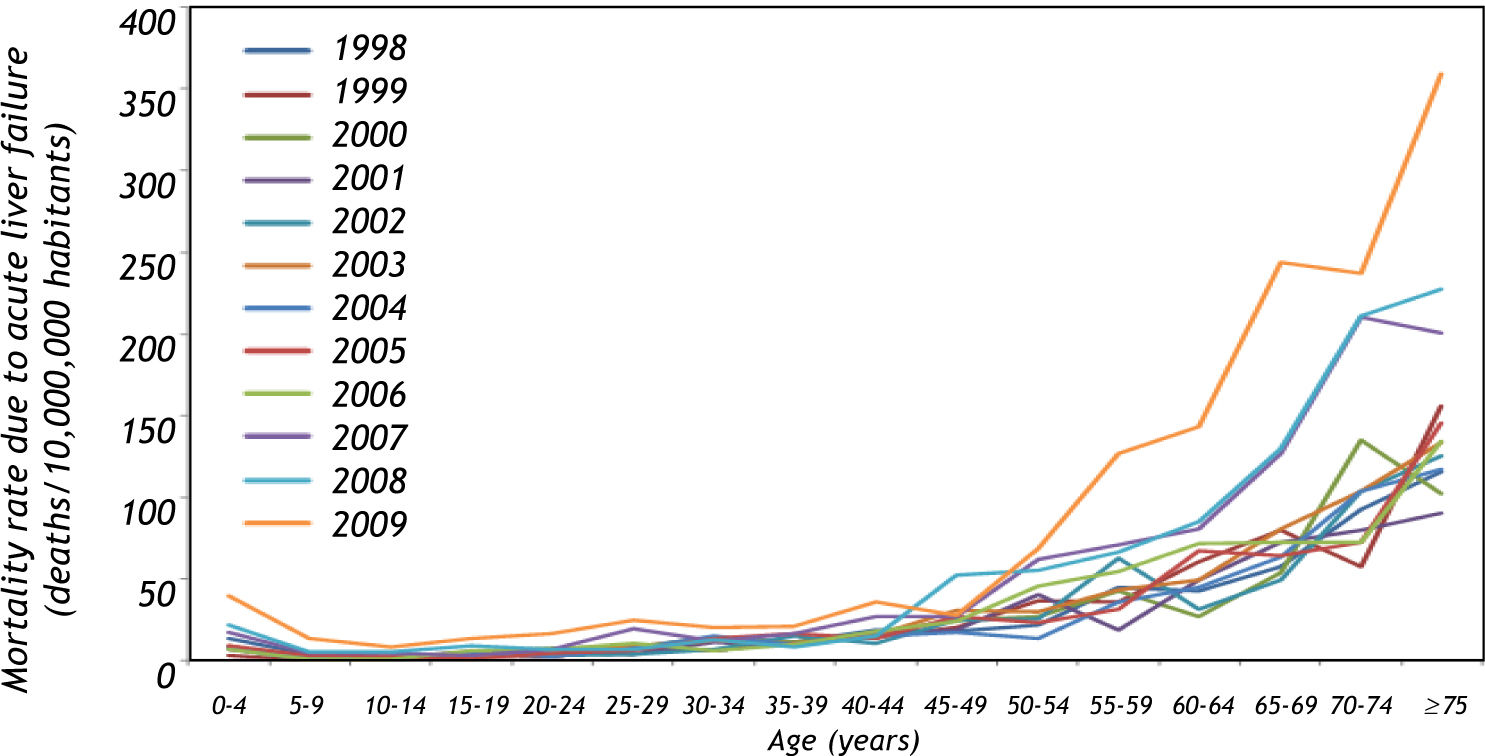
The mortality rates behaved in a similar manner. Deaths classified as K720 showed a twofold increase from 1998 to 2009 (from 9.1 to 18.3 deaths per 10,000,000 inhabitants). Similarly, K760 showed a 2.3-fold increase for the same period (from 1.67 to 3.81 deaths per 10,000,000 inhabitants) (Figure 2). A 10-fold increase in deaths was observed from 1998 to 2009 for the B-code etiologies (from 1.8 to 18.1 deaths per 10,000,000 inhabitants). Overall, ALF-related mortality experienced a threefold increase from 1998 to 2009 (from 13.1 to 40.2 deaths per 10,000,000 habitants). Higher mortality rates, as well as increased rates over time, were concentrated in the group of patients over 45 years old, particularly after 2006 (Figure 3). No differences by sex were observed.
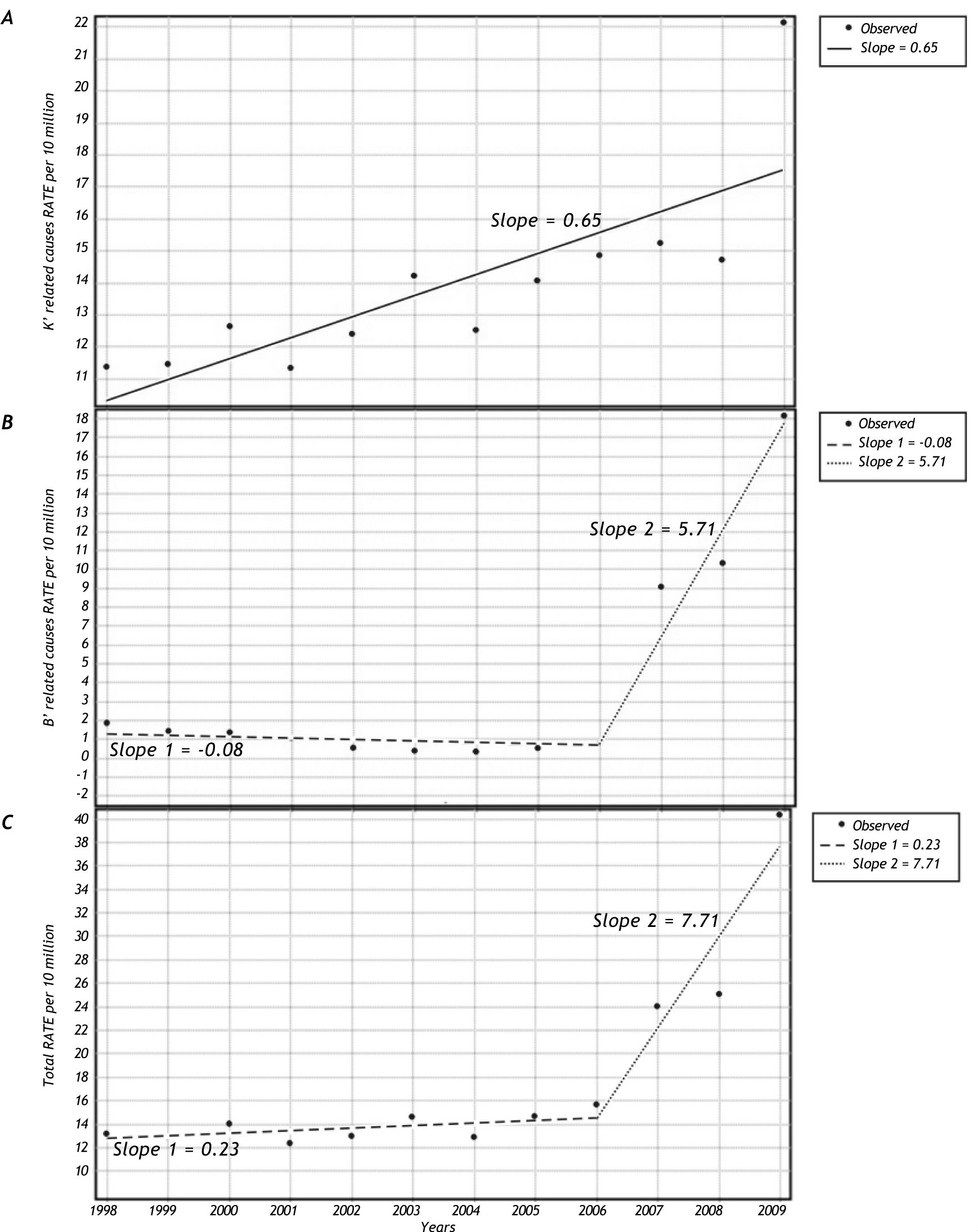
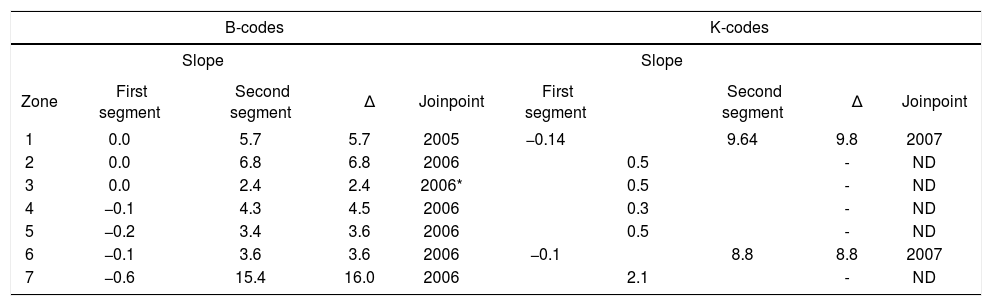
The trends in ALF-related mortality displayed important increases after 2006 (Table 1). Joinpoint analysis revealed that across all regions of Mexico, deaths attributable to viral causes (B-codes) showed an average increase of six deaths per year after 2006 compared with previous years (Figure 4); the increases were remarkably high for Mexico City (zone 7). For the K-code deaths, an increase of nine deaths per year was observed after 2007 in zones 1 (Guerrero, Oaxaca and Chiapas) and 6 (Nuevo León, Coahuila, Jalisco and Aguascalientes); the other zones maintained the same slopes over time.
Geographic analysis of the mortality rate slopes for 1998-2006 and 2007-2009.
| B-codes | K-codes | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Slope | Slope | ||||||||
| Zone | First segment | Second segment | Δ | Joinpoint | First segment | Second segment | Δ | Joinpoint | |
| 1 | 0.0 | 5.7 | 5.7 | 2005 | −0.14 | 9.64 | 9.8 | 2007 | |
| 2 | 0.0 | 6.8 | 6.8 | 2006 | 0.5 | - | ND | ||
| 3 | 0.0 | 2.4 | 2.4 | 2006* | 0.5 | - | ND | ||
| 4 | −0.1 | 4.3 | 4.5 | 2006 | 0.3 | - | ND | ||
| 5 | −0.2 | 3.4 | 3.6 | 2006 | 0.5 | - | ND | ||
| 6 | −0.1 | 3.6 | 3.6 | 2006 | −0.1 | 8.8 | 8.8 | 2007 | |
| 7 | −0.6 | 15.4 | 16.0 | 2006 | 2.1 | - | ND | ||
ND: not detected.
ALF is a rare but lethal disease with important geographic variations in its etiology and prognosis. To the best of our knowledge, this is the first national analysis of ALF in Latin America. Some reports have previously been published involving pediatric populations.10,11 and infectious etiologies of ALF.12 We analyzed the records of ALF-related mortality in Mexico for 11 years. The most striking finding was the increase in the number of deaths in the last three years of the period. Mortality increased for all etiologies, but hepatitis-related ALF caused by hepatitis A and B viruses and undetermined viruses showed the largest increases.
Because of the secondary and ecological nature of the present study, we are unable to provide a causal explanation for the increase in ALF mortality. However, some considerations can be examined to help interpret these findings. The incidence of hepatitis infections showed its last peak in Mexico in 1997,13 and has remained steady since then.14 An increase in hepatitis-related ALF mortality with a stable incidence of hepatitis could suggest an increase in lethality. However, the assessment of lethality in this situation is difficult because no information on the time lag between hepatitis onset and ALF development exists, precluding any meaningful statements about lethality. Therefore, the current cases of ALF could reflect the 10-year lag since the 1997 hepatitis peak well as present concurrent development of hepatitis and ALF.
We relied on national records to assess these trends, which are subject to reporting bias and changes in the probability of disease detection arising from changes in access to health care. The simultaneous increase in all etiologies and across sexes suggests an improvement in the registration of ALF patients, probably resulting from improved access to health care. ALF is an expensive disease, requiring relatively advanced technological resources to establish an etiological diagnosis. Mexico has recently undergone an extensive reform in health-care access through Seguro Popular, a subsidized governmental system created to provide access to health care for the previously uninsured population. From 2004 to June 2011, 48.5 million people became affiliated with Seguro Popular, many of whom belong to vulnerable groups (Informe de resultados 2011, available at: http://www.seguro-popular.gob.mx//images/contenidos/Informes_Resultados/informe_resultados_1sem_2011.pdf). Because Seguro Popular provides coverage for catastrophic expenses and facilitates access to health care, it is reasonable to expect that previously untreated cases of ALF will now be properly diagnosed and followed up. This could explain the increase in ALF mortality, particularly among the elderly.
Another likely explanation is an increase in the vulnerability of the population infected with hepatitis. It is well known that many populations with a formerly high prevalence of hepatitis A viral infections are moving toward medium prevalence in response to improved sanitation. At the same time, hepatitis infections in adulthood have increased as a result of intravenous drug use and sexual transmission, which are also important risk factors for HIV infection, which is still increasing in Mexico.15 Recently, some reports have shown that a large proportion of the adult population infected with hepatitis is also infected with HIV. The comorbidity of HIV and hepatitis has been linked to worse health outcomes, including mortality.16,17 Finally, local conditions, such as the rare but still prevalent practice of paying plasma donors, could also contribute to the increase in ALF.18
It is important to note that there are sociogeographic variations in the main causes of ALF. This joint analysis showed slight temporal and geographic variations. Probably the most relevant is the general increase in B-code disease, but the increase in K-code disease in only zones 1 and 6 is also remarkable. This should encourage local researchers to identify the regional epidemiological characteristics and to develop preventive and therapeutic strategies.
Regardless of the specific causes of the increase, 1,121 ALF-related deaths occurred from 2006 to 2009. During the same period, only 383 patients underwent orthotopic liver transplantation for all causes (available at http://www.cenatra.salud.gob.mx/interior/trasplante_estadisticas.html; accessed October 1, 2011). This mismatch highlights the dramatic shortage of organs required to accommodate at least the patients who most urgently require liver transplantation. In the current scenario, the vast majority of patients affected by ALF will succumb to the ominous natural history of the disease. This should encourage the development of alternative stratagems to promote living-donor liver transplantation,19 to improve the management of these patients in critical care units, and to promote research into prognos-tic20,21 and therapeutic options.
This study was based on administrative data, and some limitations are intrinsic to this methodology. Moreover, other causes of acute liver failure were not included (e.g., acetaminophen, autoimmune disease, Amanita phalloides consumption).
ConclusionIn conclusion, in this study, we have shown an increase in the mortality attributable to ALF in Mexico, which was greater in people older than 45 years, with slight geographic variations. These findings warrant further research to determine the real cause of this increase in ALF-related mortality.
Abbreviations- •
ALF: Acute liver failure.
- •
ICD-10: International Classification of Diseases version 10.
Partially supported by Medica Sur Clinic & Foundation.