Abstracts of the 2021 Annual meeting of the ALEH (Asociación Latinoamericana para el Estudio del Hígado)
More infoPredicting short-term mortality in patients with cirrhosis and bacterial infections is challenging.
AimsTo compare the performance of various scores in predicting in-hospital mortality in this population.
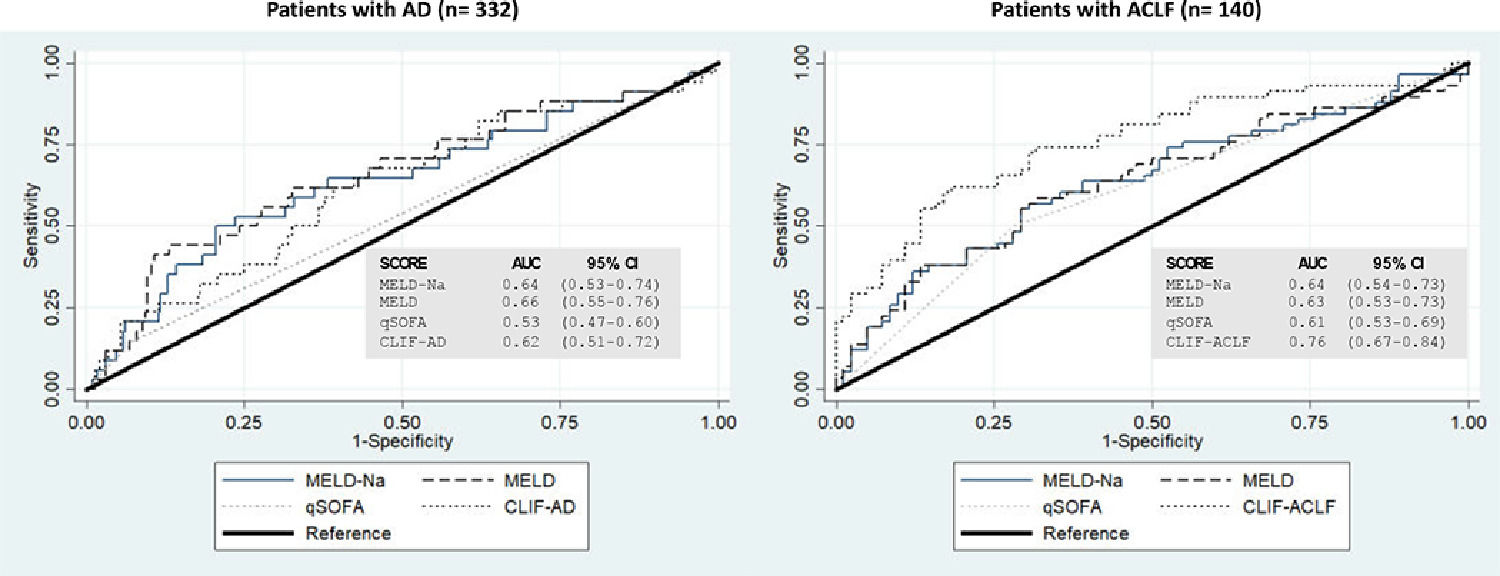
MethodsWe performed an analysis of the multicenter prospective cohort study of patients with cirrhosis with bacterial infections throughout Argentina and Uruguay (clinicatrials.gov.NCT03919032). Patients were classified according to the CLIF criteria as having ACLF or mere acute decompensation (AD). We evaluated the performance of scores of liver disease and infection severity in predicting in-hospital mortality. MELD, MELD-Na, and Quick SOFA (qSOFA) were computed in all patients. CLIF-AD was only computed in patients without ACLF, and CLIF-ACLF only in patients with ACLF. We plotted ROC curves and estimated their area under the curve (AUROC).
ResultsWe included 472 patients: 66% male, mean age 57 ± 12 years. Most frequent infections: SBP (30%) and urinary tract infection (25%). Overall, 332 (70%) patients had acute decompensation, and 140 (30%) ACLF. In-hospital mortality rate was 19%: 41% in patients with ACLF vs 10% in patients with AD (p<0,001). When we evaluated the AUROC of the entire cohort, MELD and MELD-Na performed similarly: 0.74 (95% CI 0.68-0.81) and 0.74 (95% CI 0.67-0.80), respectively; whereas qSOFA showed the lowest performance: 0.62 (95% CI 0.57-0.68). When evaluating only patients with ACLF, CLIF-ACLF performed significantly better than the other ones: AUROC 0.76 (95% CI 0.67-0.84, p =0.01). All scores performed poorly in patients with AD (Figure).
ConclusionThe best tool to predict in-hospital mortality in patients with infection-related ACLF was the CLIF-ACLF score. In patients with infection-related AD, all scores performed poorly. Evaluation of the scores performance is of paramount importance in different regions and for each complication of cirrhosis separately.