Decompensated cirrhosis carries high inpatient morbidity and mortality. Consequently, advance care planning is an integral aspect of medical care in this patient population. Our study aims to identify do-not-resuscitate (DNR) order utilization and demographic disparities in decompensated cirrhosis patients.
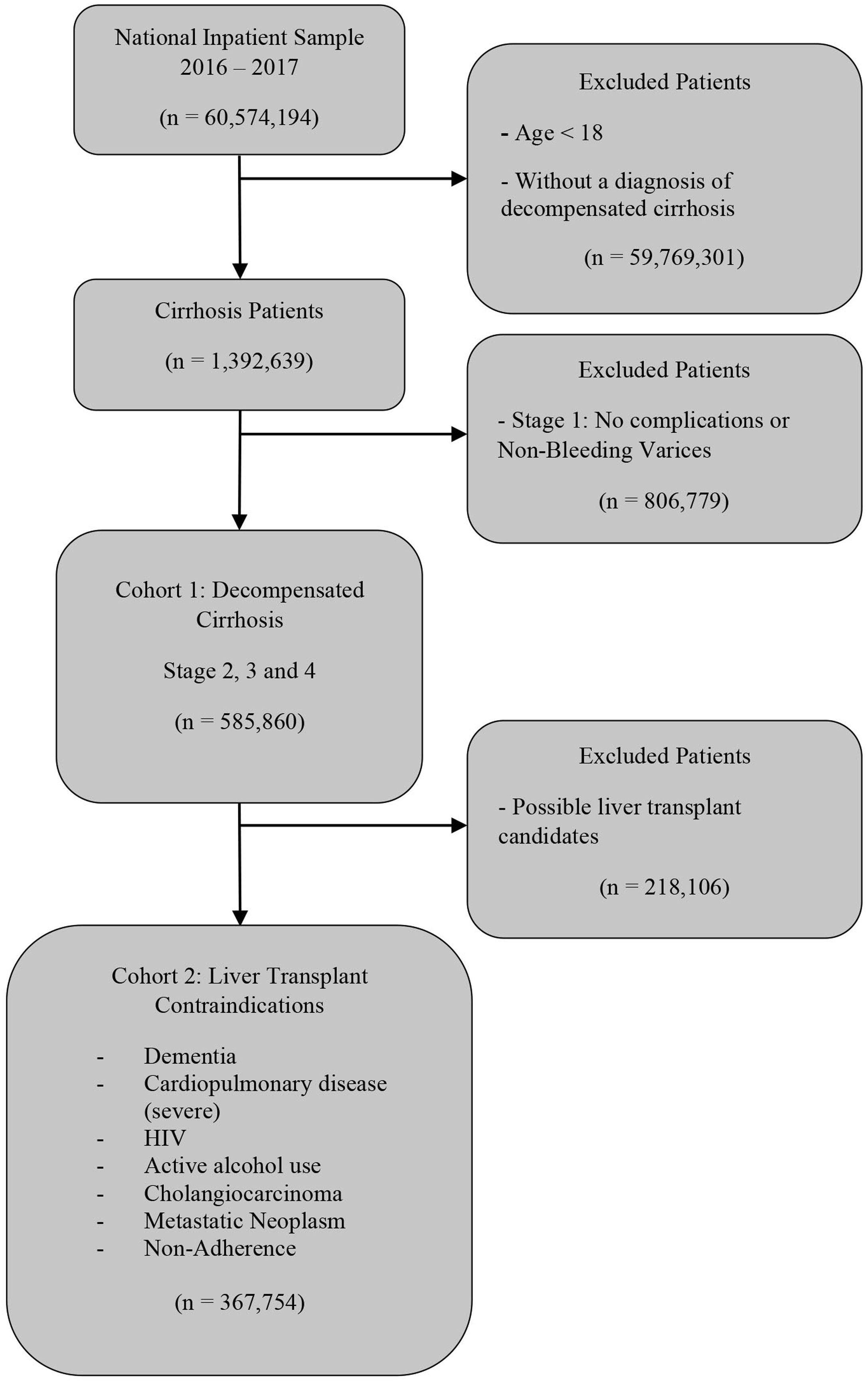
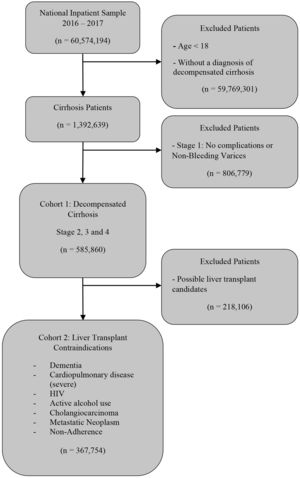
Patients or materials and methodsNationwide Inpatient Sample was used to extract the cohort of patients from January 1st, 2016 to December 31st, 2017, based on the most comprehensive and recent data. The first cohort included hospitalized patients with decompensated cirrhosis. The second cohort included patients with decompensated cirrhosis with at least one contraindication for liver transplantation.
ResultsA cohort of 585,859 decompensated cirrhosis patients was utilized. DNR orders were present in 14.2% of hospitalized patients. DNR utilization rate among patients with relative contraindication for liver transplantation was 15.0%. After adjusting for co-morbid conditions, disease severity, and inpatient mortality, African-American and Hispanic patient populations had significantly lower DNR utilization rates. There were regional, and hospital-level differences noted. Moreover, advanced age, advanced stage of decompensated cirrhosis, inpatient mortality, and relative contraindications for liver transplantation (metastatic neoplasms, dementia, alcohol misuse, severe cardiopulmonary disease, medical non-adherence) were independently associated with increased DNR utilization rates.
ConclusionsThe rate of DNR utilization in patients with relative contraindications for liver transplantation was similar to patients without any relative contraindications. Moreover, there were significant demographic and hospital-level predictors of DNR utilization. This information can guide resource allocation in educating patients and their families regarding prognosis and outcome expectations.
Liver cirrhosis resulting in end-stage liver disease (ESLD) is increasingly prevalent in the United States (US), affecting approximately 5.5 million people (2% of the population), with high hospitalization and readmission rate due to decompensation events [1–4]. These events include the development of ascites, variceal bleeding, spontaneous bacterial peritonitis (SBP), hepatic encephalopathy (HE), and hepatorenal syndrome (HRS). The annual prevalence of decompensated cirrhosis related hospitalizations is 5–7%, and they are associated with high inpatient mortality between 6–12% [5–8].
Due to the high inpatient morbidity and mortality, advance care planning is an integral aspect of medical care in decompensated cirrhosis patients. As a result, the health-care team needs to identify the resuscitation status during hospitalization. Do-not-resuscitate (DNR) orders are implemented based on the directive of the patient, family, or guardian, after consultation with a health-care provider, to respect the patient’s wishes regarding end of life care. Lack of DNR orders in the patient’s chart is usually presumed to be full code, suggesting to the provider that the patient should receive aggressive measures. A meta-analysis of 150 studies showed that approximately 61.8% of patients with chronic conditions do not have documented advance directives on file [9]. A study conducted to understand the patterns of care and end-of-life preference uncovered that 66% of ESLD patients preferred resuscitation efforts, including cardiopulmonary resuscitation (CPR) when asked about resuscitation status [10,11]. Another study demonstrated that 16% of ESLD patients in teaching hospitals had DNR orders compared to 47% of patients with metastatic lung cancer [12]. The same study also discovered that house-staff were less likely to discuss resuscitation status with ESLD patients despite awareness of their poor prognosis.
Several factors would guide the discussion about resuscitation status: patient’s current quality of life, personal values and goals, medical literacy, the likelihood of CPR success, post-CPR prognosis, and liver transplant eligibility [13,14]. The factors affecting DNR order utilization in cirrhosis patients are poorly understood because of the heterogeneity of influences and subjectivity of the decision. We aim to explore the demographic and hospital-level predictors of DNR order utilization.
2Material and methods2.1Design and data sourceThe cohort of patients was extracted from the Nationwide Inpatient Sample (NIS) database of the Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality (AHRQ) [15]. NIS is the largest dataset of hospitalized patients available in the United States. The dataset consists of a stratified sample of approximately 20% of all hospital admissions in the United States, excluding rehabilitation hospitals and long-term acute care hospitals. The dataset provides national estimates based on the discharge weights [16]. Consequently, we can obtain approximately 35 million weighed discharges every year, representing 95% of the US hospitalizations [16]. Primary and secondary diagnoses within the study population were identified using the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes.
2.2Study criteriaWe chose to evaluate the time period from January 1st, 2016, to December 31st, 2017, based on the most comprehensive and recent data. Discharge records with missing information for mortality or primary diagnoses were eliminated according to a scheme suggested by AHRQ [17]. A cohort of adult patients with decompensated cirrhosis was generated using a staging model.
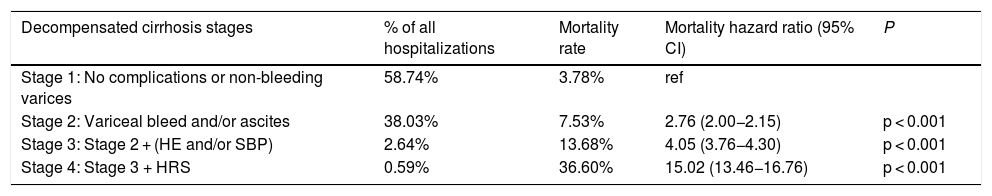
Cirrhosis admissions were distributed in four stages in rising pathology and mortality levels, as previously described [7]. Stage 1 includes no complications or non-bleeding varices, stage 2 includes variceal bleeding and/or presence of ascites, stage 3 includes HE and/or SBP, and stage 4 includes HRS. Each subsequent stage can include complications from the prior stages. Such a staging mechanism has been suggested to predict exponentially rising inpatient mortality [7]. Patients with no complications, i.e., stage 1, were excluded due to lower inpatient mortality rates. Stages 2–4 were included in the first cohort of hospitalized decompensated cirrhosis patients to analyze DNR utilization in a higher mortality cohort of patients (Fig. 1).
A subsequent cohort of patients with relative liver transplantation contraindications was generated using the following co-morbidities based on governmental and society guidelines [18,19]: dementia, severe cardiopulmonary disease, human-immuno-deficiency virus (HIV) infection, alcohol misuse, cholangiocarcinoma, metastatic neoplasm, and medical non-adherence.
2.3Definition of variablesThe dataset has demographic variables including age, gender, race, household income per patient zip-code, patient’s insurance, and hospital-related variables such as bed-size, the region in the US, teaching status, and urban/rural location of the hospital.
ICD-10-CM codes used in this study are equivalent to the ICD-9-CM codes used in the prior studies [20,21]. They include DNR (Z66), cirrhosis (K70.3, K74), Ascites (R18, K70.31), esophageal varices with/without bleeding (I85), bleeding esophageal varices (I85.01, I85.11), hepatic encephalopathy (K72.01, K72.11, K72.91), SBP (K65.2), and HRS (K76.7). Additional ICD-10-CM for co-morbidities are included in the Supplemental Table S1. Severe cardiopulmonary disease was determined by the patient having either a diagnosis of heart failure or lung disease and being oxygen dependent.
2.4OutcomesThe study’s primary outcome was to establish the DNR utilization rate in decompensated cirrhosis patients and analyze the demographic and hospital disparities of DNR utilization. The secondary outcome was to evaluate DNR utilization in decompensated cirrhosis patients with contraindications for liver transplantation.
2.5Statistical analysesAnalyses were performed using Stata, version 16.0 (StataCorp, College Station, TX). NIS is based on an intricate sampling design that includes stratification, clustering, and weighing. This software facilitates analysis to produce nationally representative unbiased results, variance estimates, and p values.
We compared the baseline characteristics between patients with DNR orders and patients with presumed full code orders. We utilized the chi-squared test for categorical variables, Student t-test for normally distributed continuous variables, and Wilcoxon rank-sum test for non-normally distributed continuous variables. Univariate analysis of patient demographics, hospital characteristics, and patient co-morbidities with a threshold of p < 0.1 was used to generate a multivariate regression model with the covariates mentioned above to identify the predictors of DNR utilization.
3Results3.1Cohort selectionA cohort of 585,860 patients was generated, as outlined in Fig. 1. Patients with stage 1 cirrhosis (n = 806,779), including no decompensating events and non-variceal bleeding were excluded. Patients with stage 1 cirrhosis represented the majority of the hospitalizations (Table 1). Decompensated cirrhosis stage 2–4 represented decreasing proportions of hospitalizations. The mortality rate increases exponentially with each increasing stage. Multivariate regression modeling after adjusting for demographic and hospital-level characteristics suggest a similar rise in the mortality hazard ratio (Table 1).
Multivariate Logistic Regression model predicting mortality based on cirrhosis decompensation events.
| Decompensated cirrhosis stages | % of all hospitalizations | Mortality rate | Mortality hazard ratio (95% CI) | P |
|---|---|---|---|---|
| Stage 1: No complications or non-bleeding varices | 58.74% | 3.78% | ref | |
| Stage 2: Variceal bleed and/or ascites | 38.03% | 7.53% | 2.76 (2.00−2.15) | p < 0.001 |
| Stage 3: Stage 2 + (HE and/or SBP) | 2.64% | 13.68% | 4.05 (3.76−4.30) | p < 0.001 |
| Stage 4: Stage 3 + HRS | 0.59% | 36.60% | 15.02 (13.46−16.76) | p < 0.001 |
Abbreviations: CI, confidence-interval; ref, reference; HE, hepatic encephalopathy; SBP, spontaneous bacterial peritonitis; HRS, hepato-renal syndrome.
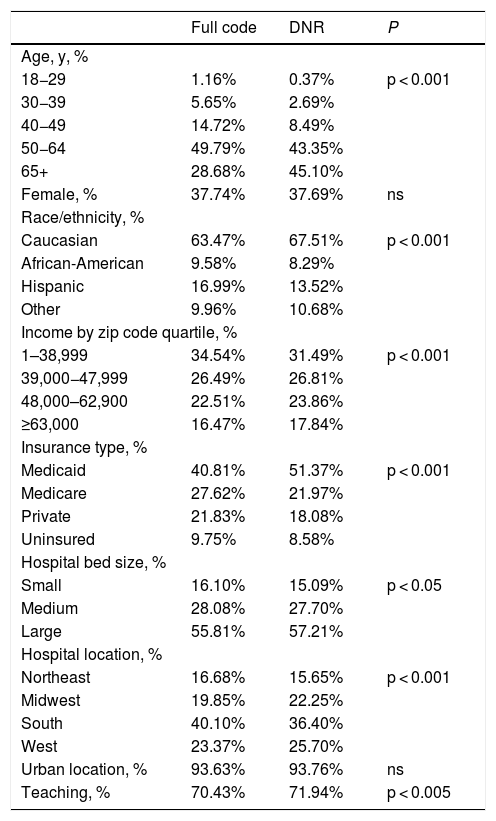
Overall, 14.22% of decompensated cirrhosis patients had DNR code status associated with their hospitalization. There were differences in demographics and hospital-level characteristics between the cohorts of patients with DNR status and full code (Table 2). Notably, older age groups and Caucasian patients had a higher DNR utilization rate.
Demographics and hospital-level characteristics of decompensated cirrhosis patients by do-not-resuscitate (DNR) status.
| Full code | DNR | P | |
|---|---|---|---|
| Age, y, % | |||
| 18−29 | 1.16% | 0.37% | p < 0.001 |
| 30−39 | 5.65% | 2.69% | |
| 40−49 | 14.72% | 8.49% | |
| 50−64 | 49.79% | 43.35% | |
| 65+ | 28.68% | 45.10% | |
| Female, % | 37.74% | 37.69% | ns |
| Race/ethnicity, % | |||
| Caucasian | 63.47% | 67.51% | p < 0.001 |
| African-American | 9.58% | 8.29% | |
| Hispanic | 16.99% | 13.52% | |
| Other | 9.96% | 10.68% | |
| Income by zip code quartile, % | |||
| 1–38,999 | 34.54% | 31.49% | p < 0.001 |
| 39,000−47,999 | 26.49% | 26.81% | |
| 48,000–62,900 | 22.51% | 23.86% | |
| ≥63,000 | 16.47% | 17.84% | |
| Insurance type, % | |||
| Medicaid | 40.81% | 51.37% | p < 0.001 |
| Medicare | 27.62% | 21.97% | |
| Private | 21.83% | 18.08% | |
| Uninsured | 9.75% | 8.58% | |
| Hospital bed size, % | |||
| Small | 16.10% | 15.09% | p < 0.05 |
| Medium | 28.08% | 27.70% | |
| Large | 55.81% | 57.21% | |
| Hospital location, % | |||
| Northeast | 16.68% | 15.65% | p < 0.001 |
| Midwest | 19.85% | 22.25% | |
| South | 40.10% | 36.40% | |
| West | 23.37% | 25.70% | |
| Urban location, % | 93.63% | 93.76% | ns |
| Teaching, % | 70.43% | 71.94% | p < 0.005 |
Abbreviations: DNR, do-not-resuscitate; ns, non-significant.
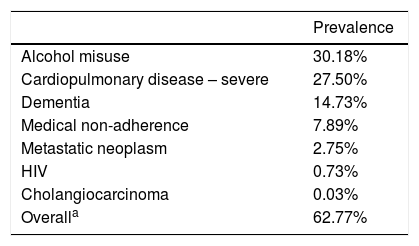
A total of 62.77% of patients were included in the second cohort of patients with at least one contraindication for liver transplant eligibility (Fig. 1). Overall, 15.20% decompensated cirrhosis patients with at least one contraindication for liver transplant eligibility had DNR code status. Current alcohol misuse and severe cardiopulmonary diseases were the most common contraindications for liver transplant eligibility (Table 3). Dementia, medical non-adherence, metastatic neoplasms were also significantly represented.
Prevalence of medical conditions and patient characteristics resulting in contraindication of liver transplant eligibility.
| Prevalence | |
|---|---|
| Alcohol misuse | 30.18% |
| Cardiopulmonary disease – severe | 27.50% |
| Dementia | 14.73% |
| Medical non-adherence | 7.89% |
| Metastatic neoplasm | 2.75% |
| HIV | 0.73% |
| Cholangiocarcinoma | 0.03% |
| Overalla | 62.77% |
Abbreviations: HIV, human immunodeficiency virus.
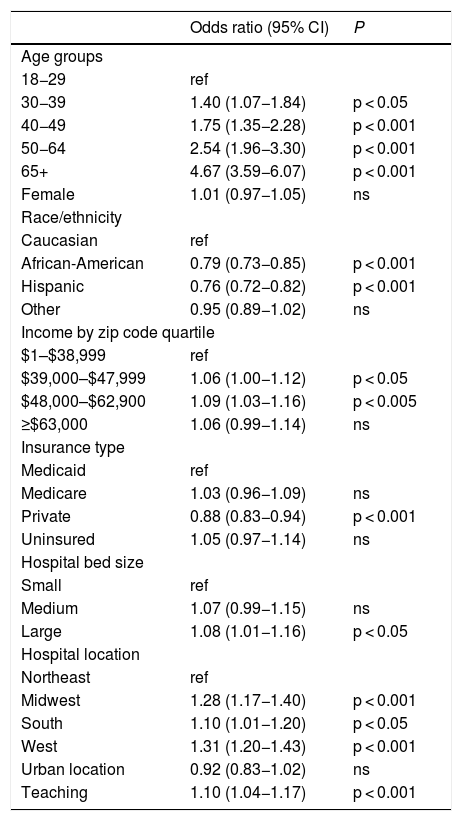
There were significant demographic and hospital-level predictors of DNR utilization in the first cohort of decompensated cirrhosis patients (Table 4). Notably, younger age groups, and minority racial groups (African American, Hispanic) had significantly lower DNR utilization rates in our multivariate regression model. Additionally, areas with higher median income, larger hospitals, and teaching hospitals had modestly higher DNR utilization rates.
Multivariable Logistic Regression Model of significant predictors of do-not-resuscitate (DNR) utilization in decompensated cirrhosis patients.
| Odds ratio (95% CI) | P | |
|---|---|---|
| Age groups | ||
| 18−29 | ref | |
| 30−39 | 1.40 (1.07−1.84) | p < 0.05 |
| 40−49 | 1.75 (1.35−2.28) | p < 0.001 |
| 50−64 | 2.54 (1.96−3.30) | p < 0.001 |
| 65+ | 4.67 (3.59−6.07) | p < 0.001 |
| Female | 1.01 (0.97−1.05) | ns |
| Race/ethnicity | ||
| Caucasian | ref | |
| African-American | 0.79 (0.73−0.85) | p < 0.001 |
| Hispanic | 0.76 (0.72−0.82) | p < 0.001 |
| Other | 0.95 (0.89−1.02) | ns |
| Income by zip code quartile | ||
| $1–$38,999 | ref | |
| $39,000–$47,999 | 1.06 (1.00−1.12) | p < 0.05 |
| $48,000–$62,900 | 1.09 (1.03−1.16) | p < 0.005 |
| ≥$63,000 | 1.06 (0.99−1.14) | ns |
| Insurance type | ||
| Medicaid | ref | |
| Medicare | 1.03 (0.96−1.09) | ns |
| Private | 0.88 (0.83−0.94) | p < 0.001 |
| Uninsured | 1.05 (0.97−1.14) | ns |
| Hospital bed size | ||
| Small | ref | |
| Medium | 1.07 (0.99−1.15) | ns |
| Large | 1.08 (1.01−1.16) | p < 0.05 |
| Hospital location | ||
| Northeast | ref | |
| Midwest | 1.28 (1.17−1.40) | p < 0.001 |
| South | 1.10 (1.01−1.20) | p < 0.05 |
| West | 1.31 (1.20−1.43) | p < 0.001 |
| Urban location | 0.92 (0.83−1.02) | ns |
| Teaching | 1.10 (1.04−1.17) | p < 0.001 |
Abbreviations: CI, confidence interval; ref, reference; ns, non-significant.
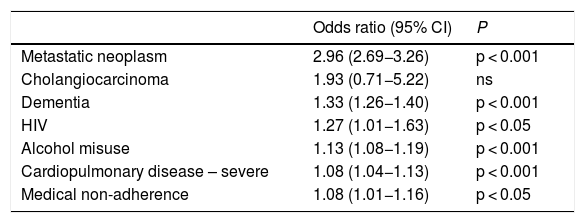
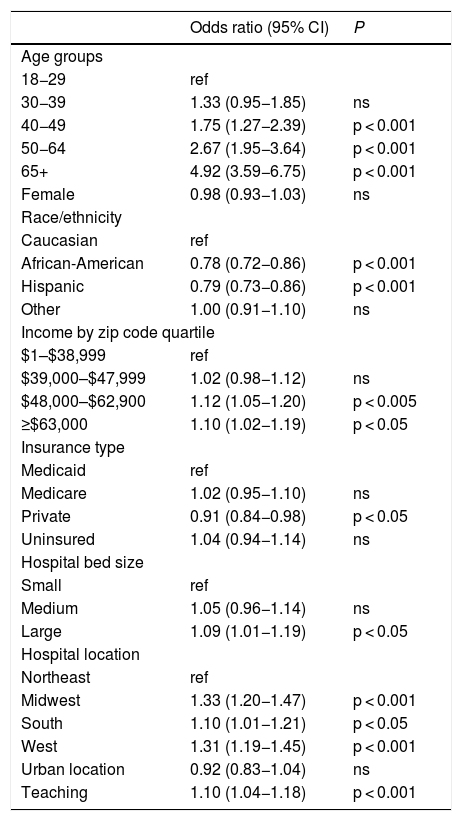
Next, we identified the DNR utilization predictors based on contraindications of liver transplant eligibility (Table 5). Metastatic neoplasms, dementia, HIV were more correlated with DNR status. Alcohol misuse and severe cardiopulmonary disease had modest correlations with DNR utilization. The significant disparities in demographic and hospital-level characteristics persisted in the second cohort of decompensated cirrhosis patients with at least one liver transplant contraindication (Table 6). Younger age groups and minority racial groups (African American, Hispanic) had lower DNR utilization rates. Areas with higher median income, larger hospitals, and teaching hospitals had modestly higher DNR utilization rates.
Multivariable Logistic Regression Model of significant predictors of do-not-resuscitate (DNR) utilization in decompensated cirrhosis patients based on relative contraindications for liver transplant eligibility.
| Odds ratio (95% CI) | P | |
|---|---|---|
| Metastatic neoplasm | 2.96 (2.69−3.26) | p < 0.001 |
| Cholangiocarcinoma | 1.93 (0.71−5.22) | ns |
| Dementia | 1.33 (1.26−1.40) | p < 0.001 |
| HIV | 1.27 (1.01−1.63) | p < 0.05 |
| Alcohol misuse | 1.13 (1.08−1.19) | p < 0.001 |
| Cardiopulmonary disease – severe | 1.08 (1.04−1.13) | p < 0.001 |
| Medical non-adherence | 1.08 (1.01−1.16) | p < 0.05 |
Abbreviations: CI, confidence interval; HIV, human immunodeficiency virus; ns, non-significant.
Multivariable Logistic Regression Model of significant predictors of do-not-resuscitate (DNR) utilization in decompensated cirrhosis patients with at least one relative contraindication for liver transplantation.
| Odds ratio (95% CI) | P | |
|---|---|---|
| Age groups | ||
| 18−29 | ref | |
| 30−39 | 1.33 (0.95−1.85) | ns |
| 40−49 | 1.75 (1.27−2.39) | p < 0.001 |
| 50−64 | 2.67 (1.95−3.64) | p < 0.001 |
| 65+ | 4.92 (3.59−6.75) | p < 0.001 |
| Female | 0.98 (0.93−1.03) | ns |
| Race/ethnicity | ||
| Caucasian | ref | |
| African-American | 0.78 (0.72−0.86) | p < 0.001 |
| Hispanic | 0.79 (0.73−0.86) | p < 0.001 |
| Other | 1.00 (0.91−1.10) | ns |
| Income by zip code quartile | ||
| $1–$38,999 | ref | |
| $39,000–$47,999 | 1.02 (0.98−1.12) | ns |
| $48,000–$62,900 | 1.12 (1.05−1.20) | p < 0.005 |
| ≥$63,000 | 1.10 (1.02−1.19) | p < 0.05 |
| Insurance type | ||
| Medicaid | ref | |
| Medicare | 1.02 (0.95−1.10) | ns |
| Private | 0.91 (0.84−0.98) | p < 0.05 |
| Uninsured | 1.04 (0.94−1.14) | ns |
| Hospital bed size | ||
| Small | ref | |
| Medium | 1.05 (0.96−1.14) | ns |
| Large | 1.09 (1.01−1.19) | p < 0.05 |
| Hospital location | ||
| Northeast | ref | |
| Midwest | 1.33 (1.20−1.47) | p < 0.001 |
| South | 1.10 (1.01−1.21) | p < 0.05 |
| West | 1.31 (1.19−1.45) | p < 0.001 |
| Urban location | 0.92 (0.83−1.04) | ns |
| Teaching | 1.10 (1.04−1.18) | p < 0.001 |
Abbreviations: CI, confidence interval; ns, non-significant.
The literature on factors that may affect DNR order utilization in cirrhosis patients is poorly elucidated. However, CPR utilization rate is two-fold higher among hospitalized patients with cirrhosis than the general patient population [22]. Resuscitation efforts in cirrhosis patients have poor outcomes. Survival after CPR was shown to be less than fifteen percent in patients with cirrhosis [22]. Additionally, a study conducted in a large tertiary university hospital found that patients with liver cirrhosis had at least four-fold increased risk of 90-day-mortality after discharge. This rate was higher than the 1.64-fold increase in mortality in patients with underlying malignancy [20]. Despite the successful return of spontaneous circulation (ROSC), patients with cirrhosis have poor 28-day outcomes. A single centered study showed that 81% of patients with ROSC had unfavorable neurological outcome or died within 28 days following ROSC after CPR administration. Moreover, these patients had a markedly worse profile of organ failure following CPR survival [23]. It is paramount for patients and their families to understand the lack of desirable outcomes after CPR administration in decompensated cirrhosis patients.
This is the first study to analyze DNR utilization in cirrhosis patients in a nationally represented inpatient sample. Our analyses confirm a step-wise exponential increase in mortality rates based on the stages of decompensated cirrhosis [7]. Our cohort’s DNR utilization rate was comparable to smaller single-center studies ranging from 14 to 28% [12,24–26]. The DNR utilization in the cohort of patients with at least one liver transplant contraindication was similar to the overall cohort. We further elucidate that DNR utilization was higher in older, uninsured, and higher-income bracket patients, who were hospitalized in teaching centers, predominantly in larger hospitals in the western and midwestern states. Racially, Hispanic, and African American populations had significantly lower rates of DNR utilization. The demographic and hospital disparities persisted in the cohort of patients with relative contraindications of liver transplantation.
Among the contraindications, irreversible risk factors such as metastatic malignancies and dementia were the significant predictors of DNR utilization likely due to shorter life expectancy and reduced quality of life. Reversible risk factors such as alcohol use disorder and medical non-adherence did not have a clinically significant rise in DNR utilization. Interestingly, severe cardiopulmonary disease also did not have a dramatic rise in the DNR utilization rate and was comparable to patients with no contraindications to a liver transplant. Additionally, the overall difference in the DNR utilization rates between the patients eligible for liver transplantation and the patients with relative contraindications for liver translation was modest. This is consistent with prior studies showing intensive health-care utilization and relatively low palliative care utilization levels in cirrhosis patients during the last year of life regardless of transplant candidacy [24,27,28]. Most of these patients spent one-quarter of their last 90 days of life in the hospital, with a substantial majority requiring ICU (Intensive Care unit) level of care during their terminal hospitalizations [24]. These findings are particularly concerning because patients not eligible for a transplant represent a high-risk population with poor prognosis and no likelihood of cure. The reasons for this phenomenon might be multifactorial. As most patients with a life-limiting illness who discuss the end-of-life care with clinicians are less likely to opt for intensive medical interventions at the end of life, inadequate conversations about goals of care might primarily affect DNR utilization rates [29–35]. A recently published meta-analysis of 11 randomized clinical trials found that CPR treatment discussions with patients led to decreased patients’ CPR preference from 53.6% to 38.6% [35]. Patients could also be unwilling to discuss the end of life issues due to disinterest and inadequate knowledge about CPR [19]. Alternatively, for patients who cannot communicate due to the severity of disease or co-morbidities, the burden of end of life discussions usually rests on the next of kin, who may or may not be aware of the patient’s wishes. However, patients with the highest risk of death/deterioration are more likely not to have family available to help with decision making [19]. Our study has identified a vital disparity in DNR utilization in transplant-ineligible patients and emphasizes the need for improved advanced care planning for a patient population that is particularly vulnerable to receiving intensive resuscitation efforts.
We also show a dramatically lower DNR utilization rate in African American and Hispanic populations, despite accounting for the severity of cirrhosis, co-morbidities, and liver transplantation ineligibility. This is consistent with findings suggesting that minority groups are linked with the higher end of life health-care utilization [36–38]. Less than 9% of African American patients were shown to have advanced care plans compared to 18%–30% of Caucasian Americans [39]. African American patients have been shown to have less access to advance care planning and have a 25% higher preference for CPR and dialysis in a cross-sectional study of 803 terminally ill patients [40]. Hence, it is paramount for patients and their families to have realistic expectations regarding resuscitation outcomes. This study can serve as a point of intervention by hospital administration and health-care teams to identify patients and families lacking medical literacy and/or unrealistic expectations regarding their resuscitation outcomes.
It appears that finances also play a role in a patient’s decision about resuscitation efforts. The most considerable difference was evident in uninsured patients, which can be attributed to lower access to advance care planning and medical resources. Moreover, larger hospitals and teaching hospitals might have more knowledgeable patients about their health status, leading to an informed and more confident decision regarding resuscitation status. These hospitals might also have more resources to help guide patient’s expectations, resulting in higher DNR utilization rates. Further investigations into the disparities between hospitals should be undertaken. Geographic differences have not been previously investigated and might be linked to regional belief systems.
It is important to note the limitations of our study. We are limited by the use of administrative data, which lacks descriptive and qualitative factors affecting disparities in DNR utilization. Given the retrospective study design, there is also a risk for selection bias and unmeasured confounding for the severity of the disease, which might not be accounted for by our multivariate model. Moreover, whether DNR orders were implemented during or prior to hospitalization cannot be determined. Although the relative contraindications for liver transplant used in our study are based on national guidelines, most transplantation centers have their own internal guidelines, which are not accounted by our cohort. Moreover, specific relative contraindications such as uncontrolled sepsis, lack of adequate social support, anatomic abnormalities were not included in the cohort, as such information was not easily extracted from the database. We derive our strength from the nationally represented sample of patients, eliminating local practice patterns that may limit the generalizability of outcomes related to end of life care. We also encourage single and multi-center studies to determine regional DNR order utilization among decompensated cirrhosis admissions.
5ConclusionsThere are dramatic disparities in DNR utilization among hospitalized decompensated cirrhosis patients. We show a lower than expected DNR utilization rate among patients with decompensated cirrhosis with relative contraindications for liver transplantation. Additionally, demographic and regional factors play a significant role in DNR utilization. AbbreviationsESLD End-stage liver disease United States Spontaneous bacterial peritonitis Hepatorenal syndrome Do-not-resuscitate Cardiopulmonary resuscitation Nationwide Inpatient Sample Healthcare Cost and Utilization Project Agency for Healthcare Research and Quality International Classification of Diseases, Tenth Revision, Clinical Modification Human-immuno-deficiency virus Return of spontaneous circulation Intensive Care Unit
Study concept & design: SK, AB
Acquisition of data: SK
Analysis/Interpretation: SK, KG, AB, VR, AP
Drafting: SK, KG, AB, VR, AP
Critical review/revision: SK, KG, AB, VR, AP
Statistical analysis: SK
Declaration of funding sourceThis research did not receive any specific grant from funding agencies.
Conflict of interestThe authors have no conflicts of interest to declare.
The manuscript has not been previously published in any language and is not currently being considered elsewhere for publication.