Hepatitis B virus (HBV) is endemic in Lao PDR, with up to 10% chronic infections in adults. Dentists have high risk of exposure and transmission to their patients. The aim was to investigate the serological profiles of vaccination, exposure and susceptibility to HBV. In addition, we determined the knowledge, attitude and practice (KAP) of Lao dentists toward HBV.
Materials and methodsDentists and dental assistants were recruited from 186 private dental clinics in Vientiane Capital. They completed a KAP questionnaire and serum was tested by ELISA for HBV markers (anti-HB surface antigen, anti-core antigen, HBV surface antigen).
Results206 dentists and 111 dental workers aged between 18–63 years were included. Serology data showed that 37.8% had previous exposure (49.0% of males and 32.4% of females) and 5.0% were chronically infected (7.7% of males and 3.8% of females). Less than 15% had serological evidence of vaccination and 66.8% were unprotected against infection. Knowledge of HBV was mostly low, for example 61.8% were aware of the childhood HBV vaccine. Just over half said that they should give dental care to HBV carriers. About one quarter reported accidental blood exposure during the last 6 months but knowledge about procedures after exposure was low.
ConclusionsLao dentists are at high risk of occupational exposure to HBV but have low awareness and serological protection. There is a need to introduce mandatory vaccination, to strengthen occupational health in health care providers and to further develop the academic curricula of dental students.
Hepatitis B virus (HBV) is a global public health problem which can cause chronic infections, cirrhosis and liver cancer. The virus is spread by blood and other body fluids such as by sexual intercourse, during pregnancy and birth and exposure to contaminated medical equipment. The WHO estimates that there are approximately 260 million chronic carriers of HBV worldwide [1]. Healthcare workers (HCW) have a high risk of accidental percutaneous or mucosal HBV exposure to infected blood or body fluids because of inadequate hygiene measures, particularly in endemic countries [1,2].
In the dental practice, contact with the patient’s blood, oral fluid, and nasopharyngeal secretions, through oral-nasal uptake or accidental needle-stick are the main routes of exposure to HBV [3]. Concern for their own health may even entice dentists to refuse treatment of HBV-infected patients [4]. Conversely, acute or chronically infected dentists may infect their patients. Therefore, dentists should be systematically vaccinated, use personal protection gear and enforce a high level of hygiene in their clinic (gloves, head caps, goggles, etc.) [2,3].
In Lao People’s Democratic Republic (PDR), HBV is highly endemic with a prevalence of HBsAg up to 10% in blood donors [5] and in the general adult population [6], resulting in high morbidity and mortality. The main route of HBV infection in the country is mother-to-child transmission [7]. The HBV containing vaccine given at 6, 10 and 14 weeks was introduced in Lao PDR in 2002. HBV birth dose vaccination was introduced in 2004. However, routine childhood vaccination in the country remains challenging and adults born before HBV vaccine introduction remain largely unprotected [6]. Also, risk populations such as healthcare workers or vulnerable groups have low vaccine coverage and awareness of the disease and its prevention is low [8,9]. In a previous study, we found that even among healthcare workers less than half were protected [10]. However, there are no data on the HBV serological profile of Lao dentists or their risk of infection.
The aim of this study was to determine the HBV serological protection and the prevalence of chronic/acute infection and exposure in Lao dentists and their assistants in private dental clinics in Vientiane Capital. We also determined their knowledge, attitude and practice towards HBV as a secondary aim.
2Materials and methods2.1ParticipantsThis cross-sectional study targeted dentists and dental assistants aged 18–65 years in Nasaythong, Saythany, Sikhottabong, Chanthabouly, Saysettha, Sisattanak and Hatsayfong districts of Vientiane Capital (March and May 2018). The list of clinics was obtained from Lao Dental Association. The clinics were contacted in advance to explain the purpose and method of the study. A sample size of at least 347 was calculated according to the formula N = z2P(1 − P)/d2 where P = 0.08, Z = 1.96 and d = 0.03. We estimated 10% refusal rate. Written informed consent was obtained from all participants.
2.2QuestionnaireFollowing informed consent, the participants completed a KAP questionnaire under guidance of the researchers. The questionnaire included open and closed questions on social demographic characteristics (age, gender, relationship status and years of work), knowledge (symptoms, routes of transmission, risk factors), attitude (concern about HBV, attitude towards infected patients) and practice (hygiene and protection). The questionnaire was pre-tested on 10 dentists.
2.3SerologyAfter completion of the questionnaire, 5 mL of blood was drawn from each participant and the Hepatitis B surface antigen (HBsAg) status was determined by rapid test (Standard Diagnostics, Abbott, USA). The participants were informed of the results, given information on the disease, and, in the case of HBsAg positive participants, advised to visit the district or central hospital for confirmation and advice. All participants were advised how to protect themselves from HBV infection.
Serum was separated by centrifugation and stored at −80 °C until further use. Antibodies against HBV core antigen (Anti-HBc) and surface antigen (anti-HBs) were tested by ELISA (Diasorin, Italy). Anti-HBs positivity was defined as those with titers above 10 mIU/mL. Anti-HBc positive/anti-HBs negative sera were tested for HBsAg by ELISA (Diasorin).
2.4Data analysisData were recorded digitally (Commcare) and then transferred to Excel for cleaning, before importing to STATA version 14 (STATA corp, USA).
Bivariate analysis was done to determine the relationship between anti-HBc and the independent variables. Variables with p-value less than 0.2 were included in the multivariate analysis. After removal of variables with high collinearity, a step-backward approach was used to construct the final model. Only those variables with p-value less than 0.05 were retained.
2.5Ethical considerationsThe study protocol was approved by the National Ethics Committee for Health Research, Ministry of Health, Lao PDR (NECHR 023/2018). Data were presented to the Lao Dental Association as a written and oral report.
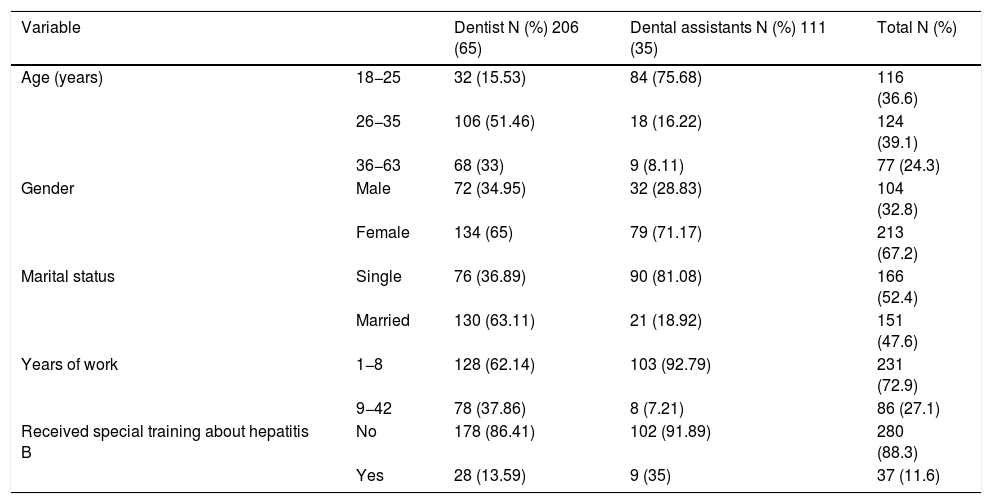
3Results3.1ParticipantsA total of 255 dental clinics were selected to join the study. Of these, 31 (12.1%) clinics could not be located and could not be contacted by phone. 17 (6.7%) clinics were shut down and 21 (8.2%) clinics refused to participate. The reasons for refusal included: already screened for HBV; fear of needles; already vaccinated; busy with patients and “don’t want to be screened”. Thus, 186 clinics participated with 317 staff aged between 18–63 years including 206 dentists (65.0%) and 111 dental assistants (35.0%). The majority of participants were female (67.2%) and about half were married. All dentists had completed 6 years at the Lao University of Health Science. Dental assistants were either dental students or had completed 2–3 years vocational training in dentistry. Very few participants (11.6%) reported to have had received training specifically on HBV (Table 1).
Sociodemographic profile of participants.
| Variable | Dentist N (%) 206 (65) | Dental assistants N (%) 111 (35) | Total N (%) | |
|---|---|---|---|---|
| Age (years) | 18−25 | 32 (15.53) | 84 (75.68) | 116 (36.6) |
| 26−35 | 106 (51.46) | 18 (16.22) | 124 (39.1) | |
| 36−63 | 68 (33) | 9 (8.11) | 77 (24.3) | |
| Gender | Male | 72 (34.95) | 32 (28.83) | 104 (32.8) |
| Female | 134 (65) | 79 (71.17) | 213 (67.2) | |
| Marital status | Single | 76 (36.89) | 90 (81.08) | 166 (52.4) |
| Married | 130 (63.11) | 21 (18.92) | 151 (47.6) | |
| Years of work | 1−8 | 128 (62.14) | 103 (92.79) | 231 (72.9) |
| 9−42 | 78 (37.86) | 8 (7.21) | 86 (27.1) | |
| Received special training about hepatitis B | No | 178 (86.41) | 102 (91.89) | 280 (88.3) |
| Yes | 28 (13.59) | 9 (35) | 37 (11.6) | |
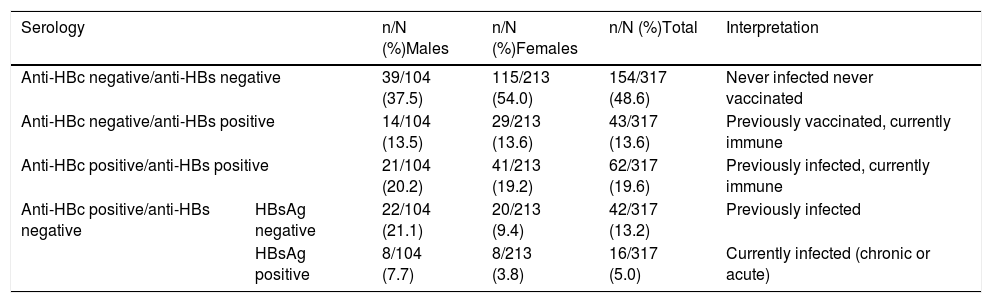
Among 317 participants, 16 (5.0%) were HBsAg positive with more males than females (7.7% and 3.8%, respectively, p = 0.13). 37.8% had a previous infection (anti-HBc positive), again with more males (49.0%) than females (32.4%) (p = 0.004).
Only a few participants (13.6%) had serological evidence of vaccination (anti-HBs positive, anti-HBc negative). However, it is possible that some of the individuals with other serological profiles had been vaccinated too late i.e. after exposure. The majority of participants (66.8%) were anti-HBs negative and therefore not protected against infection. Of the 104 participants who stated that they were vaccinated, only 33.1% had detectable anti-HBs antibodies (Table 2).
Serological profile of participants by ELISA testing.
| Serology | n/N (%)Males | n/N (%)Females | n/N (%)Total | Interpretation | |
|---|---|---|---|---|---|
| Anti-HBc negative/anti-HBs negative | 39/104 (37.5) | 115/213 (54.0) | 154/317 (48.6) | Never infected never vaccinated | |
| Anti-HBc negative/anti-HBs positive | 14/104 (13.5) | 29/213 (13.6) | 43/317 (13.6) | Previously vaccinated, currently immune | |
| Anti-HBc positive/anti-HBs positive | 21/104 (20.2) | 41/213 (19.2) | 62/317 (19.6) | Previously infected, currently immune | |
| Anti-HBc positive/anti-HBs negative | HBsAg negative | 22/104 (21.1) | 20/213 (9.4) | 42/317 (13.2) | Previously infected |
| HBsAg positive | 8/104 (7.7) | 8/213 (3.8) | 16/317 (5.0) | Currently infected (chronic or acute) | |
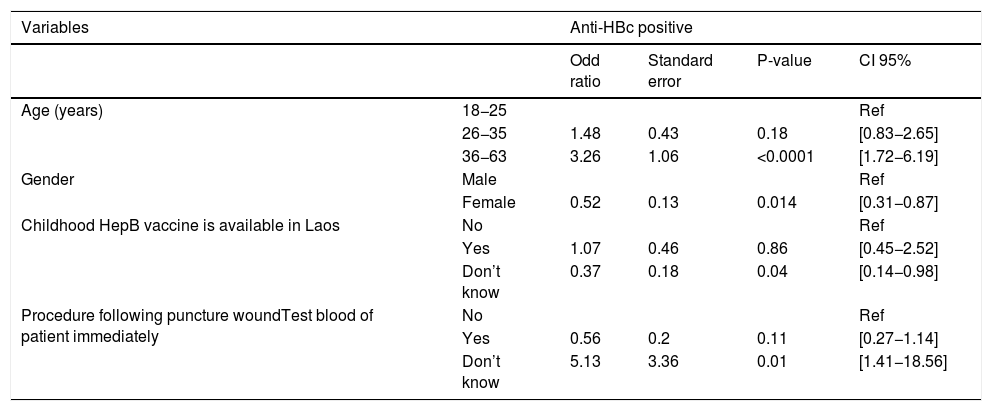
After multivariate analysis, age was significantly associated with HBV exposure. Those over the age of 36 had significantly higher odds to have had exposure compared to those between 18 and 25 (OR 3.26 [1.72−6.19], p < 0.0001). Females had a significantly lower odds of previous exposure to HBV than males (OR 0.52 [0.31−0.87], p = 0.014) (Table 3).
Multivariate analysis associated with anti-HBc.
| Variables | Anti-HBc positive | ||||
|---|---|---|---|---|---|
| Odd ratio | Standard error | P-value | CI 95% | ||
| Age (years) | 18−25 | Ref | |||
| 26−35 | 1.48 | 0.43 | 0.18 | [0.83−2.65] | |
| 36−63 | 3.26 | 1.06 | <0.0001 | [1.72−6.19] | |
| Gender | Male | Ref | |||
| Female | 0.52 | 0.13 | 0.014 | [0.31−0.87] | |
| Childhood HepB vaccine is available in Laos | No | Ref | |||
| Yes | 1.07 | 0.46 | 0.86 | [0.45−2.52] | |
| Don’t know | 0.37 | 0.18 | 0.04 | [0.14−0.98] | |
| Procedure following puncture woundTest blood of patient immediately | No | Ref | |||
| Yes | 0.56 | 0.2 | 0.11 | [0.27−1.14] | |
| Don’t know | 5.13 | 3.36 | 0.01 | [1.41−18.56] | |
All samples were tested with both HBsAg rapid test and HBsAg ELISA: two of the 16 participants positive by ELISA were not detected by rapid test. Conversely, one other participant who tested positive by rapid test was negative by ELISA. A discrepancy of HBsAg results between rapid test (4.7%) and ELISA (5.1%) suggests that there are differences in sensitivity or specificity of the tests.
3.3Knowledge, attitude and practiceKnowledge regarding HBV was mixed but mostly low, especially in the dental assistants as compared to the dentists. For example, 8.2% of the dentists and 18.1% of assistants were not familiar or did not recognize serology as a way to test for Hepatitis B infection. Participants mostly mentioned clinical signs as a way to diagnose the infection. Among those that were familiar with the serology some also indicated serum transaminase (40.7%) and/or clinical signs (20.4%) as a possibility to diagnose the disease. 33.9% of dentists and 45.9% of dental assistants did not know about childhood vaccination against HBV in Lao PDR. Although vaccination was recognized by 94.2% of dentists and 83.7% of assistants as a prophylactic measure, less than 50% knew that HBV can be transmitted by blood and even less about the other routes of transmission.
In concordance with the serology data, less than 30% of participants reported completion of three doses of HBV vaccination. More than 90% use the gloves during contact with patients, used plastic bottles or sharp containers for dispose sharps and needles and washed hands before/after touching patients. Approximately one quarter reportedly had accidental exposure to blood during the past 6 months (26%). Essentially all reported cleaning dental equipment after each patient but 8.2% do not use autoclave to clean the re-usable equipment and used either water and detergent (16/26; 61.5%) or alcohol (8/26; 30.7%) or both (2/26; 33.3%).
4DiscussionPrevious studies have shown that dentists are at high risk of infection e.g. in South Korea, Saudi Arabia and Iran [11–13]. Indeed, in the current study, about one quarter of participants said that they had accidental blood exposure during the last six months. This confirms the high risk of HBV (and other blood-borne infections) in this group. Previous studies have confirmed that HBV infections among healthcare workers are caused by contaminated sharps or different percutaneous injuries such as wire injuries or cuts [14]. Other risks of infection can be blood splashes to the eye, nose or mouth during routine work. Infection of patients within the dental healthcare setting can occur similar ways to the dentists themselves [3]. For example, skin prick with contaminated sharps or use of contaminated equipment such as lancets or scalpels during surgical or routine dental practice. These risks can be mitigated by adequately cleaning or disposing of equipment between patients [14,15]. Most clinics included in our study used plastic bottles rather than special containers for disposal of used sharp /needles. This is probably related to the high cost of appropriate sharps containers. These data suggest an urgent need to raise awareness among dentists regarding the appropriate sharp disposal (e.g. using covered containers) and post-accident procedures (e.g. washing hands with soap, recording details of the incident and checking infectious disease status) [16].
We found that the knowledge of Lao dentists regarding HBV is mixed but generally low. Of note, approximately 20% of dentists and 45% of assistants were unaware that HBV can be transmitted by blood. Even fewer could identify saliva as a route of transmission. Other studies have seen a similar low knowledge in dentists [4,17]. Despite high concern about HBV infection and awareness of HBV vaccination, less than one third of participants reported full vaccination. This gap between desire to be vaccinated and actual number of vaccinated dentists is a concern and maybe indicates a lack of availability or high cost of the vaccine (approximately 17–20 USD per dose). In addition, although most participants confirmed that they cleaned equipment after use, 8.2% did not clean by autoclaving, which is the most effective way to eliminate infectious HBV. Although chemical treatment can greatly reduce the viability of the virus, infection can still occur within the dental care setting if such cleaning is not done thoroughly and therefore autoclaving remains the most robust method [18]. Indeed, without autoclaving or adequate chemical treatment, HBV can remain infectious for several weeks [19]. Furthermore, less than one half had been screened for HBV status.
In this study, approximately two thirds of the participants were serologically unprotected against HBV infection, lacking anti-HBs antibodies. This large proportion of susceptibles is concerning, and is higher than in a previous study in healthcare workers in Lao PDR (47%) [10]. Furthermore, 5.0% and 37.8% of participants were HBsAg and anti-HBc positive, respectively. Females had a lower prevalence of HBsAg (3.8%) than males (7.7%), and significantly lower exposure (32.4% versus 49.04% (OR 0.52 [0.31−0.87], p = 0.014). Other studies in the general population have shown a similar gender bias for HBV exposure and chronic infection [6].
In a previous study on Lao healthcare workers, we that found 8.0% of all participants were HBsAg positive (11.5% of males and 7.1% of females) [10]. The prevalence of anti-HBc was also higher in the previous study (48.8% overall; 59.3% of males and 46.1% of females). Higher exposure in the previous study may be because many participants were older (more chance of exposure), and those with more high-risk activities, such as surgeons.
5ConclusionsWe see high exposure and chronic infection in Lao dentists. This underlies the risk of HBV infection in dentists and onward transmission to patients. The majority of the participants were serologically unprotected against HBV. A particular focus on occupational health should be strengthened in the dentistry school, including awareness of infectious disease risk and preventative measures. Vaccination against HBV could even be provided as a mandatory part of the diploma structure. The Lao dental association could also play a key role in raising awareness among practicing dentists by offering courses or providing material regarding HBV and other occupational risks.
FundingThis work was supported by the Luxembourg Ministry of Foreign Affairs, “PaReCIDS II” grant.
Conflict of interestThe authors declare that there is no conflict of interest. The study was approved by the National Ethics Committee for Health Research, Ministry of Health, Lao PDR (NECHR 023/2018). All participants gave full informed consent to be included. This study did not involve a clinical trial or animals.
The authors would like to thank Bounta Vongphachanh, Latdavone Khenkha and Nouna Innoula who helped with the experiments at IPL. Phimmany Phommavy, a technician from Vientiane Health Department, helped with participant recruitment, and Thongsamoud Vongphukdee and Amphone Bounmanosin drove the research team to all participating dental clinics. We also wish to thank the participants for consenting to give samples for this research.