Compared to premenopausal women, postmenopausal women are at greater risk of developing NAFLD and NASH, two common indications for liver transplantation (LT). We aim to determine the prevalence of NASH-related cirrhosis in postmenopausal women from a cohort of LT patients and investigate their post-LT complications.
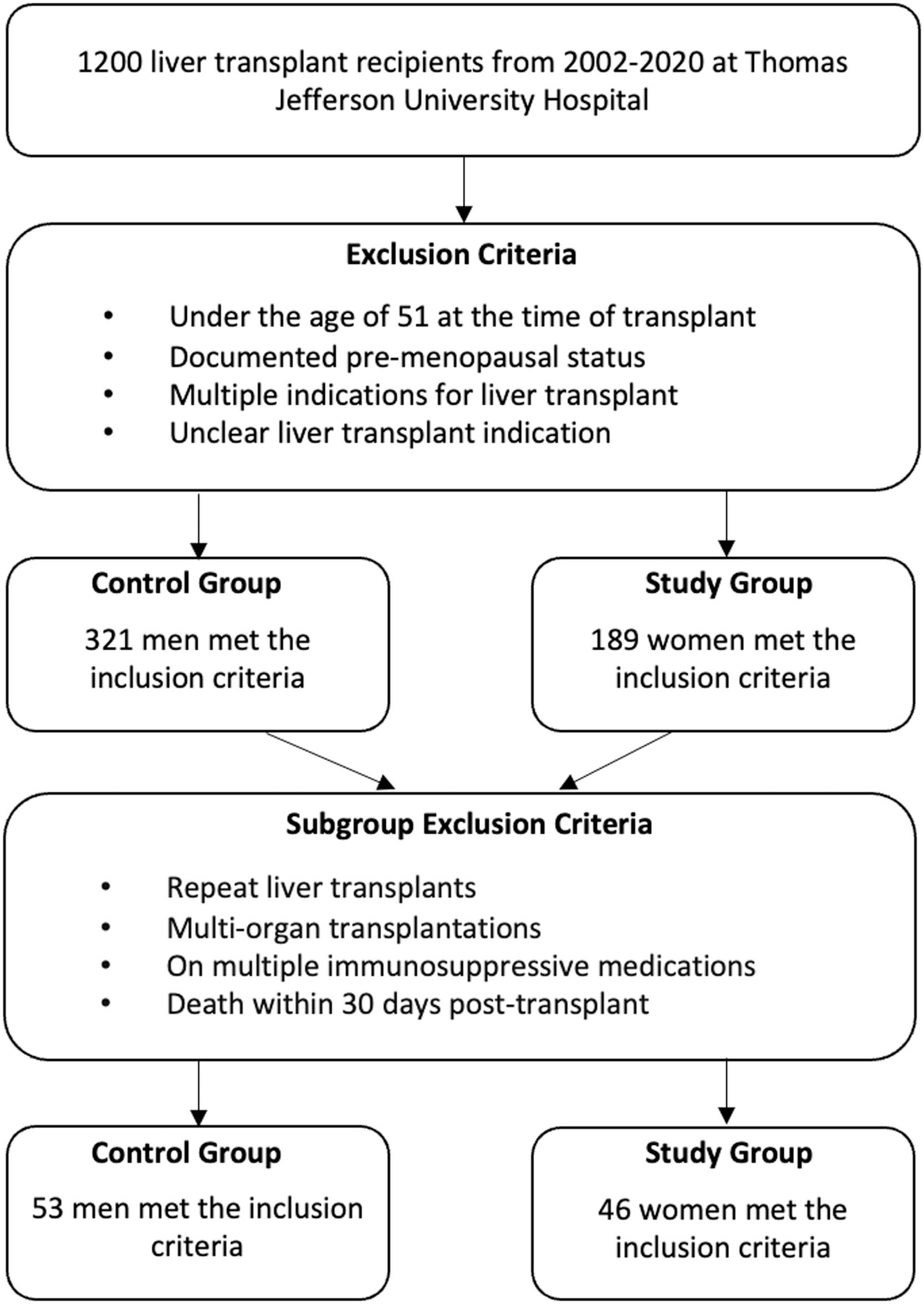
Materials and MethodsChart review of 1200 LT patients from 2002-2020 was performed. Postmenopausal women were defined as women over 51 and compared to a control group of men over 51. Prevalence of LT indications was determined. Subgroup analysis assessed cardiovascular disease risk. BMI and ASCVD risk scores were calculated at the time of LT and after 1 year.
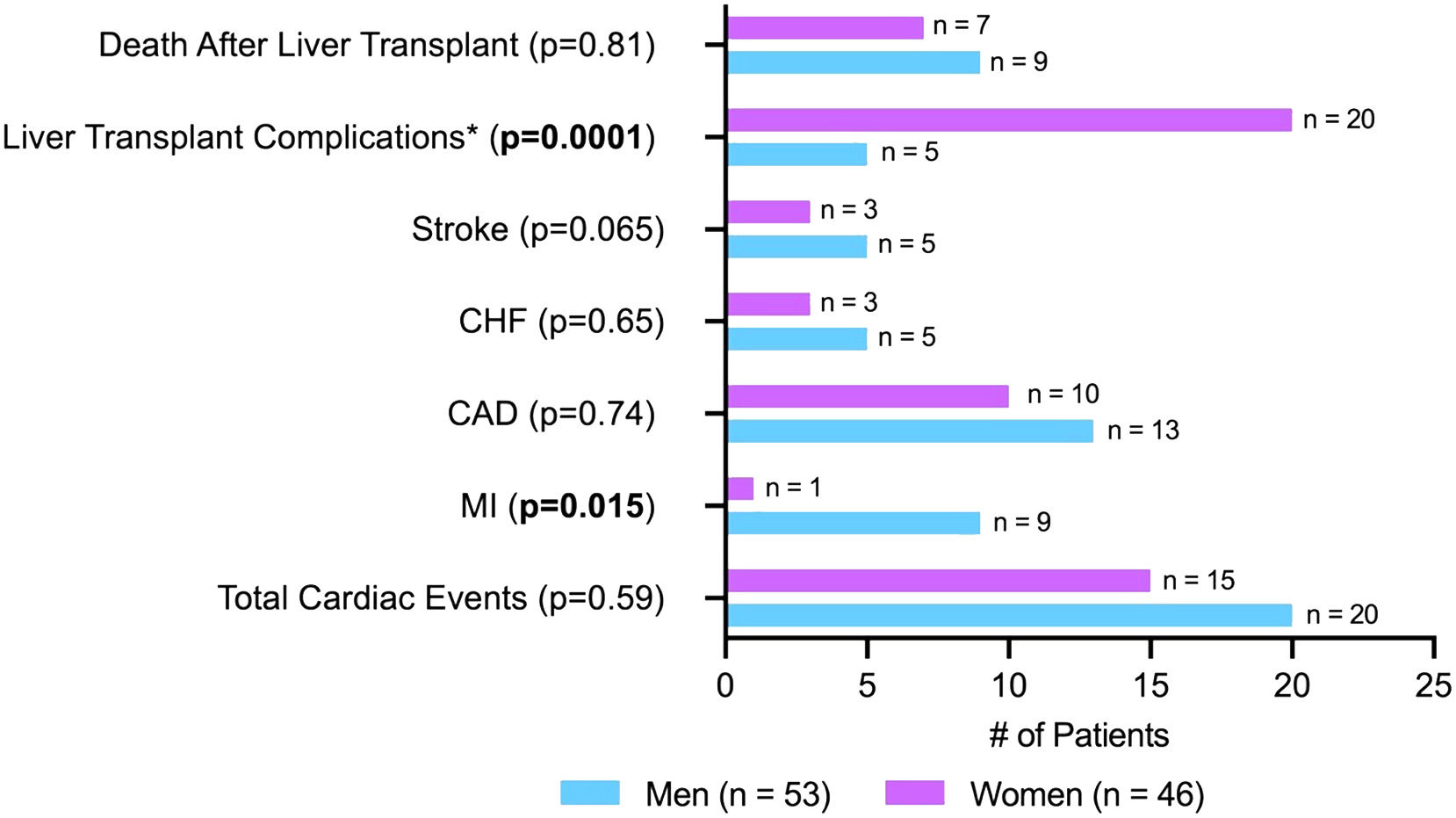
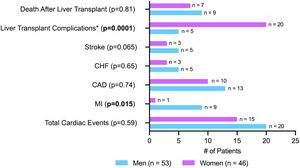
Results510 patients met the inclusion criteria: 189 (37.1%) women and 321 (62.9%) men. The most common indication was NASH for women (26.5%, p<0.001) and alcohol-related cirrhosis for men (23.1%). 53 men and 46 women underwent subgroup analysis. There was no significant difference in BMI or ASCVD 10-year risk post-LT between sexes. MI occurred more in men (n=9.17%) than women (n=1, 2%, p=0.015), with no significant differences in CAD, CHF, or stroke. LT complications occurred less in men (n=5.9%) than women (n=20, 43%, p=0.0001).
ConclusionsPostmenopausal women were significantly more likely to have NASH as an indication for LT than men. Postmenopausal women had greater weight gain and more noncardiac complications than men. Women did not have increased cardiovascular outcomes, ASCVD risk, or mortality. Diet education and weight control in postmenopausal women with existing risk factors for NASH should be encouraged to modulate health outcomes.
Non-alcoholic fatty liver disease (NAFLD) is the most common cause of liver disease globally, affecting about 1 in 4 people [1]. The umbrella of NAFLD ranges from milder forms known as steatosis to more severe and advanced forms like non-alcoholic steatohepatitis (NASH) [1]. NASH has become the leading indication for liver transplantation (LT) in women in the United States [2]. In the U.S., NAFLD is a growing public health concern with increasing prevalence—currently around 24%—and increasing NAFLD-related deaths [3,4]. The apparent prevalence of NAFLD is higher in male individuals until stratifying NAFLD patients by weight, which results in a higher prevalence of NAFLD in non-overweight females than non-overweight males [5,6]. NAFLD is a predictor for increased all-cause mortality and the mortality risk increases with worsening NAFLD histology [7,8]. Women with NAFLD are at an increased risk of all-cause mortality and cardiovascular related mortality as compared to men with NAFLD [3]. Furthermore, studies have found that postmenopausal women are at greater risk of developing NAFLD and NASH compared to premenopausal women [9,10]. Emerging literature suggests that this increased risk of NAFLD/NASH in postmenopausal women is due to a combination of decreased estrogen and metabolic syndromes prior to menopause (e.g., obesity, dyslipidemia, diabetes) [11]. Some have hypothesized that genetic disposition to NAFLD, metabolic syndromes, and high fat and fructose dietary patterns can exacerbate the effect of estrogen deficiency on the development of NAFLD/NASH [11]. The menopause transition period is also believed to be a time of accelerated cardiovascular disease risk [12]. Factors associated with menopause such as declining estrogen, vasomotor symptoms, sleep disturbances, depression, and age at menopause have all been implicated in increasing cardiovascular disease risk [13].
The most common causes of long-term mortality post-LT are cardiovascular disease, renal complications, and infection [14]. Studies have found that women have superior long-term survival post-LT compared to men [15–17]. There is limited literature that specifically investigates outcomes in postmenopausal women post-LT. The purpose of our study was to (1) determine the prevalence of NASH-related cirrhosis in postmenopausal women from a cohort of LT patients and (2) compare post-LT complications in postmenopausal women and men.
2Materials and MethodsWe performed an IRB-approved retrospective study of 1,200 patients who underwent LT at Thomas Jefferson University Hospital (TJUH) from 2002 to 2020. TJUH is a high-volume urban, tertiary liver transplant center. We collected outcomes of interest through chart review of the electronic medical record (EMR), EPIC. Postmenopausal women were defined as women over age 51 (the average age of menopause in the U.S.) and were compared to a control group of postmenopausal men greater than age 51. Patients who were under the age of 51 at the time of LT and women who had clear documentation of premenopausal status on chart review (even if older than 51) were excluded. Despite the potential for overlap in etiologies and pathophysiology leading to LT, patients were excluded if they had multiple indications for LT to more easily distinguish and compare each indication. Patients were also excluded if the LT indication was unclear. Patient age at the time of LT and race were confirmed. Transplant indications for each patient were left up to physician discretion per the chart, with cirrhosis not otherwise specified grouped with cryptogenic cirrhosis. The prevalence of the most common indications of LT was determined for men and women.
A subgroup analysis of postmenopausal men and women was performed to assess cardiovascular disease risk. Patients with more than one LT, multi-organ transplantations, more than one immunosuppressive medication, or death within 30 days post-LT were excluded. Restrictions were made on multiple immunosuppressive medications to limit confounding variables and simplify our analysis with more controlled variables; we sought to limit patients that would be prone to developing complications post-transplant unrelated to our study focus. Fig. 1 summarizes the study participant selection criteria. Atherosclerotic cardiovascular disease (ASCVD) risk scores were calculated at the time of LT and one-year post-LT. We calculated the ASCVD risk scores based on the American College of Cardiology calculator [18]. Body mass index (BMI) was recorded at the time of LT and one-year post-LT. The percent change in ASCVD risk score and BMI was reported at one-year post-LT and compared by sex. Complications post-LT from the time of transplant hospitalization to follow-up were recorded for each patient and divided into cardiac and non-cardiac complications termed “other complications”. Cardiac complications included myocardial infarction (MI), chronic heart failure (CHF), coronary artery disease (CAD), and cerebrovascular accidents (CVA). Other complications post-transplant included acute and chronic rejection, sepsis, chronic kidney disease (CKD), and biliary strictures. The prevalence of each complication was calculated for men and women. Lastly, we assessed the prevalence of post-transplant mortality by sex.
Categorical variables were analyzed using the Chi-Square test. All statistical analysis was completed using STATA. 95% confidence intervals (CIs) were reported and p-values <0.05 were considered statistically significant.
2.1Ethical statementWritten informed consent was obtained from each patient included in the study and the study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a priori approval by the institutional review board of Thomas Jefferson University Hospital (21E.1194).
3ResultsOf the 510 patients who met the inclusion criteria, 189 (37.1%) were women and 321 (62.9%) were men. The average age of the female and male cohorts was 63 and 61 years, respectively. In women, NASH/NAFLD was the most common indication (26.5%) for LT, followed by alcoholic cirrhosis (14.8%) and cryptogenic cirrhosis (13.2%, see Table 1). Women were significantly more likely to have NASH as an LT indication (p<0.001) compared to other indications. In men, alcohol-related cirrhosis was the most common indication (23.1%), followed by Hepatitis C Cirrhosis (21.2%), cryptogenic cirrhosis (19.3%) and then NASH (12.5%, see Table 1).
Indications for liver transplant stratified by sex.
| Indications* | Men (n = 321) | Women (n = 189) |
|---|---|---|
| NASH/NAFLD | 40 (12.4%) | 59 (26.5%) |
| Alcoholic | 74 (23.1%) | 28 (14.8%) |
| HCV | 68 (21.2%) | 23 (12.2%) |
| HBV | 4 (1.2%) | 2 (1.1%) |
| Autoimmune Hepatitis | 6 (1.9%) | 14 (7.4%) |
| PSC | 16 (5.0%) | 16 (8.5%) |
| PBC | 11 (3.4%) | 15 (7.9%) |
| HCC | 33 (10.3%) | 7 (3.7%) |
| DILI | 7 (2.2%) | 9 (4.8%) |
| Cirrhosis NOS / Cryptogenic | 62 (19.3%) | 25 (13.2%) |
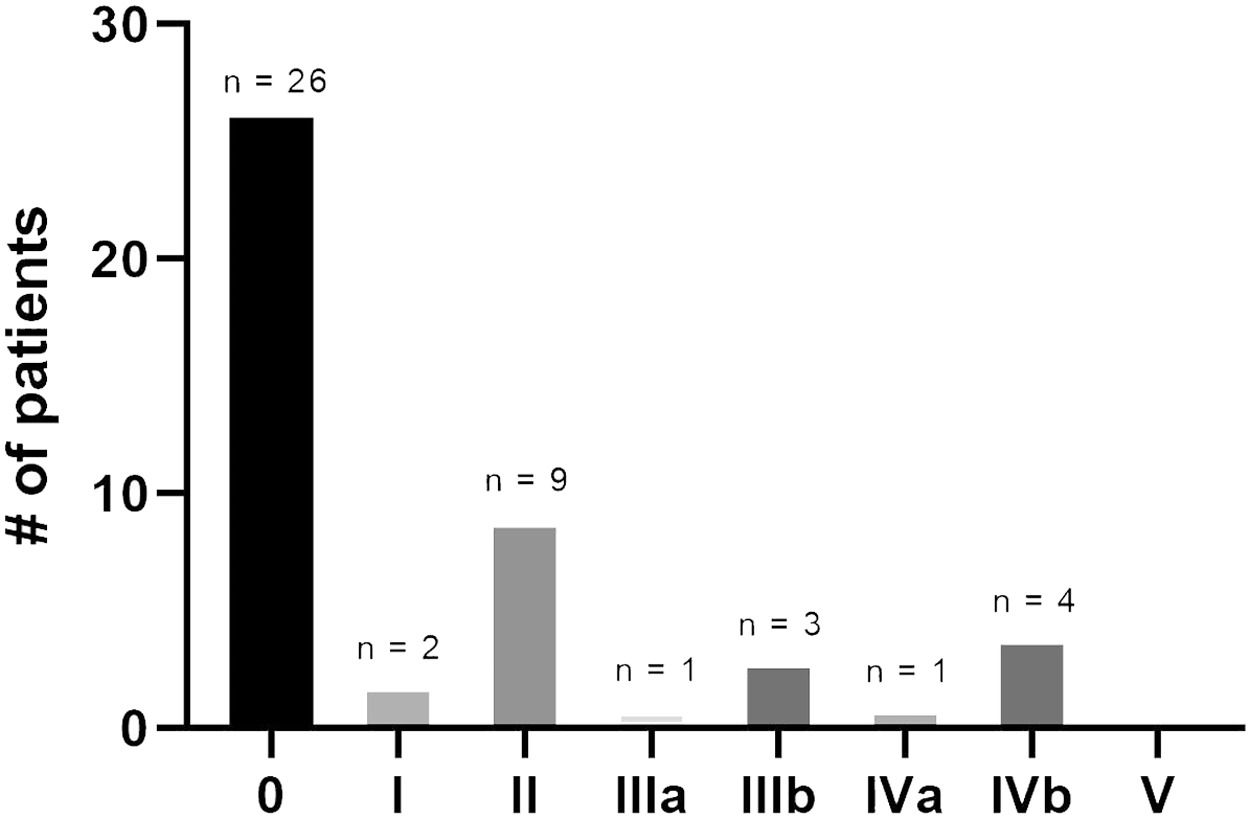
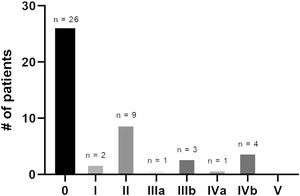
Of these patients, 99 patients (53 men and 46 women) met criteria for subgroup analysis (Table 2). The average age was 61.8 years (95% CI 48.7-74.8) for men and 63.1 years (95% CI 51.0 -75.2) for women. Most men (n=47, 89%) and women (n=38, 83%) racially identified as White. BMI change post-LT was -1.4 (95% CI -10.2-7.4) in men and 0.87 (95% CI -11.1-12.8) in women (p=0.039, Table 2). ASCVD 10-year risk change was 1.3% (95% CI -5.1-7.7) in men and 1.8% (95% CI -5.2-8.8) in women (p=0.44). Average ASCVD 10-year risk at the time of LT and at one-year post-LT was numerically but not statistically higher in men than women, at 8.1% and 9.3% for men and 2.8% and 4.6% for women, respectively (p=0.44, Table 2). Regarding post-transplant outcomes, the overall rate of all major cardiac events was not different between men (n=20, 38%) and women (n=15, 32%, p=0.59, Fig. 2). However, MI occurred significantly more often in men (n=9, 17%) than in women (n=1, 2%, p=0.015). While men had slightly higher occurrences than women of post-transplant CAD (25% vs. 22%, p=0.74), CHF (9% vs. 7%, p=0.65) and CVA (9% vs. 7%, p=0.65), these differences were not statistically significant (p>0.05, Fig. 2). Other LT complications (acute/chronic rejection, sepsis, CKD, or biliary strictures) occurred significantly less often in men (n=5, 9%) versus women (n=20, 43%; p=0.0001, Fig. 2). Of the 20 women affected, 6 had acute/chronic rejection, 3 had sepsis, 6 had biliary strictures, and 5 developed CKD. The Clavien–Dindo system was used to classify and stratify non-cardiac LT complications in women [19]. Fig. 3 shows the distribution of the Clavien–Dindo complication grades in these patients, with grades I-II considered mild and grades III-V severe. Based on this classification, 11 women experienced mild complications and 9 experienced severe complications. However, there was no difference in mortality post-LT in 9 men (17%) and 7 women (15%) (p=0.81).
Summary of subgroup analysis between men and women.
BMI, body mass index; ASCVD, atherosclerotic cardiovascular disease.
NAFLD/NASH is the fastest growing etiology of liver disease amongst LT candidates in western countries [20]. Studies have shown that Hispanic, White, and Asian women are more likely than Hispanic, White, and Asian men to have NASH as the leading indication for LT waitlist registration and LT in the United States. Ovarian senescence has been strongly associated with severe steatosis and fibrosis in NASH and is postulated to be secondary to the development of postmenopausal metabolic syndrome due to estrogen deficiency [21]. Postmenopausal women are more likely to develop metabolic dysfunction and cardiovascular disease compared to premenopausal women [22]. Our study found that postmenopausal women are significantly more likely than men older than 51 years of age to have NAFLD/NASH as an indication for LT. These findings suggest that postmenopausal women with and without risk factors for NAFLD/NASH development may benefit from greater surveillance and closer follow-up.
Our study found that postmenopausal women had higher post-LT weight gain and higher LT complications, including acute/chronic rejection, sepsis, CKD, or biliary strictures, as compared to men. These findings indicate the importance of monitoring postmenopausal women for post-LT complications and a potential role for diet education and weight control through appropriate patient counseling. Estrogen is a hormone that can protect against inflammation and fibrosis by affecting both Kupffer cells and proinflammatory cytokines, and therefore the decreased levels of estrogen seen in postmenopausal women have been associated with higher levels of liver fibrosis [23]. Because estrogen works as a vasodilator and promotes angiogenesis, the decrease of estrogen following menopause could have vascular effects leading to decreased arterial compliance. The aforementioned functions of estrogen and its lower serum levels following menopause may play a role in the observed increase of LT complications in postmenopausal women, yet there is minimal literature that proposes a sex or hormonal associated mechanism. More studies are needed to elicit the pathophysiology occurring in postmenopausal women following liver transplantation which leads to higher levels of complications and adverse events. Identifying high-risk populations such as postmenopausal women for post-LT complications is crucial to reduce long-term morbidity and mortality. Future studies in larger populations stratified by the etiology of the disease process and indication for LT are necessary to further elucidate the role of sex.
Among LT recipients, cardiovascular disease is a leading cause of morbidity and mortality [23]. LT recipients often have coexisting occult metabolic syndrome and, as a result, have an increased risk for worsened cardiovascular risk profile post-LT [24,25]. Likewise, NAFLD/NASH has an overlapping pathogenesis with metabolic syndrome, and the unfavorable metabolic profile associated with NAFLD/NASH also contributes to increased cardiovascular risks [25]. We found no significant differences between sexes in cardiac mortality or ASCVD risk change although men had a higher number of MIs compared to women.
In alignment with existing literature, our findings support the notion that sex and age are important risk factors for LT indication and post-LT morbidity and mortality [26]. The limitations of our study include the demographics of the patient population. In this single center study, most participants identified as White. Since previous population-based studies have identified an increased prevalence of NAFLD/NASH in the Hispanic population, a larger demographic of patients with a more diverse representation of races could accentuate our results and improve generalizability. Given that our selection of postmenopausal women was based primarily on age, there could be some degree of sampling error regarding group definitions. However, because there needed to be a standardized comparison against men and because it is difficult to confirm markers of postmenopausal status consistently (if not otherwise clearly stated) from an EMR retrospective study, this work remains a valuable and worthwhile start to further investigations on this subject.
Given the discussion of increased cardiovascular disease risk in association with decreased levels of estrogen, a notable limitation is not discerning whether patients were on estrogen or hormonal replacement therapy (HRT). Reported prevalence of HRT use in the United States varies widely, as the benefits and risk profile for HRT has changed dramatically over recent years. While some studies have found decreased cardiovascular disease risk with HRT, more recent studies have shown increased neurovascular risk [27,28]. Seeing if HRT influenced the outcomes of this study may provide some new information; however, it is likely that the number of patients taking HRT in our study group is low and would only act as an outlier rather than provide further insight. Additional studies with larger populations are needed to examine the effect of HRT on this demographic. Furthermore, studies that have tried to evaluate the effect of HRT on NAFLD/NASH specifically are limited [29]. There is currently an ongoing clinical trial sponsored by Massachusetts General Hospital with preliminary results expected in 2027 looking into HRT as a therapeutic option for post-menopausal women with NAFLD/NASH, demonstrating the recent interest and importance of this subject [30].
An additional limitation of this study is exclusion bias. Patients with multiple LT indications were excluded from this study. Excluding this subset of patients removed additional patients with NAFLD/NASH, which may have otherwise demonstrated an increased prevalence of NAFLD/NASH among post-menopausal women. Patients taking more than one immunosuppressive medication were also excluded from this study to simplify the analysis and eliminate confounding variables. Including these patients in the final analysis may have modified the results and demonstrated an increased prevalence of NAFLD/NASH among post-menopausal women. Another limitation includes the categorization of LT indications among men. Although NASH was not a common LT indication among men (12.5%) as compared to women (26.5%), cryptogenic cirrhosis was the third most common LT indication among men (19.3%). Cryptogenic cirrhosis represents cirrhosis of unknown etiology, but research suggests NASH may play a role in its pathogenesis and development [31]. As such, NASH as a LT indication among men may be underrepresented in this study.
5ConclusionsThere is limited literature that specifically investigates outcomes in postmenopausal women post-LT. This study suggests that postmenopausal women are significantly more likely to have NASH as an indication for LT than men. Postmenopausal women had greater weight gain and more noncardiac complications than men. Despite weight gain with presumably lower estrogen levels postmenopause, women did not have increased cardiovascular outcomes, ASCVD risk, or mortality compared to men. With these noted relationships, diet education and weight control in postmenopausal women with existing risk factors for NASH should be encouraged to modulate health outcomes.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statementNatalia Salinas Parra: Writing – original draft, Writing – review & editing. Michelle Schafer: Writing – original draft, Writing – review & editing. Heather M. Ross: Writing – original draft, Writing – review & editing. John Bruckbauer: Writing – original draft. Brian Yan: Writing – original draft. Sarah L. Chen: Writing – original draft. Adnan Khan: Conceptualization, Methodology, Supervision. Danielle M. Tholey: Supervision, Writing – review & editing. Dina Halegoua-DeMarzio: Supervision, Writing – review & editing.