Recurrent pyogenic cholangitis is endemic to South-east Asia but has been very rarely reported from natives of other parts of the world. A 43-years-old woman was presented with sepsis that had a history of recurrent epigastric pain and fever attacks. Her liver tests were unremarkable suggesting any hepatobiliary diseases. Recurrent pyogenic cholangitis and congenital extrahepatic biliary anomaly have been diagnosed after serial diagnostic and therapeutic procedures including endoscopic retrograde cholangiography, MR-cholangiography, percutaneous transhepatic cholangiography and finally left hepatectomy. She was cured completely following surgical treatment.
Recurrent pyogenic cholangitis (RPC) is characterized by recurrent cholangitis attacks, dilated bile ducts and intrahepatic pigment stones.1 Typically its prevalence is high either in natives or immigrants of South-east Asian population. Sporadic cases have been very rarely reported among natives of other parts of the world.2 Although the mechanism underlying the initiation of biliary sepsis is unknown, parasites including Ascaris lumbricoides and Clonorchis sinensis, enteric microorganisms, and malnutrition are accused as the triggering factors.3 Stone formation is thought to result from the action of bacterial beta-glucuronidase on conjugated bilirubin. Although congenital biliary defects are usually of no clinical importance, occasionally these defects may lead to bile stasis, inflammation and biliary stones. Congenital biliary anomaly and RPC relationship has not been described before. Herein, we have reported for the first time RCP in a patient with congenital biliary anomaly. We have also discussed the diagnostic and therapeutic difficulties of that extremely rare association.
Case ReportA 43-years-old woman admitted with the complaint of fever for three days. Her past medical history revealed intermittent upper abdominal pain and fever for the last 2 years. She had admitted to other medical centers several times with the same complaints and laboratory tests including liver enzymes and bilirubin were detected as unremarkable. At admission, she looked miserable, had fever (40 °C), hypotension (80/50 mmHg) and tachycardia (119/min). There was mild pain on deep epigastric palpation. Laboratory examination showed leukocytosis (23,000/mm3) and thrombocytopenia (52,000/mm3). Other abnormal findings were as follows:
- •
Erythrocyte sedimentation rate: 53 mm/h.
- •
C-reactive protein: 32 (N: 0-0.8).
- •
Blood urea nitrogen: 73 mg/dL.
- •
Serum creatinine: 2.2 mg/dL.
- •
Plasma albumin 3.2 g/dL.
Other blood tests including liver enzymes and bilirubin were all within normal limits. Chest X-ray was normal. Urine analysis was free of bacteria or leukocyte. Abdominal ultrasonography and tomography showed biliary dilatation at the left lobe of liver (Figure 1). Gallbladder and choleduct could not be differentiated due to marked dilated biliary tract. She was hospitalized and empirical intravenous antibiotic (ertapenem 1,000 mg/day) was initiated after taking blood and urine samples for bacterial culture.
Endoscopic retrograde cholangiography (ERC) was performed showing normal choleduct and right intra hepatic biliary tree (Figure 2). Left intrahepatic biliary tree could not be visualized at ERC. Urine and blood cultures were non-diagnostic. Her clinical status and laboratory findings became better gradually and improved completely at the 5th day of hospitalization. Magnetic resonance cholangiopan-creatography (MRCP) demonstrated stone in the gallbladder, prominent dilatation of left biliary tree and stones in the left biliary ductules (Figure 3). Percutaneous cholangiopancreatography was performed showing marked biliary dilatation and numerous intrahepatic stones at the left lobe of the liver (Figure 4). Guide wire could not be passed through the choleduct because of hard stones. Surgery was planned and left hepatectomy was performed.
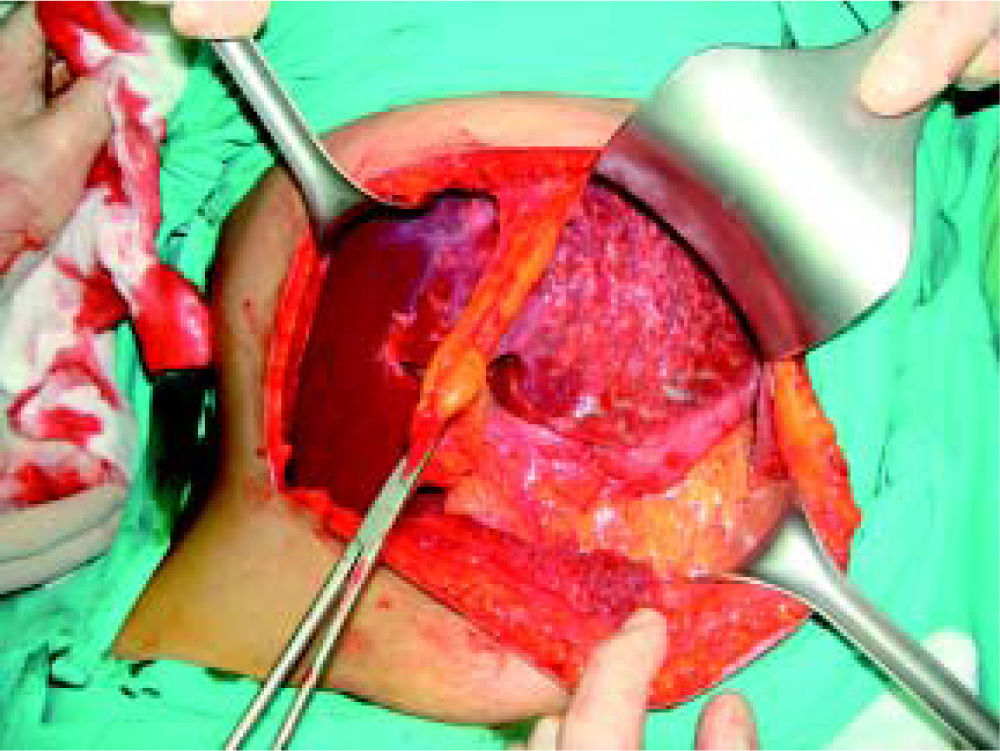
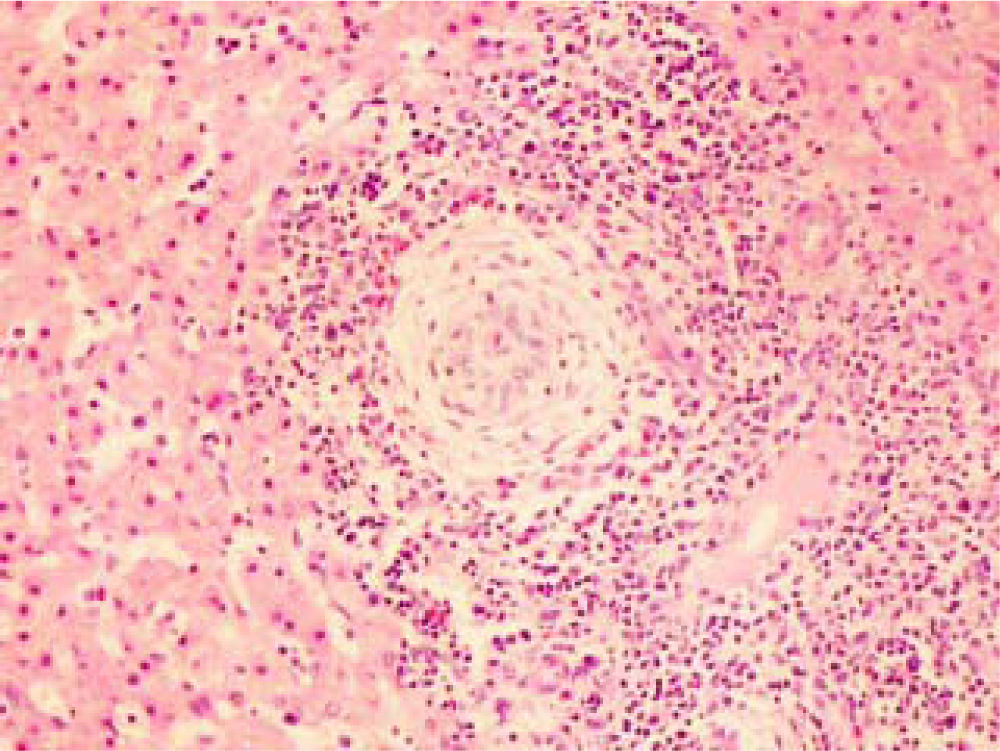
Two hepatic lobes appeared completely different macroscopically (Figure 5). Numerous biliary black pigment stones were present in the resected lobe. Moreover, her left hepatic duct was not connecting with the right hepatic duct, was strictured, and was opening to the duodenum separately. Also left hepatic artery was originated from left gastric rather than common hepatic artery. Histological examination of resected liver revealed dilated biliary ductules containing numerous black stones and secondary sclerosing cholangitis (Figure 6). At the post-operative follow-up she had biliary leakage from the resected side of remaining liver. Nasobiliary draining catheter was inserted into that side and complete resolution was achieved at the 30th day after operation. She was free of symptoms at the 3 months follow-up period.
DiscussionThe present case report is featured for several aspects. First, RPC has been extremely rarely reported in population other than Southeast Asia. Second, congenital extrahepatic anomaly may be a triggering factor for RPC in the present case. Finally, her liver enzymes and serum bilirubin levels remained normal since the beginning of symptoms and even during sepsis.
RCP is a syndrome endemic to South-east Asia. Reports from the other parts are encountered mostly in Asian immigrants and sporadic cases have been reported among natives of other parts of the world.4,5
Right hepatic duct was the major conduit for the right and left lobes of liver. Typically, the left biliary ducts are affected most severely in the course of RPC. The pathogenesis of that left-side predominance is not known. Papilla of the sphincter of Oddi may be hypertrophied and fibrosed. Similarly left hepatic duct and its separate papilla were fibrosed and left hepatic duct was strictured in the present case.
In our case although multiple stones were impacted in whole left lobe of the liver, there was no evidence of cholestatic findings based on the laboratory results. This may be ascribed to the presence of a communicating channel between the two extrahepatic bile ducts that provided another way for biliary excretion. Although MRCP has also played an important role in the diagnosis of double extrahepatic bile ducts, it did not provide detailed anatomical information about the biliary tree due to the multiple impacted stones in the current case.6s
The variations in the morphological characteristics of the extra-hepatic biliary system are rare and different types have been reported either alone or as in combinations in the literature. Complete duplication of the common bile duct occurs rarely.7 The morphological classification of a double extrahepatic bile duct has been modified by Choi, et al.6 Our case corresponded with a type IIIa anomaly according to that classification.
Surgical management was the optimal option in the present case. She had a life-threatening septic attack, had stones within the intrahepatic ducts, and disease predominantly localized to the left hepatic ductal system. Although left hepatic lobectomy was curative, post-operative period was somehow problematic as a result of congenital variations in the present case. Surgery is also mandatory to prevent long-term complications including secondary biliary cirrhosis and cholangiocarcinoma in patients with RPC.8
In conclusion, RCP is a very rare disease in the world other than among cases living in South-east Asia. Recognition of RPC and underlying biliary variation is highly important in therapeutic management.
DisclosuresWe (all authors) declare that there is no conflict of interests among the authors.