Hepatic metastases are common in the clinical course of breast cancer and typically appear as mass lesions. This report describes the case of a 70-year-old woman with a history of breast cancer and no previously known liver disease presenting with the first episode of variceal bleeding and subacute hepatic failure. Imaging studies indicated liver cirrhosis without signs of malignant focal lesions. Comprehensive diagnostic work-up was negative for specific causes of liver disease and provided no evidence for tumor recurrence. Finally transjugular liver biopsy revealed a marked diffuse desmoplastic infiltration by breast cancer cells. Malignant pseudocirrhosis is an unusual pattern of metastatic tumor, spread representing a rare but important differential diagnosis of progressive liver failure. Liver biopsy is the key procedure to establish the diagnosis as imaging studies may mimic cirrhosis.
Complications of portal hypertension and progressive liver failure are the characteristic presentations of advanced liver disease, however malignant pseudocirrhosis has been delineated as an uncommon pattern of metastatic spread of solid tumors and represents a rare but important differential diagnosis.1,2 Determination of the etiology of liver failure is crucial for further clinical management of these patients as orthotopic liver transplantation is contra-indicated in patients with active malignancy.
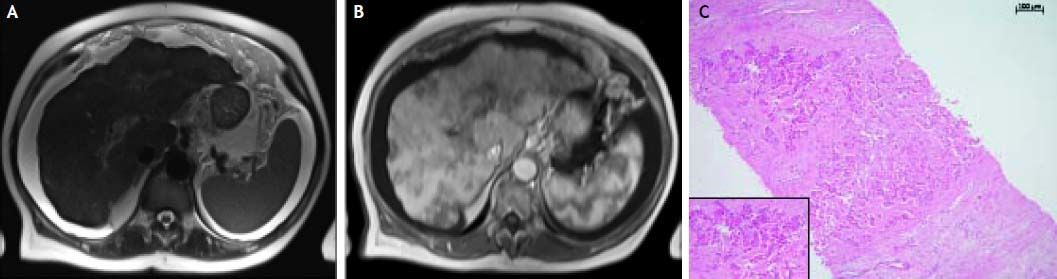
Case ReportA 70-year-old woman with a history of type 2 diabetes mellitus, remote breast cancer and current ibuprofen intake since knee replacement surgery three weeks earlier presented with upper gastrointestinal bleeding and signs of hemorrhagic shock. Emergency endoscopy revealed grade 3 esophageal varices with active bleeding, which was successfully controlled by band ligation. Laboratory work up was significant for: hemoglobin, 5.1 g/dL; platelets, 98,000 cells/mm3; alanine aminotransferase, 97 U/L; γ-glutamyl transpeptidase, 296 U/L; alkaline phosphatase, 138 U/L; total bilirubin, 3.5 mg/dL; international normalized ratio, 1.92; serum albumin, 18 g/L; and lactate dehydrogenase, 1,561 U/L. Comprehensive serology studies provided no evidence for viral, autoimmune, or hereditary liver diseases, and alpha-fetoprotein screening for hepatocellular carcinoma was negative. Liver ultrasound was consistent with macronodular liver cirrhosis with large amounts of ascites, and MRI likewise delineated macronodular liver cirrhosis devoid of focal lesions and portal vein thrombosis (Figure 1). Thus, in absence of chronic alcohol consumption, a provisional diagnosis of subacute presentation of cryptogenic, potentially non-alcoholic steatohepatitis-related cirrhosis was entertained.
Magnetic resonance imaging of the liver and histology of transjugular biopsy. A. The T2-weighted HASTE-Sequence demonstrates massive ascites and a nodular surface of the liver together with a hypertrophy of liver segment 1. B. On the arterial phase T1-weighted image post contrast medium hypovascularized areas throughout the whole liver are noticed, indicating areas of focal fibrosis. C. Highly distorted liver architecture with extensive fibrosis and diffuse infiltration by small clusters of medium sized tumor cells (H&E, x100).
However, though no variceal re-bleeding occurred, the clinical course and liver function continued to relentlessly deteriorate with repeated requirement for paracentesis and relapsing episodes of grade 3 hepatic encephalopathy. A detailed chart review indicated left-sided (ductal type: pT2pN1b, G2) and right-sided breast cancer (lobular type: pT1N0, G2) 17 and 7 years ago, respectively, for which mastectomies with adjuvant chemo- and endocrine therapies had been performed. In conjunction with persistent excessive lactate dehydrogenase elevation, the patient underwent an oncologic re-assessment including gynaecologic examination, imaging studies of chest, abdomen and brain as well as bone scintigraphy without evidence of tumor recurrence. Cytopathologic examination of ascites fluid did not reveal malignant cells. Given the clinical picture of a subacute liver failure, we performed transjugular liver biopsy. Liver histology was consistent with marked desmoplastic infiltration by breast cancer (Figure 1). Since palliative chemotherapy was precluded by marginal liver function with quickly rising bilirubin levels up to 15 mg/dL, the patient opted for home hospice and succumbed one month later.
DiscussionPseudocirrhotic presentations have been appreciated as an uncommon pattern of metastatic spread of invasive breast cancer and other malignancies including, among others, non-Hodgkin lymphoma and small cell lung cancer.1,2 While the pathoanatomy recapitulates cirrhosis, as reflected by the alternative designation “pseudocirrhosis” or “metastatic carcinomatous cirrhosis”, a profound peritumoral desmoplastic reaction has been reported to be mounted by diffuse neoplastic cell infiltration, which is potentially related to an altered expression pattern of cell adhesion molecules.3,4 Pressure atrophy or vascular occlusion by tumor cells might lead to ischemic necrosis of hepatocytes and subsequently to acute liver failure.3
Clinical presentation of pseudocirrhosis is by complications of portal hypertension and/or by progressive liver failure. Radiologic studies may fail to depict carcinomatous infiltration as CT and MR imaging typically mimicks cirrhosis.1 Since in most reports diagnosis was established post-mortem, the critical issue of isolated malignant pseudocirrhosis as a potential, though uncommon, presentation of active malignancy has important implications for liver transplantation. Indeed, despite its clinical relevance, no consensus has been reached as to the management of patients with a history of extrahepatic cancer with respect to specific time requirements of relapse-free survival and overall tumor- and stage-specific prognosis.5 Specifically, breast cancer is notorious for a high propensity for late recurrence.6 Furthermore, the relative diagnostic yield of liver biopsy to confirm or exclude microscopic tumor infiltration has not been studied systemically in this specific subset of potential transplant candidates.
However, in this case, transjugular liver biopsy was instrumental in pinpointing the elusive differential diagnosis of metastatic breast cancer recurrence confined to the liver. With respect to the important question as to how to select patients for pre-transplant liver biopsy in such a scenario, disproportionate lactate dehydrogenase elevation and lactate dehydrogenase:alanine aminotransferase ratio in comparison to non-malignant causes have been reported and might provide helpful clues for patient assessment.7
Financial DisclosureAll authors disclose no financial relationships relevant to this manuscript.