Hepatopulmonary syndrome (HPS) is a complication of portal hypertension (PH) defined by the presence of liver disease, abnormal pulmonary gas exchange and evidence of intrapulmonary vascular dilatations (IPVD) producing a right to left intrapulmonary shunt. Liver transplantation (LT) is the treatment of choice; however, severe hypoxemia may contraindi-cate LT. The use of transjugular intrahepatic porto-systemic shunts (TIPS) could be effective in HPS, although available data is limited. Aim: To report a clinical case of severe HPS treated sequentially with TIPS and LT. Case report: A 46 year old female cir-rhotic patient presented with rapidly progressive dyspnea, hypoxemia (PaO2 60 mmHg, SaO2 92%) and increased alveolar-arterial oxygen gradient (A-a) (46 mmHg). She also had orthodeoxia (SaO2 87% in sitting position, but 91% in a prone position). A CT scan and pulmonary angiography were normal. Spirometric assessment showed a mild restrictive pattern and a desaturation was observed in a six-minute walking test. Contrast-enhanced echocardiography (CEE) showed intrapulmonary shunting. A HPS was diagnosed and liver transplantation was disregarded due to severe hypoxemia. The patient underwent TIPS placement. After four weeks, a significant improvement of dyspnea and a complete remission of orthodeoxia were seen. One year later, the patient was successfully transplanted. Interestingly, six months after LT, and in the absence of dyspnea, a new CEE showed persistent passing of bubbles to the left cavities. Comments/Conclusion: Persistent right-to-left shunt after TIPS placement and liver transplantation in spite of the improvement of pulmonary function tests suggests long-term persistence of structural changes in the pulmonary vascular tree after liver transplantation. Because of lack of data, it is not possible to recommend the routine use of TIPS as a part of the conventional management of HPS. However, in patients with severe hypoxemia TIPS placement can reasonably be used as a bridge towards transplantation.
Hepatopulmonary syndrome (HPS) is a complication of portal hypertension that is present among up to 15-20% of cirrhotic patients.1,3 The currently accepted diagnostic criteria for HPS are: i) presence of portal hypertension or liver failure, ii) decrease of arterial PO2 (defined as PaO2 < 70 mmHg, or an increased alveolar-arterial oxygen gradient corrected by the age of the patient), iii) presence of intrapulmonary vascular dilatations (IPVD) that produce intrapulmonary shunt.1 The hallmark of HPS is the presence of IPVD, probably secondary to portal hypertension and producing a right to left intrapulmonary shunt.4 Currently, liver transplantation is considered the treatment of choice for HPS. However, because of severe hypoxemia, the procedure is contraindicated in many cases. We describe the case of a woman with cirrhosis and HPS who showed an impressive improvement after TIPS placement which allowed for a successful orthotopic liver transplantation.
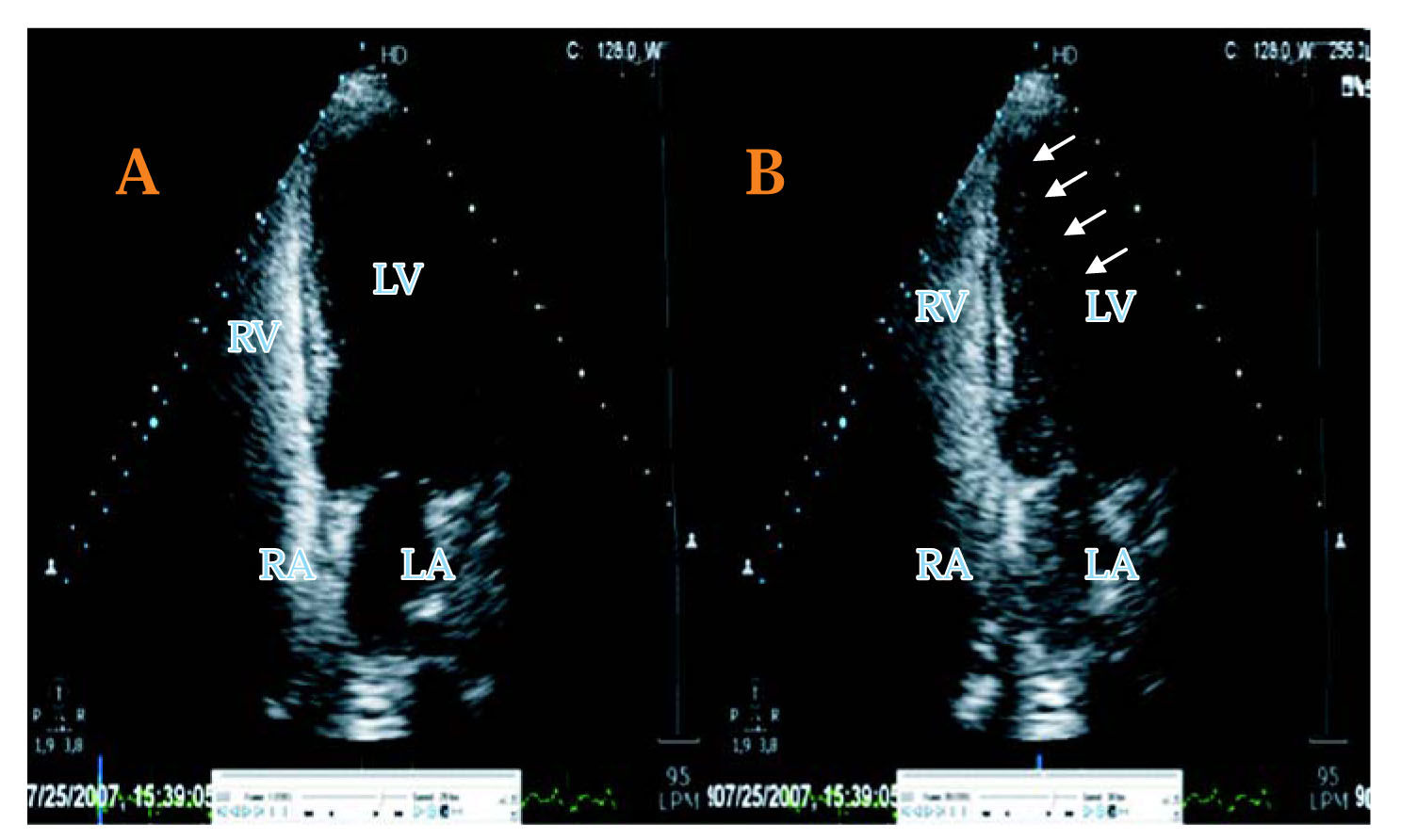
Case reportWe present a 46 year old female patient with cryptogenic cirrhosis that developed ascites, which was well controlled with diuretics and sodium restriction. Four years after the diagnosis, she developed progressive dyspnea over several months, until functional capacity III (shortness of breath when dressing). At that point, a biochemical evaluation was performed showing the following laboratory results: Hematocrit 41%, hemoglobin 8.7 mg%, leucocytes 3,200/uL, platelets 64,000/uL, serum levels of bilirubin 3.7 mg%, albumin 3.2 g%, aspartate aminotransferase 48 UI/L, alanine aminotransferase 29 UI/L, alkaline phosphatase 195 UI/L, gamma-glutamyl-transpeptidase 39 UI/L, and creatinine 1.05 mg%. The International normalized ratio (INR) International Normalized Ratio of prothrombin time was 1.4 and the serum levels of sodium and potassium were normal. She was classified as Child Pugh B (7 points) and had a MELD score of 13 points. Arterial gases were measured: PaO2 60 mmHg, PaCO2 27 mmHg, SaO2 92% and alveolar-arterial oxygen gradient (A-a) 46 mmHg (normal value for her age 12 mmHg). Pulse oxymetry was 87% in a sitting position, but 91% in a prone position, a finding consistent with orthodeoxya. A thoracic CT scan was normal and a spirometric study of liver volumes showed a mild restrictive disease. Additionally, a very important desat-uration was observed in a six minutes in the walking test. A microbubble contrast-enhanced echocardiogram (CEE) was performed and showed a late pass of bubbles to the left cavities of the heart, which is compatible with an intrapulmonary shunt (Figure 1). A pulmonary angiography was also normal.
Transthoracic echocardiography study, 4 chamber view, showing right heart opacification with contrast saline bubbles (A), and the presence of contrast in the left heart (B, arrows) evident > 5 cardiac cycles of right heart opacification, compatible with the presence of a pulmonary arteriovenous shunt.
Considering the above mentioned data, the diagnosis of HPS was made, and liver transplantation was discussed. However, the severe hypoxemia was considered a contra-indication of the procedure. Because of this, a TIPS placement was considered as a bridge towards liver transplantation. The TIPS was placed uneventfully. In the next 4 weeks the patient showed a significant improvement of dyspnea and a complete loss of orthodeoxya. At that point, she had a PaO2 of 72 mmHg and a normal functional capacity. Six months later she once again presented a moderate shortness of breath. An abdominal Doppler ultrasonography test showed a 50% stenosis of the TIPS. Its dilatation was followed by a complete improvement of the symptoms. In spite of the absence of shortness of breath, a new mi-crobubble contrast echocardiography showed persistent passing of bubbles to the left cavities. The patient was successfully transplanted almost one year after the installation of the TIPS. Interestingly, six months after the liver transplantation, and in the absence of dyspnea, a new CEE was made and showed an important passing of bubbles to the left cavities.
DiscussionHPS was described for the first time by Kennedy and Knudson in 1977.5 In spite of the important advances in the knowledge of its etiopathogenic diagnosis and treatment, it is still an important challenge for hepatologists.
The diagnostic procedures currently used to establish the presence of HPS are microbubble contrast echocardiography and technetium-labeled macroaggregated albumin scan (MAA scan). The contrast echocar-diography is considered diagnostic if the bubbles are seen in the left heart cavities at least three beats after their visualization in the right cavities, to rule out an intracardiac shunt.6 On the other hand, the MAA scan is considered positive if there is accumulation of the labeled albumin in extrapulmonary organs, because normally the macroaggregates should be caught by the pulmonary capillaries.6 The diagnosis of HPS was made in our patient using contrast echocardiography. Interestingly she exhibited a very significant improvement in her functional capacity after the TIPS placement, but the contrast echocardiogram was persistently altered even after liver transplantation. This may indicate that test’s utility seems to be limited to the diagnosis of the disease and appears ineffective for the follow-up.
At present, there is no effective medical therapy considered useful in the management of HPS. In fact, the current treatment of choice for HPS is liver transplantation with a mean in the largest single-institution series.7 Since the strongest predictor of death in this series was a preoperative partial pressure of oxygen of 50 mmHg the presence of severe hypoxemia may be considered a contraindication for the transplant procedure.1 In this setting, portal decompression through a TIPS placement could be effective. Although the role of cirrhosis and portal hypertension in the pathogenesis of HPS is controversial since HPS can occur in patients with cirrhosis but no portal hypertension, and in cases with portal hypertension but no liver damage,8 portal hypertension is frequently associated to HPS and TIPS could be beneficial. However, experience in this regard is scarce and contradictory.9–15 In six of the published cases, an improvement of pulmonary function was observed, but problems such as a short follow up or the presence of hepatic hydrothorax secondary to portal hypertension make interpretation of the results very difficult. On the other hand, Martinez et al. evaluated the utility of TIPS in three patients with advanced HPS. There were no significant changes of the pulmonary function of these patients and they concluded that it is not possible to recommend the use of TIPS for the treatment of HPS.12
Our patient was not considered a good transplant candidate due to her functional capacity and therefore TIPS placement was proposed as a bridge to liver transplantation. Her symptoms and pulmonary tests showed an amazing improvement after the shunt installation that allowed for a successful liver transplantation afterwards. Interestingly, the occurrence of TIPS dysfunction was associated to the reappearance of the symptoms and, more impressively, they disappeared after the correction of the shunt stenosis. This allowed us to establish a clear relation between the presence of a functional TIPS and the resolution of the symptoms. It has been suggested that TIPS effectiveness is due to the fact that a reduction of portal pressure induced by TIPS placement increases cardiac output, improving the ventilation-perfusion matching as a result of a selective redistribution of the blood flow to the upper lobes of the lung where the vasodilatation is typically less severe in HPS.12
As in a previous report,16 the diagnostic studies for HPS (in our case CEE) were persistently positive after TIPS placement, in spite of the improvement of pulmonary function. This suggests that, in successfully treated cases, the intrapulmonary shunt is not completely eliminated, but reduced enough to improve pulmonary function. Along this line, Martínez-Palli has recently reported that in patients with HPS, single-breath diffusing capacity for carbon monoxide remains reduced despite the improvement of the results of pulmonary function tests (ventilation-perfusion mismatch, PaO2, alveolar-arterial oxygen gradient and PCO2) after liver transplanta-tion.17 This can be due to the persistence of structural changes in the pulmonary vascular tree after liver transplantation, such as an increase of the collagen layer of the vessels, which can make the diffusion of the carbon monoxide more difficult.18
In conclusion, based on the available evidence, it is not possible at present time to recommend the use of TIPS as a part of the conventional management of HPS. However, in patients with severe hypoxemia and marked deterioration of functional capacity who cannot undergo a liver transplantation, as the patient presented here, the placement of TIPS can reasonably be used as a bridge towards it.