Intense enhancement of the quadrate lobe in the arterial phase may be seen on computed tomography in patients of superior vena cava syndrome. We present this imaging finding in a case of lymphoma causing superior vena cava syndrome and discuss the physiological cause and importance of this sign.
It is important to recognise the intense arterial enhancement of the quadrate lobe in superior vena cava obstruction to avoid misdiagnosing it as a true lesion.
IntroductionSuperior Vena Cava (SVC) syndrome is usually caused by extrinsic compression due to malignant disease like bronchogenic carcinoma, lymphoma and metastatic lymphnodes; occasionally it may be due to benign causes like aortic aneurysms, chronic/fi-brosing mediastinitis, mediastinal granulomatous disease, retrosternal goiter, intrinsic thrombosis due to prothrombotic disorders and iatrogenic causes including central venous cannulations and transvenous pacemaker.1 It clinically manifests by progressive dilatation of veins and edema of the upper body, cyanosis, CNS disturbances like syncope, headaches and altered consciousness and edema of the trachea and esophagus with respiratory distress. Occasionally SVC syndrome may not be clinically apparent, especially in obese patients with a thick neck. Also, when obstruction is partial and gradual sufficient collateral circulation may develop for the obstruction to be clinically unapparent and in these cases development of collateral circulation can precede signs and symptoms.2 These collateral channels are essential to the diagnosis of SVC syndrome and also give rise to a few signs on imaging which give a clue to the diagnosis of SVC syndrome. We present such a sign, the CT quadrate hot spot sign, in a case of lymphoma with SVC syndrome and discuss the physiological cause and importance of this sign.
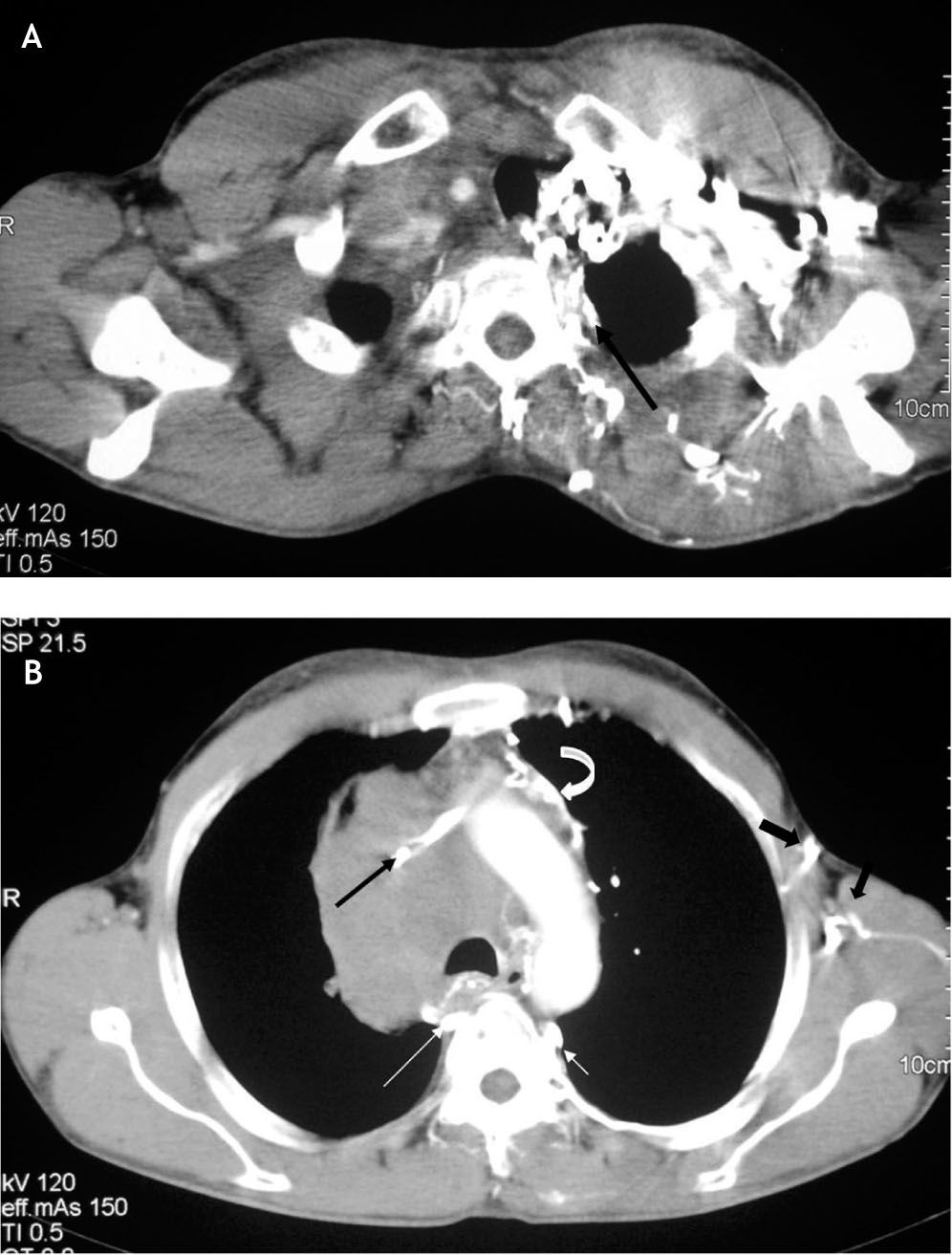
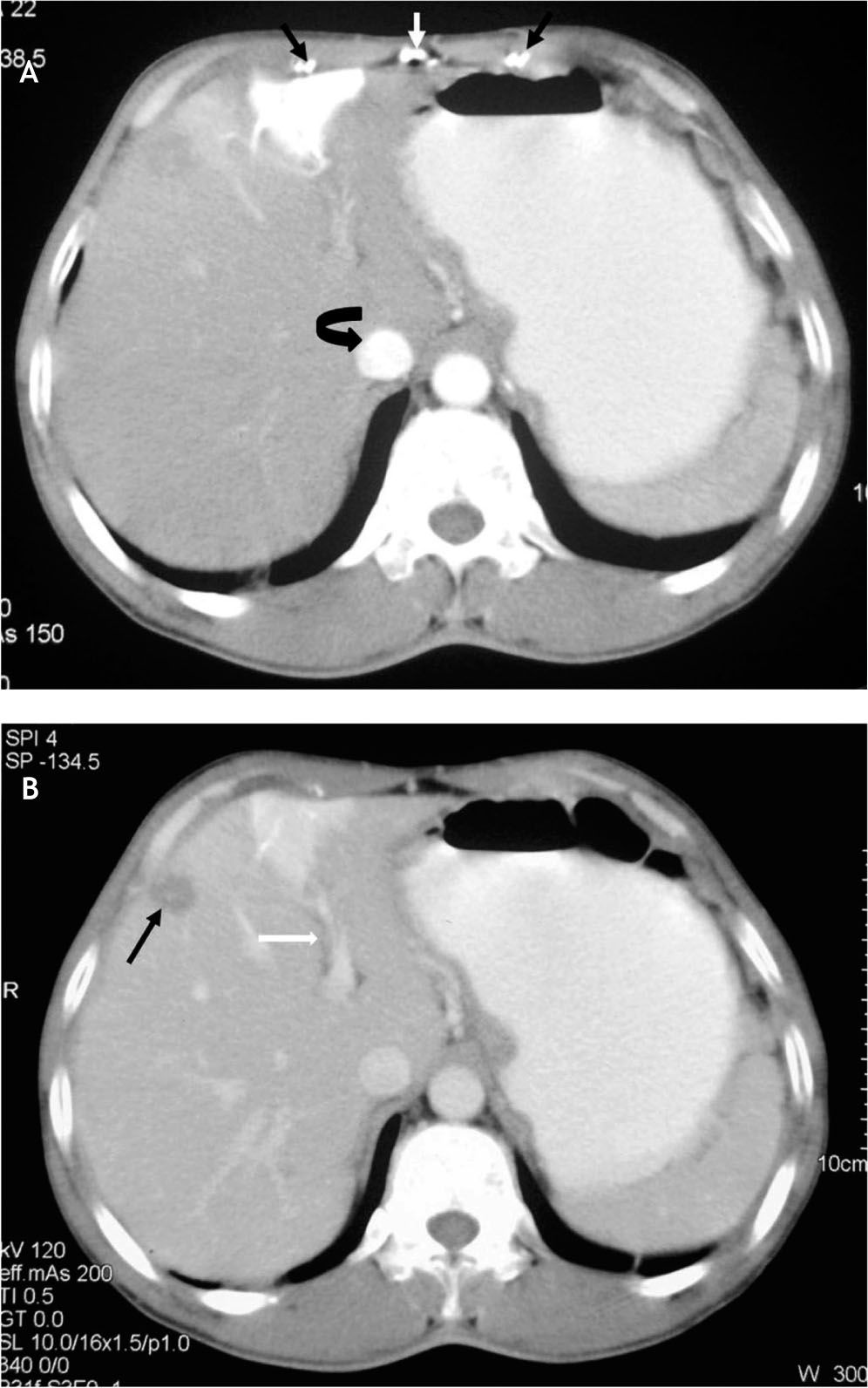
Case HistoryA 43-year-old male patient presented with four month history of fever, malaise and significant weight loss and a two week history of swollen and plethoric face and marked superficial venous distention over his neck and chest suggestive of SVC obstruction. A contrast enhanced biphasic CT of the chest and abdomen was performed, which revealed diffuse homogenous mediastinal lymphadenopathy extending from the level of the superior mediastinum to the left atrium, causing gross compression of the SVC along its entire course and obstruction of the azygous arch as well. Multiple paravertebral, chest and abdominal wall collaterals and dilated azygous-hemiazygous veins were also seen (Figure 1). The lung fields were unremarkable. A diagnosis of SVC syndrome due to lymph nodal compression was established. In addition, there was presence of a geographical area of intense focal enhancement in the medial segment of the left lobe of liver seen on both the arterial and venous phase images (Figure 2). The paired internal mammary veins and the recana-lised umbilical vein were also visualized (Figure 2A). Fine needle aspiration cytology of the mediastinal lymphnodes revealed high grade Non-Hodgkin’s lymphoma and the patient was subsequently referred for chemotherapy.
A. Contrast enhanced CT of the chest, superior section, showing parascapular and superior paravertebral collaterals which carry contrast to the enlarged left superior intercostal vein (arrow) via the intercostal and paravertebral veins. B. Caudal section at the level of aortic arch shows enlarged homogenous lymphnodes causing compression of the SVC (black arrow) and the azygous arch. Dilated azygous (long white arrow) and hemiazygous veins (short white arrow), along with aorto-pulmonary window (curved arrow) and left lateral chest wall collaterals (arrowheads) are seen.
A. Contrast enhanced CT of abdomen, arterial phase, shows a wedge shaped area of intense focal enhancement (slightly more than aorta) in segment IV of liver that represents CT equivalent of hepatic hot spot sign on nuclear scan. The paired mammary veins are dilated (black arrows) and note is also made of recanalised umbilical vein (white arrow). There is early enhancement of the IVC as well (curved arrow). B. Portal venous phase showing partial washout but persistence of the focal enhancement of the medial segment of left lobe of liver, which is in close proximity to the left branch of the portal vein (white arrow). Note is made of a simple liver cyst in segment VIII of liver (black arrow).
The diagnosis of SVC syndrome on CT requires the presence of two imaging findings:
- •
Decreased or absent opacification of central venous structures distal to the site of obstruction, usually associated with a visible obstructing lesion or intraluminal filling defect.
- •
The opacification of collateral venous channels.3
Four main collateral pathways carry venous blood around an obstruction and back to the right side of the heart: The azygous hemiazygous route, internal mammary vein, lateral thoracic and superficial thoracoabdominal veins and the vertebral venous plexus.4 SVC syndrome was venographically classified by Stanford into four types:
- •
Type I and type II referred to supra-azygous obstruction with < 90% and > 90% obstruction of the SVC respectively.
- •
Type III obstruction is infra-azygous complete or near complete obstruction of the SVC with reversal of azygous blood flow. Maximum collaterals and most severe symptoms develop in this kind of obstruction.
- •
In Type IV obstruction (as in the index case) there is complete obstruction of the SVC and one or more of major caval tributaries, including the azygous system.5
Different collateral venous channels may get opa-cified depending on the type of obstruction. In cases of supra-azygous SVC obstruction (type I and II) there is antegrade flow with hyperdense opacifica-tion of the azygous hemiazygous system, along with the superior intercostal veins and the superior para-vertebral and intercostals collaterals. In infra-azygous SVC obstruction (type III) there is retrograde flow with opacification of the entire azygous-hemiazygous system, inferior paravertebral and lumbar veins, hepatic veins and musculophrenic collaterals towards the IVC and right atrium. When concomitant SVC and azygous venous system block occurs (type IV) the anterolateral collaterals, which include the internal mammary veins, and lateral thoracic and superficial thoracoabdominal veins are opacified.4,5 These systemic veins may communicate with the umbilical and paraumbilical veins through the musculophrenic and superficial epigastric veins.3,6
The umbilical and paraumbilical veins preferentially drain into the left branch of the portal vein and these results in a systemic-portal shunt, causing increased blood flow in the arterial phase in the part of the liver supplied by the left branch of the portal vein. This systemic portal shunting, along with the preferential drainage of the umbilical and paraumbilical veins into the left branch of the portal vein forms the physiological basis of the “focal hepatic hot spot” in the quadrate lobe (functionally a part of the left lobe of liver, lies between the gall bladder fossa and fissure for ligamentum teres and designated segment IV in the Bismuth-Couinaud classification of liver segments) observed on 99 m (99 mTc) sulphur colloid scan.3,7 The CT counterpart of this sign was first described by Ishikawa in 1983 and it manifests as an area of intense focal enhancement of the quadrate lobe in the arterial phase with opacification equal to or more than the aorta.7 This area of enhancement partially washes out and is slightly hyperdense or isodense in the venous phase. Some other causes of hepatic hot spots include Budd-Chiari syndrome, hemangioma, focal nodular hyperplasia and hepatocellular carcinoma.3 However, the characteristic location, the wedge shape, arterial and venous phase characteristics and associated findings of collateral vessels make this lesion highly specific as an indicator of SVC syndrome. Another finding observed in the index case was early enhancement of the IVC in the arterial phase, which has been described in SVC syndrome, due to collateral vessel formation between the systemic and pulmonary venous circulation which allows the alveolar spaces and right heart to be bypassed.8
In conclusion, the CT counterpart of the quadrate lobe hot spot sign (on technetium sulphur colloid scans) helps to provide a clue to the diagnosis of thoracic central venous obstruction, especially where enhanced CT of the abdomen is performed in patients with clinically unapparent obstruction of the SVC and is highly specific for the diagnosis of SVC obstruction.