Recurrent cirrhosis complicates 10-30% of Liver transplants (LT) and can lead to consideration for re-transplantation. We evaluated the trajectories of relisted versus primary listed patients on the waitlist using a competing risk framework.
Materials and MethodsWe retrospectively examined 1,912 patients listed for LT at our centre between from 2012 to 2020. Cox proportional hazard models were used to assess overall survival (OS) by listing type and competing risk analysis Fine-Gray models were used to assess cumulative incidence of transplant by listing type.
Results1,731 patients were included (104 relisted). 44.2% of relisted patients received exception points vs. 19.8% of primary listed patients (p<0.001). Patients relisted without exceptions, representing those with graft cirrhosis, had the worst OS (HR: 4.17, 95%CI 2.63 – 6.67, p=<0.0001) and lowest instantaneous rate of transplant (HR: 0.56, 95%CI 0.38 – 0.83, p=0.006) than primary listed with exception points. On multivariate analysis listing type, height, bilirubin and INR were associated with cumulative incidence of transplant, while listing type, bilirubin, INR, sodium, creatinine were associated with OS. Within relisted patients, there was a trend towards higher mortality (HR: 1.79, 95%CI 0.91 – 3.52, p=0.08) and low transplant incidence (HR: 0.51, 95%CI 0.22 – 1.15, p=0.07) for graft cirrhosis vs other relisting indications.
ConclusionsPatients relisted for LT are carefully curated and comprise a minority of the waitlist population. Despite their younger age, they have worse liver/kidney function, poor waitlist survival, and decreased transplant incidence suggesting the need for early relisting, while considering standardized exception points.
Liver transplantation is the gold standard treatment for end-stage liver disease. However, cirrhosis recurs in 10-30% of cases [1], while allograft failure can occur in 2.7-6.9% of the grafts [2], requiring relisting for transplantation. There exists a growing discrepancy between the number of available donor organs and the number of potential organ recipients which has caused a noticeable increase in the waiting time as well as the number of deaths while on the waiting list [3]. Patients undergoing re-transplantation (re-LT) are at a higher risk of mortality or complications than those undergoing primary transplant [4].
Under the present allocation system for liver transplantation, primary and re-transplantation are treated the same. MELD scores at the time of initial listing of primary transplantation have been shown to accurately predict mortality on the waiting list. However, data on whether waitlist outcomes differ between primary and relisted transplant candidates have not been examined in detail [5,6]. It has been reported vastly that re-LT candidates tend to be sicker, but their MELD score is not reflective of the extent of decompensation [6,7]. The accuracy of the MELD scores in predicting mortality in patients awaiting liver transplantation has been shown to be correlated to pre-transplant mortality for both those awaiting primary transplant and retransplant with a greater concordance for primary listing [6,8]. Exception points may be used for patients whose MELD scores are unreflective of disease severity [9,10]. However, factors predicting poor outcomes as well as the efficacy of exception points have not been elucidated in full detail [8].
The objective of this study is to compare the outcomes of primary and re-transplant patients on the waiting list and to elucidate the factors that may reveal poor outcomes (death and drop-out) for re-listed candidates. Whether exception points can bridge the gap incurred with the underrepresentation of MELD scores for re-LT has not been examined in detail. Therefore, we also aimed to examine whether the allotment of exception points can ameliorate any underrepresentation of disease severity for relisted candidates to bolster the outcomes through the comparison of primary vs. retransplant cases with and without exception points.
2Materials and Methods2.1Study designThis was a retrospective cohort study consisting of 1,912 adult patients listed at University Health Network, Toronto between November 12th, 2012, and December 31st, 2020. We excluded patients listed for multi-organ transplant, 3rd liver transplant, urgent retransplant, and those delisted due to clinical improvement. The start date was chosen, as this is when the MELD-Na system was adapted for listing in the province of Ontario. All patients were followed from the time of listing to LT or dropout or until June 30, 2021.
2.2Patient characteristicsDemographic and clinical characteristics at the time of listing, including age, sex, body mass index (BMI), blood group, liver disease etiology, decompensation of liver disease such as portosystemic encephalopathy, ascites, variceal bleeding, hepatorenal syndrome (HRS) and spontaneous bacterial peritonitis (SBP), comorbidities including type 2 diabetes mellitus, hypertension, ischemic heart disease (IHD) and chronic kidney disease (CKD) were documented. Functional capacity was categorized from 1 to 9 using the Clinical Frailty Scale (CFS). Patients were divided into four groups:
- 1)
Primary listing with exception points,
- 2)
Primary listing without exception points,
- 3)
Relisting with exception points, and
- 4)
Relisting without exception points.
Exception points in Ontario are provided per standard indications i.e. hepatocellular carcinoma, hepatopulmonary syndrome, primary sclerosing cholangitis with recurrent episodes of cholangitis, and post-transplant ischemic cholangiopathy. While immediate post LT complications requiring urgent retransplant such as hepatic artery thrombosis and primary non-function of the graft are listed as category 4F and were excluded from the study.
2.3Statistical methodsDescriptive statistics were provided for patient characteristics, clinical measurements and events on the waitlist. Means (standard deviations) or medians (range) were calculated for continuous variables and group differences were compared using two-sample t-tests or Wilcoxon tests, depending on the distribution of data. Counts and proportions were provided for categorical variables, and the differences between groups were compared using Chi-squared tests or Fisher's exact tests. In addition, Kaplan-Meier curves were plotted for overall survival, stratified by listing type (primary listing vs. relisting) and exception point (with and without), with group differences compared using log-rank tests. Cumulative incidence curves of transplant were plotted, stratified by listing type and exception, where group differences were assessed using Gray K-sample test.
Univariate and multivariate Cox proportional hazard models were performed to examine the association between variables and overall survival. Univariate and multivariate Fine-Gray models were carried out to investigate the association between risk factors and cumulative incidence of transplant. For both multivariate models, the “listing type stratified by exception point” was included as the primary risk factor, whereas height, bilirubin, INR, sodium, and creatinine at listing were adjusted as covariates due to their clinical importance.
We further assessed the waitlist survival and cumulative incidence of transplant for primary transplant and retransplant by dividing patients into groups according to MELD-Na score <20, 20-24, 25-29, and 30 or more. Lastly, subgroup analyses for relisted patients were performed for comparisons between graft cirrhosis and biliary/vascular causes of relisting. A p value lower than 0.05 was considered statistically significant. All statistical analyses were carried out using SAS 9.4 software (Cary, NC, USA).
2.4Ethical statementWritten informed consent was exempted given the retrospective chart review and the study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a priori approval by the Research Ethics Board of the UHN (REB ID 20-5302).
3Results3.1Patient characteristics1731 patients met inclusion criteria, of which 104 were relisted. Most patients were male (64.8%). The most common etiology of liver disease for the first LT (primary listed patients) was viral hepatitis (29.4%) followed by alcohol (23.2%), nonalcoholic steatohepatitis (NASH) (19.3%) and cholestatic liver diseases (14.6%). The most common reasons for relisting were graft cirrhosis (21.6%) and vascular problems (21.6%).
3.2Comparison of primary listed candidates to relisted candidatesPatients relisted for transplant were significantly younger at listing (mean age 49.93±13.7 vs. 56.57±10.32 years, p<0.001), had lower BMI (median 24.3 vs. 27.1 kg/m2, p<0.001) and less proportion of frail patients (8.7% vs. 29.3%, p=0.031) than primary listed candidates. However, they had more frequent episodes of bacteremia/sepsis (8.65% vs. 1.29%, p<0.001) and ICU stay (33.65% vs. 11.19%, p<0.001) in the last 90 days before end of listing.
All liver disease-related decompensations (encephalopathy, ascites SBP, HRS, and variceal bleeding) were significantly less prevalent in relisted candidates; however, their median bilirubin, INR and creatinine were significantly higher at end of listing (Table 1). Exception points were more frequently awarded to relisted candidates (44.2% vs. 19.8%, p<0.001). Despite that, relisted candidates were transplanted less frequently (49% vs. 61%, p=0.002) with high waitlist mortality (28.8% vs. 18.5%).
Baseline characteristics of all patients stratified between exception status and listing type.
| Listing Type | P value | ||||||
|---|---|---|---|---|---|---|---|
| Totaln = 1731 | Primary listingn = 1627 | Relistingn = 104 | |||||
| Age at list (Years) | Mean (SD) | 56.17 (10.66) | 56.57 (10.32) | 49.93 (13.70) | <0.001 | ||
| Age at end of list (Years) | Mean (SD) | 56.77 (10.68) | 57.16 (10.33) | 50.77 (13.85) | <0.001 | ||
| Sex (Male) | n (%) | 1122 (64.82%) | 1052 (64.66%) | 70 (67.31%) | 0.58 | ||
| Primary etiology | Alcohol | n (%) | 401 (23.19%) | 388 (23.88%) | 13 (12.50%) | ||
| Autoimmune | 66 (3.82%) | 57 (3.51%) | 9 (8.65%) | ||||
| Cholestatic | 252 (14.57%) | 220 (13.54%) | 32 (30.77%) | ||||
| Cryptogenic | 53 (3.07%) | 49 (3.02%) | 4 (3.85%) | ||||
| Metabolic | 43 (2.49%) | 37 (2.28%) | 6 (5.77%) | ||||
| NASH | 333 (19.26%) | 325 (20.00%) | 8 (7.69%) | ||||
| Viral | 509 (29.4%) | 480 (29.54%) | 29 (27.88%) | ||||
| Others | 74 (4.27%) | 69 (4.36%) | 3 (2.88%) | ||||
| Hepatocellular carcinoma | n (%) | 552 (31.89%) | 535 (32.88%) | 17 (16.35%) | <0.001 | ||
| Height at list (cm) | Mean (SD) | 169.65 (9.66) | 169.69 (9.72) | 169.13 (8.78) | 0.57 | ||
| Weight at listing (kg) | Mean (SD) | 80.06 (19.33) | 80.58 (19.31) | 72.40 (18.03) | <0.001 | ||
| Weight at end of listing (kg) | Mean (SD) | 78.20 (19.19) | 78.61 (19.22) | 71.73 (17.47) | <0.001 | ||
| BMI at listing (Kg/m2) | Mean (SD) | 27.08 (5.91) | 27.89 (5.87) | 25.21 (5.69) | <0.001 | ||
| BMI at end of listing (Kg/m2) | Mean (SD) | 27.08 (5.91) | 27.22 (5.90) | 24.90 (5.59) | <0.001 | ||
| ICU stay in last 90 days | n (%) | 217 (12.54%) | 182 (11.19%) | 35 (33.65%) | <0.001 | ||
| Bacteremia/ sepsis last 90 days | n (%) | 30 (1.73%) | 21 (1.29%) | 9 (8.65%) | <0.001 | ||
| Smoking | n (%) | 474 (27.4%) | 448 (27.54%) | 26 (25%) | 0.57 | ||
| Alcohol | n (%) | 612 (35.4%) | 591 (36.32%) | 21 (20.19%) | <0.001 | ||
| Comorbids | Hypertension | n (%) | 337 (19.5%) | 322 (25.10%) | 15 (14.42%) | 0.015 | |
| Diabetes | n (%) | 364 (21%) | 342 (26.66%) | 22 (21.15%) | 0.22 | ||
| Hyperlipidemia | n (%) | 108 (6.2%) | 108 (8.42%) | 00 (00%) | 0.002 | ||
| IHD | n (%) | 71 (4.1%) | 69 (5.38%) | 2 (1.92%) | 0.12 | ||
| CKD | n (%) | 55 (3.2%) | 48 (3.74%) | 7 (6.73%) | 0.18 | ||
| Decompensations | PSE | n (%) | 705 (50.83%) | 682 (53.16%) | 23 (22.12%) | <0.001 | |
| Ascites | n (%) | 948 (68.30%) | 903 (70.33%) | 45 (43.27%) | <0.001 | ||
| LVPs | n (%) | 505 (37.52%) | 489 (38.35%) | 16 (22.54%) | 0.007 | ||
| SBP | n (%) | 189 (13.65%) | 182 (14.21%) | 7 (6.73%) | 0.033 | ||
| Variceal Bleed | n (%) | 476 (34.34%) | 463 (36.12%) | 13 (12.50%) | <0.001 | ||
| HRS | n (%) | 211 (15.21%) | 208 (16.21%) | 3 (2.88%) | <0.001 | ||
| Frail at listing | n (%) | 228 (28.72%) | 226 (29.31%) | 2 (8.70%) | 0.031 | ||
| Bilirubin at listing (µmol/L) | Median (range) | 40 (3 – 1414.) | 39.0 (3 – 1414) | 54.0 (3 – 946) | 0.004 | ||
| Bilirubin at end of listing (µmol/L) | Median (range) | 40 (3 – 1414) | 19 (2 – 1011) | 36 (3 – 816) | <0.001 | ||
| INR at listing | Median (range) | 1.3 (0.8 – 10) | 1.3 (0.8 – 10) | 1.3 (0.9 – 5.2) | 0.11 | ||
| INR at end of listing | Median (range) | 1.1 (0.8 – 10) | 1.1 (0.8 – 10) | 1.1 (0.9 – 10) | 0.017 | ||
| Sodium at listing (mmol/L) | Median (range) | 137 (117 – 153) | 137 (117 – 153) | 137 (127 – 151) | 0.12 | ||
| Sodium at end of listing (mmol/L) | Median (range) | 138 (119 – 160) | 138 (119 – 158) | 138 (121 – 160) | 0.43 | ||
| Creatinine at listing (µmol/L) | Median (range) | 80 (20 – 1376) | 79 (20 – 1376) | 119 (20 – 495) | <0.001 | ||
| Creatinine at end of listing (µmol/L) | Median (range) | 91 (20 – 794) | 91 (20 – 794) | 124.5 (20 – 748) | <0.001 | ||
| MELD-Na at listing | Median (range) | 19 (6 – 55) | 19 (6 – 55) | 19 (6 – 49) | 0.14 | ||
| MELD-Na at end of listing | Median (range) | 19 (6 – 57) | 19 (6 – 57) | 16 (6 – 49) | 0.43 | ||
| MELD-Na at primary listing(For relisted patients only) | Median (range) | NA (NA – NA) | NA (NA – NA) | 21.5 (6.0 – 42.0) | |||
| MELD-Na at end of primary listing(For relisted patients only) | Median (range) | NA (NA – NA) | NA (NA – NA) | 23.5 (7.0 – 39.0) | |||
| Reason of relisting | Vascular problems | n (%) | NA (NA – NA) | NA (NA – NA) | 21 (20.19%) | ||
| RecurrentPrimary disease | NA (NA – NA) | NA (NA – NA) | 21 (20.19%) | ||||
| Rejection/Immune mediated | NA (NA – NA) | NA (NA – NA) | 14 (13.46%) | ||||
| Biliary | NA (NA – NA) | NA (NA – NA) | 20 (19.23%) | ||||
| Exception points | n (%) | 369 (21.32%) | 323 (19.85%) | 46 (44.23%) | <0.001 | ||
| Time on waitlist (Days) | Median (range) | 161 (0 – 2360) | 159 (0 – 2360) | 188.5 (0 – 1772.0) | 0.16 | ||
| Outcome of listing | Active listing | n (%) | 184 (10.63%) | 166 (10.20%) | 18 (17.31%) | 0.002 | |
| De-listed | n (%) | 173 (9.99%) | 168 (10.33%) | 05 (4.81%) | |||
| Died | n (%) | 331 (19.12%) | 301 (18.50%) | 30 (28.85%) | |||
| Transplanted | n (%) | 1043 (60.25%) | 992 (60.97%) | 51 (49.04%) | |||
When comparing listings with exception points to those without, relisted patients with exception points (group 3) were the youngest among the four groups (mean age at listing 47.3 vs. 59.4, 55.9 and 52 years for group 1, 2, and 4 respectively, p < 0.001). Relisted candidates had a low prevalence of hypertension, especially those without exception points.
Encephalopathy, ascites SBP, HRS, and variceal bleeding were most prevalent in primary listed candidates without exception points (group 2). Considering biological markers, relisted without exception points (group 4) had the highest levels of bilirubin, INR and creatinine among all the four groups. (Supplementary table 1) Median biological MELD-Na scores at the time of listing were typically higher for those without exception points in both primary (group 2: 20, 6 – 55) and relisted cohorts (group 4: 22.5, 8 – 49) as compared to those with exception points in primary (group 1: 12, 6 – 38) and relisted patients (group 3: 16, 6 – 30).
Relisted candidates without exception points (group 4) spent shorter time on waitlist (median 126 vs. 219, 129, and 259 days), were transplanted least frequently (44.8% vs. 67.1, 59.4%, and 54.3%, p=0.001) and carried highest mortality (41.4% vs. 5.6, 21.7%, and 13%, p<0.0001) as compared to group 1, 2 and 3 respectively. (Supplementary table 1) We further stratified according to patients who died vs. who received transplant to see any difference in time on waitlist. Primary listed without exceptions (group 2) died earlier with a median time of 1 day (79 – 1455) as compared to group 1 (49, 170 – 524), group 3 (172, 220 – 451) and group 4 (3, 102 – 1689). Nonetheless, primary listed without exception points (group 2) received transplant earlier within a median time of 95 days (0 – 2108) as compared to group 1 (212, 15 – 2360), group 3 (167, 1 – 806) and group 4 (113, 0 – 566).
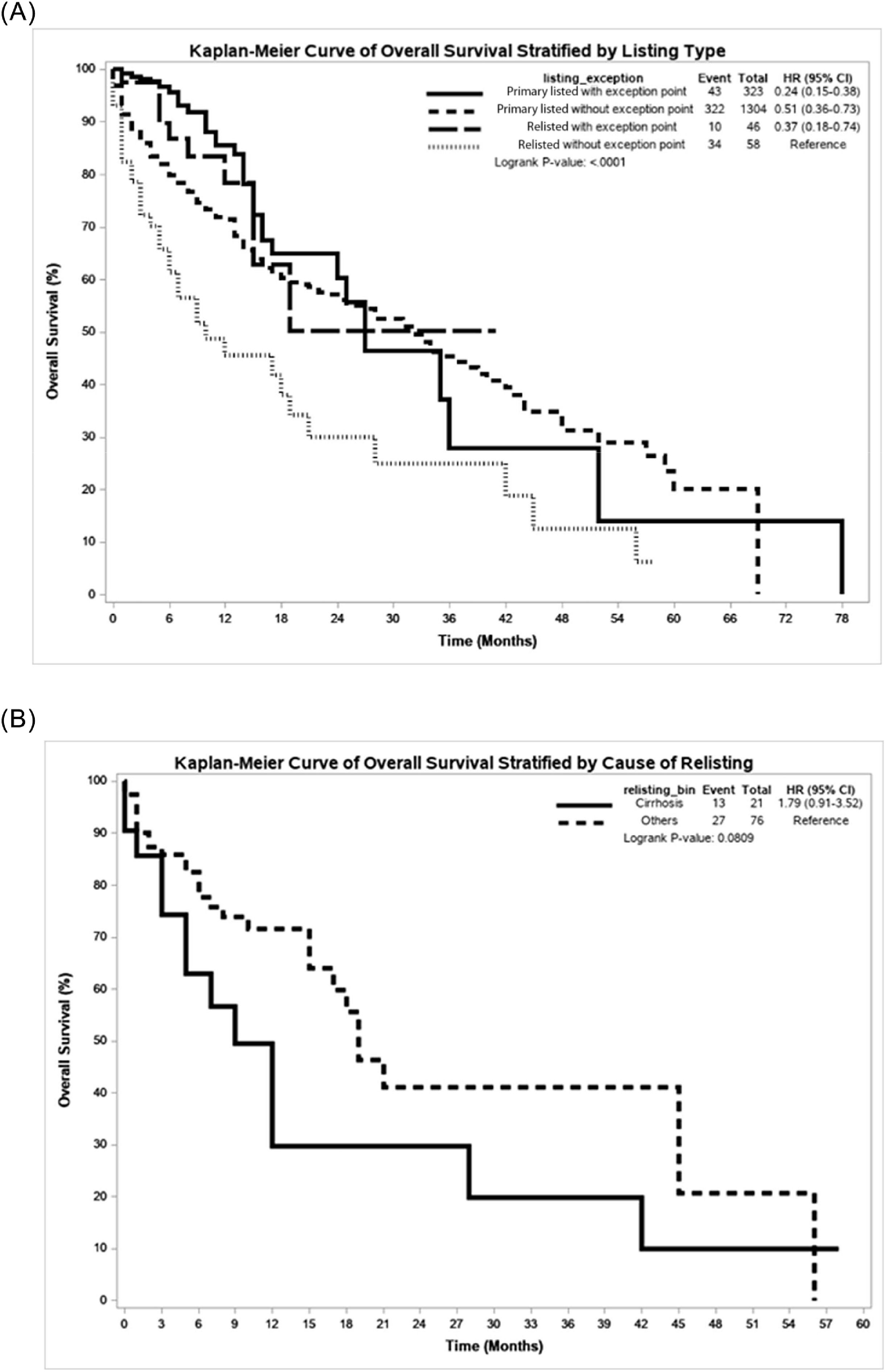
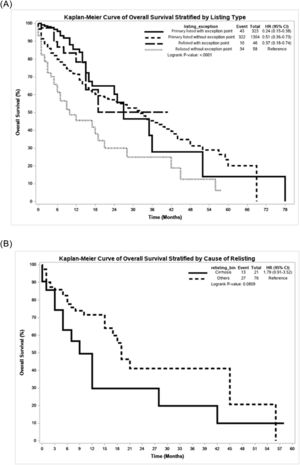
3.4Overall survivalFig. 1A demonstrates that overall survival is affected by the dissemination of exception points. Group 1 (HR: 0.24, 95%CI 0.15 – 0.30), group 2 (HR: 0.51, 95%CI 0.36 – 0.72) and group 3 (HR: 0.37, 95%CI 0.18 – 0.74) had better survival than group 4 patients (p<0.001).
On multivariate analysis (Table 2), listing type (stratified by exception points) was significantly associated with overall survival (p=0.00125). Specifically, compared to group 4, the instantaneous rate of death was 61% lower in group 1 (HR: 0.386, 95% CI 0.236 – 0.632, p<0.002), while it was 41% lower in group 2 (HR: 0.59, 95% CI 0.403 – 0.863, p=0.0065). The instantaneous rate of death did not differ between group 3 and 4.
Multivariate analysis - overall survival stratified by listing type.
| Parameter | HR | 95% CI | P value | ||
|---|---|---|---|---|---|
| Listing type(Ref: relisted without exception | Primary listed with exception point | 0.386 | 0.236 – 0.632 | <0.002 | 0.0025 |
| Primary listed without exception point | 0.590 | 0.403 – 0.863 | 0.0065 | ||
| Relisted with exception point | 0.611 | 0.295 – 1.266 | 0.185 | ||
| Etiology(Ref: NASH) | Autoimmune | 2.773 | 1.549 – 4.964 | 0.0006 | 0.0006 |
| Cholestatic | 1.601 | 1.032 – 2.483 | 0.036 | ||
| Cryptogenic | 3.123 | 1.743 – 5.596 | 0.0001 | ||
| ETOH | 2.111 | 1.445 – 3.085 | 0.0001 | ||
| Metabolic | 2.696 | 1.095 – 6.639 | 0.031 | ||
| Others | 2.455 | 1.162 – 5.189 | 0.019 | ||
| Viral | 2.033 | 1.401 – 2.952 | 0.0002 | ||
| Height at listing | 0.995 | 0.984 – 1.006 | 0.342 | ||
| Age at listing | 1.027 | 1.015 – 1.040 | <0.0001 | ||
| Bilirubin at listing | 1.003 | 1.002 – 1.003 | <0.0001 | ||
| INR at listing | 1.476 | 1.352 – 1.611 | <0.0001 | ||
| Sodium at listing | 0.960 | 0.937 – 0.984 | 0.0011 | ||
| Creatinine at listing | 1.002 | 1.001 – 1.003 | <0.0001 | ||
Multivariate Cox proportional hazard model suggested that in addition to listing type (stratified by exception point), primary etiology, bilirubin, INR, sodium, and creatinine are significantly associated with overall survival. (Table 2) When compared to NASH, cryptogenic cirrhosis carried highest risk of mortality (HR: 3.123, 95%CI 1.743 – 5.596, p=0.0001) followed by autoimmune (HR: 2.773, 95%CI 1.549 – 4.964, p=0.0006) and metabolic causes (HR: 2.696, 95%CI 1.095 – 6.639, p=0.031). With increase in age at listing by 1 year, the instantaneous rate of death was increased by 2.7% (HR: 1.027, 95%CI 1.015 – 1.040, p <0.0001). Looking toward biological parameters, as bilirubin at listing increased by 1 µmol/L, instantaneous rate of death was increased by 0.3% (HR: 1.003, 95%CI 1.002 – 1.003, p<0.0001). As INR at listing increased by 1 unit, the instantaneous rate of death was increased by 47% (HR: 1.476, 95%CI 1.352 – 1.611, p<0.0001). As sodium at listing increased by 1 mmol/L, instantaneous rate of death was decreased by 4% (HR: 0.96, 95%CI 0.937 – 0.984, p=0.0011). As creatinine at listing increases by 1 µmol/L, instantaneous rate of death increases by 0.2% (HR: 1.002, 95%CI 1.001 – 1.003, p<0.0001). Height was not associated with overall survival (p=0.41).
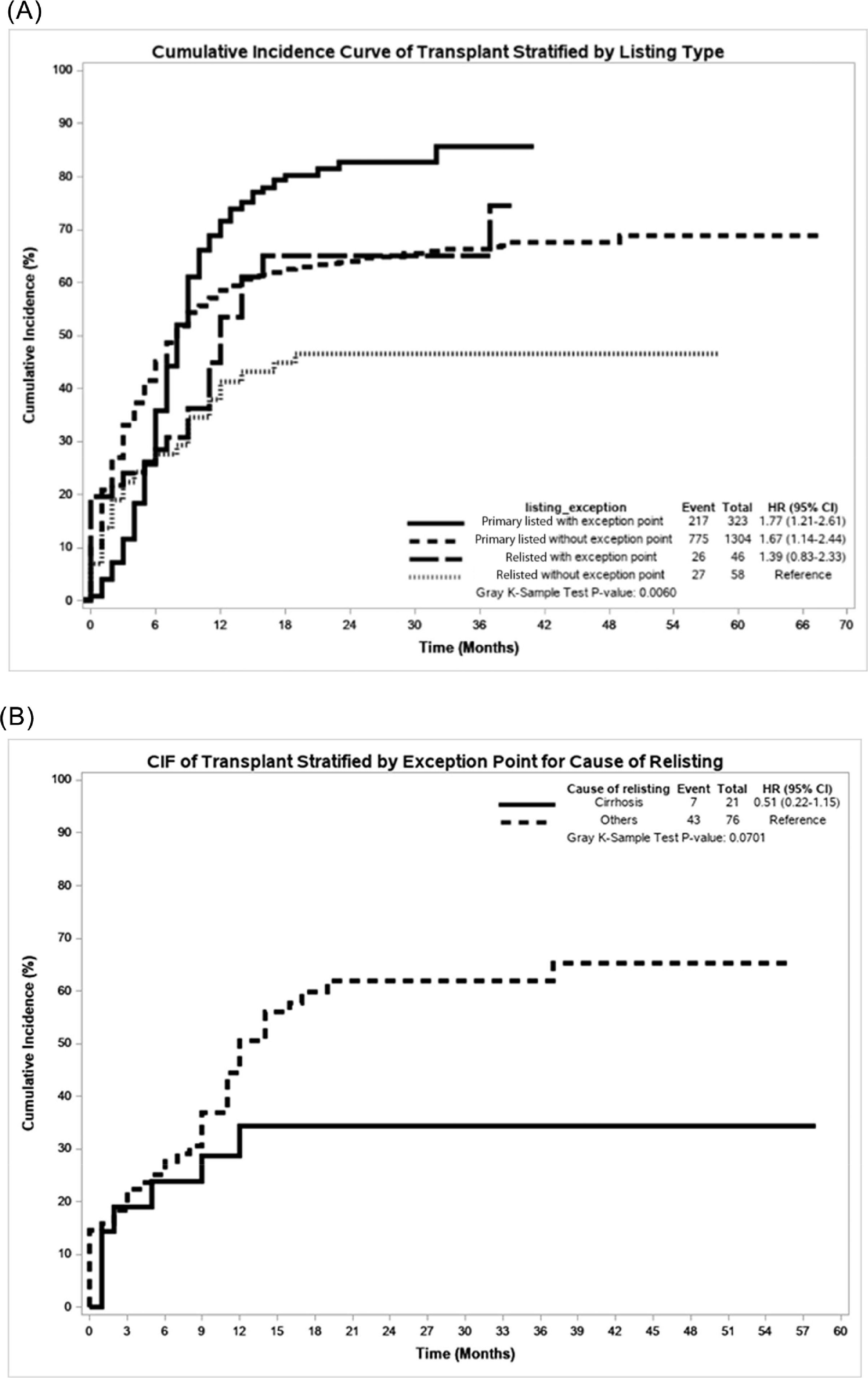
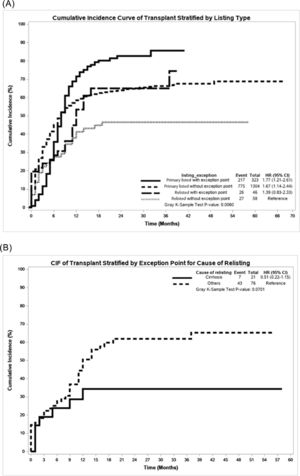
3.5Cumulative incidence of transplantFig. 2A demonstrates that cumulative incidence of transplant was affected by the type of listing and exception points. Group 1 (HR: 1.77, 95%CI 1.21 – 2.61), and Group 2 (HR: 1.67, 95%CI 1.14 – 2.44) had higher cumulative incidence of transplant than group 4 patients (p<0.006).
Listing type (stratified by exception points) was significantly associated with cumulative incidence of transplant (p=0.0011) (Table 3). Specifically, the instantaneous rate of transplant among group 2 was 1.75 times higher than group 4 (HR: 1.756, 95%CI 1.176 – 2.621, p=0.006).
Multivariate analysis for cumulative incidence of transplant.
| Parameter | HR | 95% CI | P value | ||
|---|---|---|---|---|---|
| Listing type(Ref: Relisted without exception | Primary listed with exception point | 1.499 | 0.990 – 2.269 | 0.056 | 0.0011 |
| Primary listed without exception point | 1.756 | 1.176 – 2.621 | 0.006 | ||
| Relisted with exception point | 1.098 | 0.650 – 1.853 | 0.728 | ||
| Etiology(Ref: NASH) | Autoimmune | 1.168 | 0.799 – 1.709 | 0.422 | 0.0054 |
| Cholestatic | 0.838 | 0.666 – 1.054 | 0.131 | ||
| Cryptogenic | 0.792 | 0.502 – 1.249 | 0.315 | ||
| ETOH | 0.857 | 0.700 – 1.050 | 0.137 | ||
| Metabolic | 1.650 | 1.171 – 2.324 | 0.0042 | ||
| Others | 0.968 | 0.711 – 1.317 | 0.835 | ||
| Viral | 0.958 | 0.807 – 1.138 | 0.628 | ||
| Height at listing | 1.012 | 1.006 – 1.018 | 0.0001 | ||
| Age at listing | 0.987 | 0.981 – 0.993 | <0.0001 | ||
| Bilirubin at listing | 0.999 | 0.998 – 1.000 | 0.023 | ||
| INR at listing | 0.595 | 0.489 – 0.724 | <0.0001 | ||
| Sodium at listing | 1.011 | 0.995 – 1.027 | 0.171 | ||
| Creatinine at listing | 1.000 | 0.999 – 1.001 | 0.950 | ||
Multivariate Fine-Gray model revealed in addition to listing type (stratified by exception point), primary etiology, height, bilirubin and INR were significantly associated with cumulative incidence of transplant. When compared to NASH, metabolic diseases appeared to have a better incidence of transplant (HR 1.65, 95% CI: 1.171 – 2.324, p=0.004). As patient height increased by 1 cm, the instantaneous rate of transplant increased by 1.2% (HR: 1.012, 95%CI 1.006 – 1.018, p=0.0001). As age at listing increased by 1 year, the instantaneous rate of transplant decreased by 1.3% (HR: 0.987, 95%CI 0.981 – 0.993, p<0.0001). As bilirubin at listing increased by 1 µmol/L, the instantaneous rate of transplant decreased by 0.1% (HR: 0.999, 95%CI 0.998 – 1.000, p=0.023). As INR at listing increased by 1 unit, the instantaneous rate of transplant decreased by 34% (HR: 0.6595, 95%CI 0.489 – 0.724, p<0.0001). Sodium at listing and creatinine at listing were not associated with instantaneous rate of the transplant.
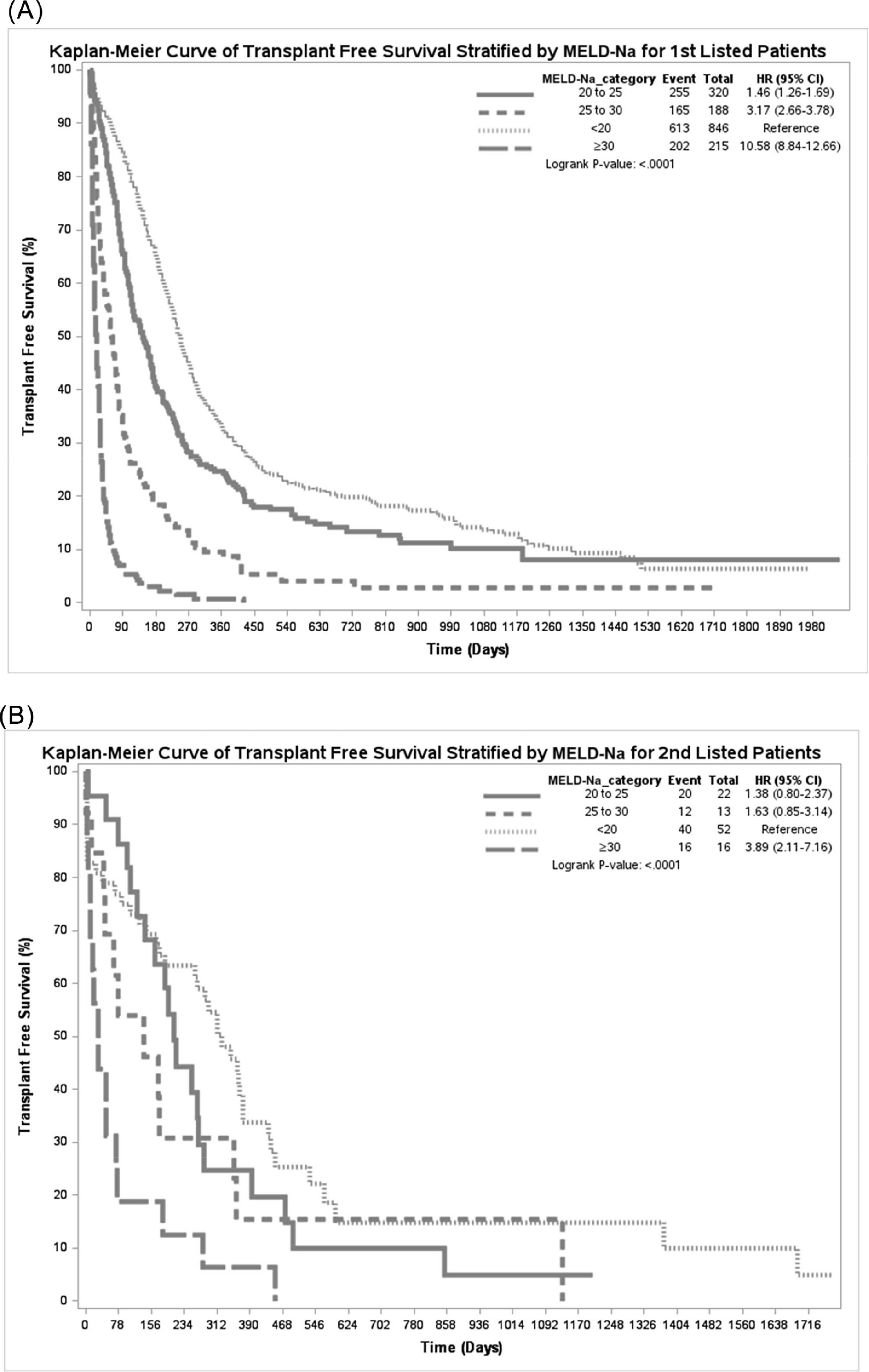
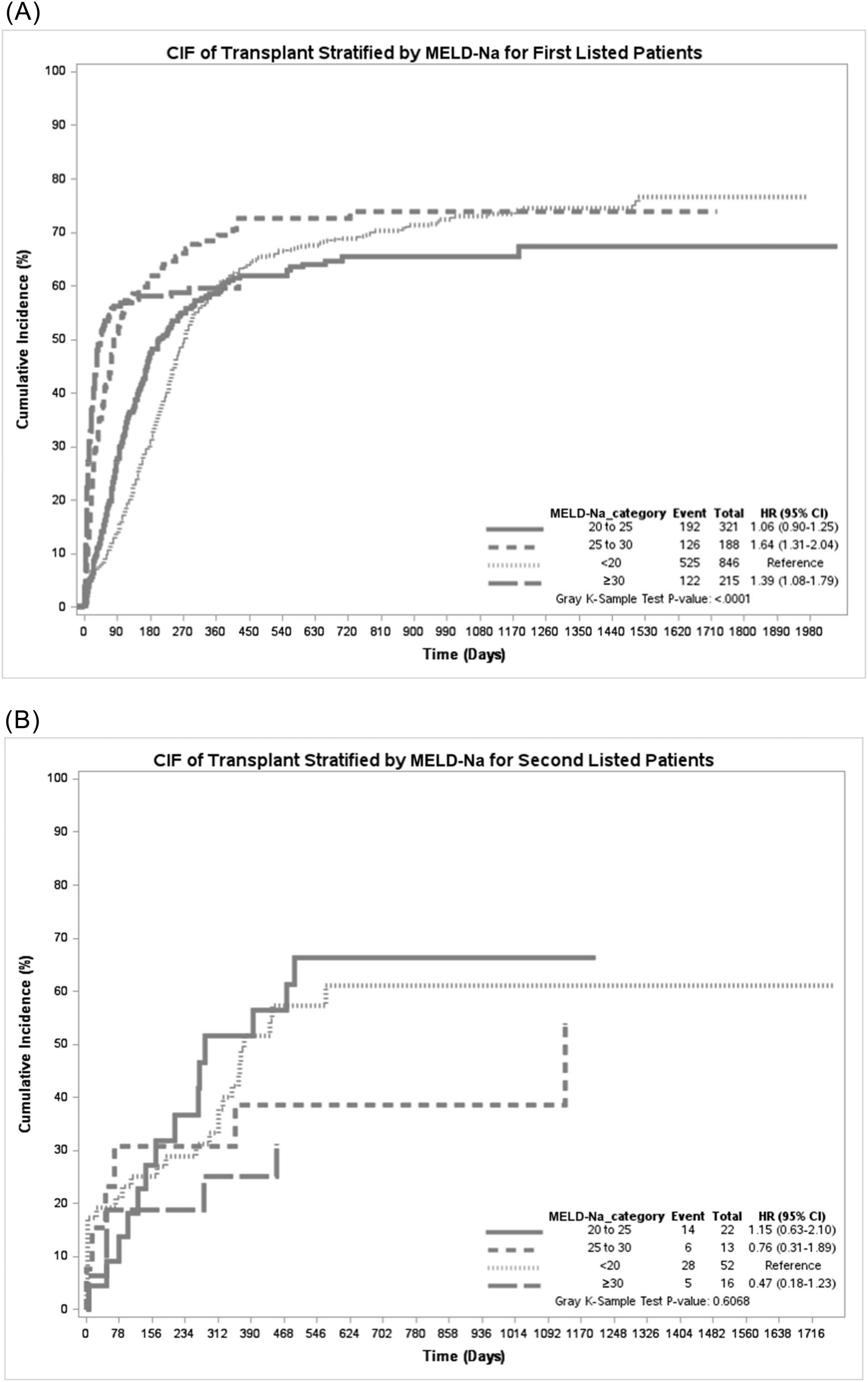
3.6Stratification by MELD-Na scoreTransplant-free survival among primary listed patients was worst for patients with MELD-Na ≥30 (HR: 10.58, 95%CI 8.84 – 12.66) followed by MELD-Na 25-29 (HR: 3.17, 95%CI 2.66 – 3.78) and MELD-Na 20-24 (HR: 1.46, 95%CI 1.26 – 1.69) as compared to MELD-Na ≤19 (p<0.0001). While transplant free survival among relisted patients was poor only for patients with MELD-Na ≥30 (HR: 3.89, 95%CI 2.11 – 7.16, p<0.0001) but not different for MELD-Na 25-29 (HR: 1.63, 95%CI 0.85 – 3.14) and MELD-Na 20-24 (HR: 1.38, 95%CI 0.80 – 2.37) as compared to MELD-Na ≤19. (Fig. 3) The cumulative incidence of transplant among primary listed patients was highest for patients with MELD-Na ≥30 (HR: 1.39, 95%CI 1.08 – 1.79) followed by MELD-Na 25-29 (HR: 1.64, 95%CI 1.31 – 2.04) but and MELD-Na 20-24 (HR: 1.06, 95%CI 0.90 – 1.25) as compared to MELD-Na ≤19 (<0.001). However, the cumulative incidence of transplant was not different among relisted patients when stratified by MELD-Na (p=0.6) (Fig. 4).
Within the relisted group of patients, there was a trend towards higher waitlist mortality (HR: 1.79, 95%CI 0.91 – 3.52, p=0.08) and lower cumulative incidence of transplant (HR: 0.51, 95%CI 0.22 – 1.15, p=0.07) for patients relisted for graft cirrhosis as compared to biliary/vascular reasons (Figs. 1B and 2B). On multivariate analysis (Table 4), compared to patients with graft cirrhosis, the instantaneous rate of death was 64% lower in patients relisted due to biliary/vascular causes (HR: 0.36, 95%CI 0.14 – 0.93, p<0.035). Height and sodium at listing remain significant though age at listing did not appear significant.
Overall survival stratified by cause of relisting.
| Parameter | HR | 95% CI | P Value |
|---|---|---|---|
| Reason of relisting(Biliary/vascular*vs Cirrhosis) | 0.36 | 0.14 – 0.93 | 0.035 |
| Height at listing | 0.93 | 0.87 – 0.98 | 0.013 |
| Sodium at listing | 0.84 | 0.74 – 0.96 | 0.0118 |
| Age at listing | 0.99 | 0.95 – 1.03 | 0.62 |
Transplant remains the gold standard procedure for acute and chronic liver disease due to various etiologies [11]. Relisted candidates with liver grafts present with portal hypertensive complications without significantly elevated MELD-Na score; suggesting a lag between portal hypertensive complications and synthetic dysfunction in relisted patients. Therefore, the MELD-Na is unable to reflect the degree of disease severity among relisted patients. Additionally, these patients have been immunosuppressed for years, and are even more susceptible to infectious complications and greater severity of sepsis. Within this study, the trajectory of re-listed candidates was compared to primary candidates to elucidate a difference in outcomes on the transplant waiting list.
From an ethical standpoint, strict scrutiny exists surrounding the necessity of retransplant listings [12]. Considering organs are a limited commodity on an oversaturated waitlist, many ethicists carefully examine the utility of relisting candidates. Given that retransplant candidates tend to present sicker than primary transplant candidates, questions surrounding their outcomes are also raised [13].
Nonetheless, the incidence of re-transplant ranges from 4.8%-7% worldwide with numbers increasing annually [14–18]. While historically outcomes for retransplantation were dismal [15,19,20] compared to primary transplant outcomes, survival has increased over the years [17,18]. A recent study based on the Canadian experience found comparable values with a 5-year patient survival of 65.6% [17]. A study based on an Australian and New Zealand cohort found increasing patient survival when comparing patient retransplant outcomes post-2000 to pre-2000. When comparing 5-year survival between the 1986-2017 and 2001-2017 era, both overall survival and graft survival increased in the latter cohort with patient survival only being 72% at five years in 1986-2017 compared to 81% in 2001-2017 [18]. These improvements in patient survival can be understood in reference to advances in transplant medicine, immunosuppression as well as an improvement in surgical techniques. Focusing on comorbidities related to transplant such as antiviral therapies has also optimized graft survival.
While rates of retransplantation have increased over the years along with outcomes post-retransplant, retransplant patients have suffered disproportionately on the waitlist compared to primary transplant candidates. The implementation of the MELD-Na has led to an improvement in waitlist outcomes for select populations since its advent and has been seen as an accurate predictor of waitlist mortality. [6] Nonetheless, improvement can always be made and as Kim et al suggest, certain subpopulations are not well-served by this system and re-transplant patients have been proven to be one such population [6]. There may be situations in which the risk of adverse outcomes is not related to a worsening of liver function rendering the MELD score void [2,21,22]. For cases such as these, MELD exceptions exist which disseminate points to patients with morbidities that are not reflected in the MELD score such as hepatocellular carcinoma. While determining the best candidate for receiving a transplant in an already oversaturated system remains an ethical discourse, further research into the clinical considerations through evidence-based discourse can offer key insight into this inquiry.
The MELD score is a measurement of both hepatic as well as renal function with MELD-Na being a recent addition. MELD is based on the ‘sickest first’ principle that calculates bilirubin, creatinine and international normalized ratio levels [23]. Patients are expected to have greater MELD scores when they suffer from hepatic impairments. In patients with other common morbidities such as ascites, hepatocellular carcinoma (HCC) or cholestatic disease, the worsening situation is not reflected in an increased MELD score which requires a correction to accurately reflect the status of the patient. In the case of cholestatic diseases for example, until a very late stage, a low MELD score is maintained due to a normal INR as well as creatinine levels [21,22]. This introduces the concept of exception points which are awarded to patients when they have complications that are not reflected in MELD.
Waitlist outcomes from primary to retransplant candidates have not been compared in great detail in the literature, with the work by Kim et al being the most relevant to the MELD era [6]. Previous studies based on the Organ Procurement and Transplantation Network (OPTN) demonstrated a correlation between MELD scores for both primary and re-LT candidates [24,25]. All these studies demonstrated candidates to be overall sicker when listed for re-LT which our study concurs as seen by increased ICU hospitalization rates as well as inferior outcomes on the waiting list. Re-LT participants on average had higher creatinine and bilirubin scores in our study. Previous studies suggest these inflated values to be associated with nephrotoxicity of post-LT drugs and the high presence of cholangiopathy to explain higher bilirubin levels [6]. This is important to consider because it suggests that the extent of the liver disease may be worse for re-LT candidates than primary LT candidates. Our study further suggests this, given the high rates of death while on the waiting list for re-LT patients at 28.85% compared to primary listing at 18.50%. We also showed that the MELD-Na does not accurately reflect severity of disease in re-LT candidates, given that they were less likely to attract an organ offer.
A recent study exploring from our own centre elucidated that recipient age, donor age, as well as donor cytomegalovirus (CMV) status, were all independent predictors of patient and graft survival after re-LT [17]. Our own study found that with increase in recipient's age at listing by 1 year, the instantaneous rate of death was increased by 2.1% (HR: 1.021, 95%CI 1.009 – 1.032, p <0.0003), further validating the literature. Considering etiologies of underlying liver diagnosis, a staggering 29.4% of patients were listed due to viral causes within our study. Previous literature (Rosen et al) has elucidated that CMV infection and hepatitis C virus (HCV) infection are conducive to worse outcomes post-transplant and re-transplant [26]. Our study found no correlation between a positive HCV diagnosis and worse outcomes confirming the Yoon et al study from 2022 [17].
A strength of this study is the focus on stratification by exception point dissemination as well as reason for relisting which further sheds light on outcomes when situated on the transplant waiting list. A recent study found an increased probability of transplantation for patients with MELD exceptions on the waiting list, especially those with HCC exceptions [21]. Another recent study found that access to liver transplants was adequately balanced between groups and found a similar drop-out rate for patients with hepatic insufficiency to the remaining cohort suggesting an adequate allocation policy [21,22]. Our study further compared exception point dissemination between primary and relisted patients and found a significant advantage difference. Primary listed candidates with exception points had highly favorable outcomes on the waiting list with a 67.18% transplant rate compared to relisted candidates without exception points who only had a 44.83% transplantation rate. Furthermore, relisted candidates on average had a higher death rate on the waiting list for both exception and non-exception status compared to primary listings. This follows similar findings to Edward et al as well as Kim et al that elucidated that primary transplant candidates on average have better outcomes on the waiting list [6,25]. More crucial than this, our study showed the cumulative incidence of transplant was associated with exception point dissemination. Our study also compared primary listed candidates without exception points to relisted patients with exception points. The analyses revealed the relisted patients with exception points fared similarly to the primary listed without exception points (HR: 0.90). This suggests that awarding exception points to those relisted for transplant can level the outcomes when placed against those who are primary listed. Since those relisted tend to have overall worse outcomes on the transplant waiting list compared to primary listed candidates, this offers support for relisted candidates on the transplant waiting list.
Ultimately, while exception points may ameliorate some of the dissonance posed by differences between primary and relisted candidates as well as morbidities not reflected in the MELD score, further modifications can be made to accommodate these variations. Our study demonstrated the dissemination of exception points to have a minor improvement in both overall survivals on the waiting list as well as the incidence of transplant but also demonstrated a noticeable difference between different subgroups, specifically primarily listed patients with exception points compared to relisted candidates with exception points. Finally, the awarding of exception points can level the overall survival difference between primary listed candidates without exception points to those relisted.
4.1LimitationsOur study focused on a single centre and a retrospective design which is prone to recall bias and cannot discern causation. Furthermore, patients placed temporarily on hold or withdrawn from the waiting list and then relisted were not considered separately from the rest of the data which could have artificially inflated waitlist times. Additionally, those patients listed for graft cirrhosis have limited or no comorbidities, which may limit relevance to the outcomes of older relisted patients. Moreover, MELD exception points may vary from country to country. One could argue about excluding the patients with clinical improvement on the waitlist. However, as the goal of our study was to compare outcomes between patients who received a transplant and those who dropped off the waitlist, it was appropriate to exclude patients delisted due to clinical improvement [27].
4.2StrengthsThis study harnessed a large sample size and provided data on a previously underreported phenomenon. This study will be a significant addition to the existing literature on waitlist outcomes for retransplant patients.
5ConclusionsLooking specifically toward the graft cirrhosis demographic, they are carefully curated and compromise a minority of the waitlist population. They tend to be younger, however often have worse liver and kidney function, tend to fare worse off on the waitlist and have a decreased incidence of transplant. Therefore, based on these findings, there is an impetus to relist graft cirrhosis patients earlier while simultaneously considering liver donor liver transplantation as a viable option as well as standardized exception point dissemination for this population.