Amyloidosis is a rare disease that is caused by extracellular deposits of amorphous, insoluble fibrillar protein, which often occur in the kidneys, the heart, the nervous system, the digestive tract, especially the hepatosplenic and intestinal tract, and can be present in bone marrow, though unusual in the gallbladder. The interest of this case lies in the rarity of amyloidosis localisation and in the uncommon clinical presentation as acute cholecystitis.
We have reviewed cases of amyloidosis with gallbladder involvement in literature and briefly discussed the predictive value of the main histological diagnostic methods.
Amyloidosis is a rare disease that is caused by extracellular deposits of amorphous, insoluble fibrillar protein. Five different types have been identified: immunoglobulin-associated amyloidosis, secondary amyloidosis; hemodialysis-associated amyloidosis, familial amyloidosis and senile amyloidosis.
We will describe a case of primary amyloidosis with heart, bone marrow and gallbladder involvement, with the uncommon clinical presentation as acute cholecystitis. Amyloid deposition is in fact frequent in the kidneys, the heart, the nervous system, the hepatosplenic and intestinal tract and can be present in bone marrow (40% of cases), but localisation in the gallbladder is uncommon.
We have reviewed cases of amyloidosis with gallbladder involvement in literature and briefly discussed the predictive value of the main histological diagnostic methods.
Case ReportA 74-years-old patient was experiencing abdominal pain in the right hypochondrium and epigastrium.
The patient’s medical history includes bronchial asthma at a young age, hypertension, mild dyslipidemia and also recent hospitalisation for pneumonia. Physical examination showed right upper quadrant pain, positive Murphy’s sign, jaundice, and a grade 2/6 systolic heart murmur.
Laboratory tests reveal alterations in liver and pancreatic function (AST/ALT 70/73 U/l, gamma GT 231 U/l, ALP 220 U/l, amylase 216 U/1, lipase 281 U/1), and also biological inflammatory syndrome (C reactive protein 16 mg/dL).
An ultrasound to the abdomen detected diffuse gallbladder wall thickening (maximum diameter 6.3 mm), biliary sand and pericholecystic fluid (Figure 1). We also performed abdomen CT scan without contrast medium (serum creatinine is moderately increased), which did not confirm involvement of pancreatic parenchyma. The patient was diagnosed with acute cholecystitis and was placed on antibiotics.
During hospitalisation, however, two clinical problems occurred: electrocardiographic changes (little progression of R waves in precordial leads and T negative in lateral precordial leads) with cardiac enzymes negatives and on another occasion a significant monoclonal component.
Echocardiogram showed cardiomyopathy with severe concentric left ventricular hypertrophy. Moreover serum IgG lambda monoclonal levels were 17.3 g/l and blood tests showed: normocytic anaemia (Hb 10.3 g/dL, MCV 88), mild renal insufficiency (creatinine 1.8 mg/dL), finally, calcium levels, LDH, uric acid, microalbuminuria and urinary Bence Jones protein negatives.
Amyloidosis was suspected for gammopathy and discrepancy between low voltage QRS complex and echocardiography evidence of left ventricular hypertrophy. Furthermore a bone marrow biopsy was performed, which was compatible with multiple myeloma in the first anatomopathologic stage with micro hyaline deposits of amyloid in vessel walls. Finally X-rays of the shoulders, pelvis, spine and cranium were negative for osteolysis.
The patient was discharged, pending a minimally invasive cholecystectomy. Post discharge a periumbilical fat biopsy and a rectal submucosa were performed, both resulting negative for amyloidosis. Finally, a histological examination of the gallbladder, after cholecystectomy, detected ulcerated chronic cholecystitis with amyloid deposits, Congo red-positive in the lamina propria mucosae and vessel walls (Figure 2). We concluded, therefore, with a diagnosis of multiple myeloma, stage II, associated with amyloidosis, with cardiac, bone marrow and gallbladder involvement.
The patient was sent to a Center for amyloidosis, where the periumbilical fat biopsy proved positive for amyloidosis. The patient underwent a course of therapy with high dose dexamethasone, with mild reduction in monoclonal components and subsequently Leukeran-Prednisone chemotherapy.
DiscussionIn literature reports of outbreaks of multiple myeloma as acute cholecystitis are rare; the trigger, however is a general increased susceptibility to infections.1-3 Moreover, acute cholecystitis is less common than other diseases, such as, for example, pneumonia.
Cholecistitis secondary to gallbladder localisation of amyloidosis is even more unusual: generally amyloidosis affects the epithelium of the intrahepatic bile duct without reaching canaliculi and acini of glandular peribiliaires and the amount of bile deposits correlates with the extent of amyloidosis in liver parenchyma.4 In particular gallbladder localisation of amyloidosis has never been observed in experimental models of amyloidosis,5 in routine histopathological examinations of gallbladder in patients without liver amyloidosis,6 nor in a series of 21 patients with amyloidosis associated with polyneuropathy.7
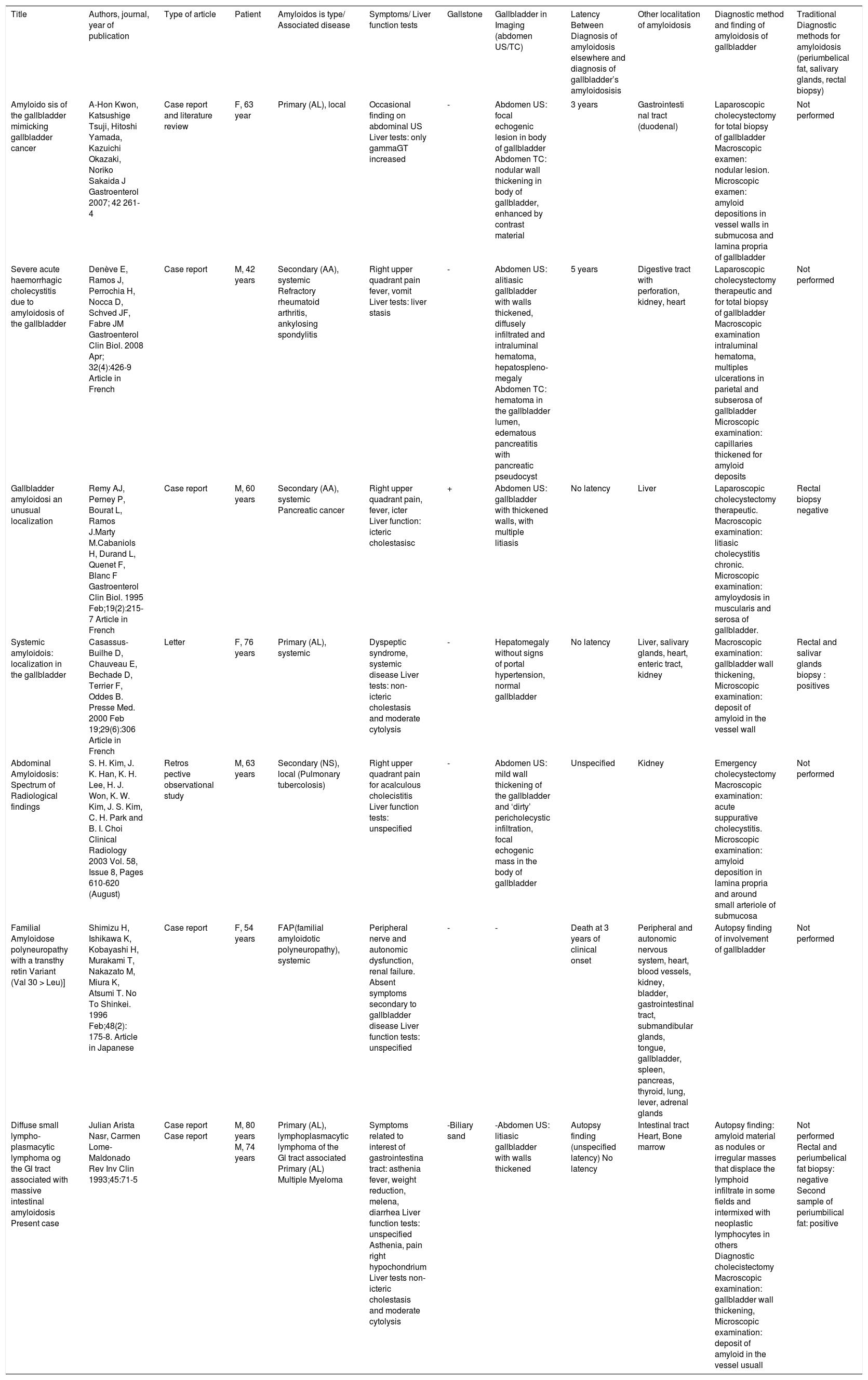
Therefore we performed a systematic research on Pubmed for cases of gallbladder involvement (Mesh term ‘cholecystitis’ AND ‘amyloidosis’ and, then, ‘gallbladder’ AND ‘amyloidosis’, with detailed control of references). We obtained 10 cases; we excluded three8-10 for temporal limits (temporal limits: 1990-2010), with total of seven cases (Table 1).
Cases with gallbladder localization of amyloidosis in literature. Abdomen US: abdomen ultrasonography; Abdomen TC: abdomen computed tomography.
| Title | Authors, journal, year of publication | Type of article | Patient | Amyloidos is type/ Associated disease | Symptoms/ Liver function tests | Gallstone | Gallbladder in Imaging (abdomen US/TC) | Latency Between Diagnosis of amyloidosis elsewhere and diagnosis of gallbladder’s amyloidosisis | Other localitation of amyloidosis | Diagnostic method and finding of amyloidosis of gallbladder | Traditional Diagnostic methods for amyloidosis (periumbelical fat, salivary glands, rectal biopsy) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Amyloido sis of the gallbladder mimicking gallbladder cancer | A-Hon Kwon, Katsushige Tsuji, Hitoshi Yamada, Kazuichi Okazaki, Noriko Sakaida J Gastroenterol 2007; 42 261-4 | Case report and literature review | F, 63 year | Primary (AL), local | Occasional finding on abdominal US Liver tests: only gammaGT increased | - | Abdomen US: focal echogenic lesion in body of gallbladder Abdomen TC: nodular wall thickening in body of gallbladder, enhanced by contrast material | 3 years | Gastrointesti nal tract (duodenal) | Laparoscopic cholecystectomy for total biopsy of gallbladder Macroscopic examen: nodular lesion. Microscopic examen: amyloid depositions in vessel walls in submucosa and lamina propria of gallbladder | Not performed |
| Severe acute haemorrhagic cholecystitis due to amyloidosis of the gallbladder | Denève E, Ramos J, Perrochia H, Nocca D, Schved JF, Fabre JM Gastroenterol Clin Biol. 2008 Apr; 32(4):426-9 Article in French | Case report | M, 42 years | Secondary (AA), systemic Refractory rheumatoid arthritis, ankylosing spondylitis | Right upper quadrant pain fever, vomit Liver tests: liver stasis | - | Abdomen US: alitiasic gallbladder with walls thickened, diffusely infiltrated and intraluminal hematoma, hepatospleno-megaly Abdomen TC: hematoma in the gallbladder lumen, edematous pancreatitis with pancreatic pseudocyst | 5 years | Digestive tract with perforation, kidney, heart | Laparoscopic cholecystectomy therapeutic and for total biopsy of gallbladder Macroscopic examination intraluminal hematoma, multiples ulcerations in parietal and subserosa of gallbladder Microscopic examination: capillaries thickened for amyloid deposits | Not performed |
| Gallbladder amyloidosi an unusual localization | Remy AJ, Perney P, Bourat L, Ramos J.Marty M.Cabaniols H, Durand L, Quenet F, Blanc F Gastroenterol Clin Biol. 1995 Feb;19(2):215-7 Article in French | Case report | M, 60 years | Secondary (AA), systemic Pancreatic cancer | Right upper quadrant pain, fever, icter Liver function: icteric cholestasisc | + | Abdomen US: gallbladder with thickened walls, with multiple litiasis | No latency | Liver | Laparoscopic cholecystectomy therapeutic. Macroscopic examination: litiasic cholecystitis chronic. Microscopic examination: amyloydosis in muscularis and serosa of gallbladder. | Rectal biopsy negative |
| Systemic amyloidois: localization in the gallbladder | Casassus-Builhe D, Chauveau E, Bechade D, Terrier F, Oddes B. Presse Med. 2000 Feb 19;29(6):306 Article in French | Letter | F, 76 years | Primary (AL), systemic | Dyspeptic syndrome, systemic disease Liver tests: non-icteric cholestasis and moderate cytolysis | - | Hepatomegaly without signs of portal hypertension, normal gallbladder | No latency | Liver, salivary glands, heart, enteric tract, kidney | Macroscopic examination: gallbladder wall thickening, Microscopic examination: deposit of amyloid in the vessel wall | Rectal and salivar glands biopsy : positives |
| Abdominal Amyloidosis: Spectrum of Radiological findings | S. H. Kim, J. K. Han, K. H. Lee, H. J. Won, K. W. Kim, J. S. Kim, C. H. Park and B. I. Choi Clinical Radiology 2003 Vol. 58, Issue 8, Pages 610-620 (August) | Retros pective observational study | M, 63 years | Secondary (NS), local (Pulmonary tubercolosis) | Right upper quadrant pain for acalculous cholecistitis Liver function tests: unspecified | - | Abdomen US: mild wall thickening of the gallbladder and ‘dirty’ pericholecystic infiltration, focal echogenic mass in the body of gallbladder | Unspecified | Kidney | Emergency cholecystectomy Macroscopic examination: acute suppurative cholecystitis. Microscopic examination: amyloid deposition in lamina propria and around small arteriole of submucosa | Not performed |
| Familial Amyloidose polyneuropathy with a transthy retin Variant (Val 30 > Leu)] | Shimizu H, Ishikawa K, Kobayashi H, Murakami T, Nakazato M, Miura K, Atsumi T. No To Shinkei. 1996 Feb;48(2): 175-8. Article in Japanese | Case report | F, 54 years | FAP(familial amyloidotic polyneuropathy), systemic | Peripheral nerve and autonomic dysfunction, renal failure. Absent symptoms secondary to gallbladder disease Liver function tests: unspecified | - | - | Death at 3 years of clinical onset | Peripheral and autonomic nervous system, heart, blood vessels, kidney, bladder, gastrointestinal tract, submandibular glands, tongue, gallbladder, spleen, pancreas, thyroid, lung, lever, adrenal glands | Autopsy finding of involvement of gallbladder | Not performed |
| Diffuse small lympho-plasmacytic lymphoma og the Gl tract associated with massive intestinal amyloidosis Present case | Julian Arista Nasr, Carmen Lome-Maldonado Rev Inv Clin 1993;45:71-5 | Case report Case report | M, 80 years M, 74 years | Primary (AL), lymphoplasmacytic lymphoma of the Gl tract associated Primary (AL) Multiple Myeloma | Symptoms related to interest of gastrointestina tract: asthenia fever, weight reduction, melena, diarrhea Liver function tests: unspecified Asthenia, pain right hypochondrium Liver tests non-icteric cholestasis and moderate cytolysis | -Biliary sand | -Abdomen US: litiasic gallbladder with walls thickened | Autopsy finding (unspecified latency) No latency | Intestinal tract Heart, Bone marrow | Autopsy finding: amyloid material as nodules or irregular masses that displace the lymphoid infiltrate in some fields and intermixed with neoplastic lymphocytes in others Diagnostic cholecistectomy Macroscopic examination: gallbladder wall thickening, Microscopic examination: deposit of amyloid in the vessel usuall | Not performed Rectal and periumbelical fat biopsy: negative Second sample of periumbilical fat: positive |
Although the number of cases is small, gallbladder involvement appears to be present equally in primary and secondary forms, while there is a single case of familial amyloidosis.
Clinical spectrum is very wide: no symptoms,4 dyspeptic symptoms11 or, finally, systemic disease or disease related to other organs involvement.12-14 Laboratory tests and imaging also are very varied: only unspecific gammaGT increase,4 anicteric cholestasis,15 jaundice,16 moderate cytolysis,14 in addition nodular or diffuse wall thickening of gallbladder,4,11,15 intraluminal hematoma;15 sometimes generic hepatomegaly only.14 Finally acute cholecystitis, as in our patient, is reported in three cases;11,15,16 only once gallstones also are described.16 Thus we believe that cholelithiasis represents a misleading element for the etiology of cholecystitis, more likely secondary to unusual localisation of amyloidois.
In literature surgery does not improve digestive symptoms and, conversely, is complicated in one case by bilioperitoneo,16 due to the fragility of bile channels. In our case, however, the non-specificity of clinical picture made it difficult to form a preoperative diagnosis, as often occurs.
The final consideration is related to diagnosis of amyloidosis, sometimes obtained through the biopsy of parenchymal organs, associated with high diagnostic value (sensitivity of trans-dermal core kidney biopsy, for example, is close to 100%),17 but there is a high risk of bleeding.17 Therefore the biopsy of subcutaneous fatty tissue is most practised (sensitivity 73%-78%, specificity 90%-93%, positive predictive value 84%, negative predictive value 90%),17 less frequently labial salivary glands biopsy (80-85% sensitivity), rectal biopsy (73% sensitivity), gingival mucosa biopsy (40-46 % sensitivity).17 However a negative result of a traditional diagnostic method (in our patient the first biopsy of subcutaneous fatty tissue and the rectal biopsy) may be due to multiple causes: different practice setting, level of experience, absence of abdominal soft tissue involvement.
In conclusion even if gallbladder localisation of amyloidosis is very unusual, however it is appropriate to think about this, especially in cases of outbreak of multiple myeloma as acute cholecystitis. Since clinical picture is not specific, laparoscopic cholecystectomy with gallbladder biopsy is often necessary to exclude additional pathologies, although associated with high risk of bleeding. Finally a negative result of traditional diagnostic methods in presence of highly suggestive clinical images still require further investigation.
AknowlegementsTo Dott Anna Rita Lombardi, Anatomical Pathology Institute, Infermi Hospital, Rimini (Italy).