Excessive intake of vitamin A may produce acute or chronic toxicity. Vitamin A can be consumed in foods, fortified products and supplements. We present a case of a young physical culturist man who was referred to our Unit because of chronic liver disease of unknown origin. The patient had a history of increased vitamin A intake from natural source with the addition of high dose of vitamin A supplements with the purpose of improving his muscular development. Our patient showed chronic liver disease with severe fibrosis, signs of portal hypertension and marked hyperplasia of Ito cells. In conclusion, chronic vitamin A toxicity may produce severe liver damage and should be recognized in the differential diagnosis of chronic liver diseases.
Abbreviations
ALT: alanine aminotransferases.
AST: aspartate aminotransferases.
HCV: hepatitis C virus.
HBV: hepatitis B virus.
HBc: hepatitis B core.
HBs: hepatitis B surface.
PAS: periodic acid Schiff’s.
IntroductionHigher organisms need Vitamin A to preserve normal cell growth and differentiation, the vision, immune response and reproduction.1 Nevertheless, excessive intake of vitamin A may produce acute or chronic toxicity. Vitamin A can be consumed in foods, fortified products and supplements. Consuming natural sources of this vitamin rarely results in chronic toxicity, with the exception of excessively high intake of carnivore liver on a continued basis.2,3 We present a case of chronic liver disease in a young physical culturist associated with increased vitamin A intake from natural source and supplements.
Case reportA 25 years old male patient was referred to our Liver Unit because of alanine (ALT) and aspartate aminotransferases (AST) elevations of more than 6 months length of unknown origin. He had no history of alcohol, illegal drugs or tobacco consumption, but he practiced physical culture and consumed a diet rich in meat and/or liver (more than 1,000 g per day). In order to improve his muscular development he used to supplement his food intake with high doses of vitamin A (220,000 IU/day) and consumed steroidal anabolic drugs. His physical examination disclosed a slightly enlarged spleen. The laboratory findings included increased levels of alkaline phosphatases (361 IU/L for a normal value up to 240 IU/L), AST (86 IU7L, normal value up to 40 IU/L), ALT (104 IU/L, normal value up to 40 IU/L) and y glutamyl transpeptidase (392 IU/L, normal value up to 50 IU/L). Viral markers for HCV and HIV were negative; auto-antibodies (anti nuclear, anti mitochondria, anti smooth muscle and anti liver-kidney-microsomes antibodies) were not found, and ferritin level was 406 ng/mL. The patient presented positive anti HBc and anti HBs antibodies. Ultrasound and Doppler duplex examination showed a normal liver structure, a portal vein with hepatopetal blood flow and an enlarged spleen.
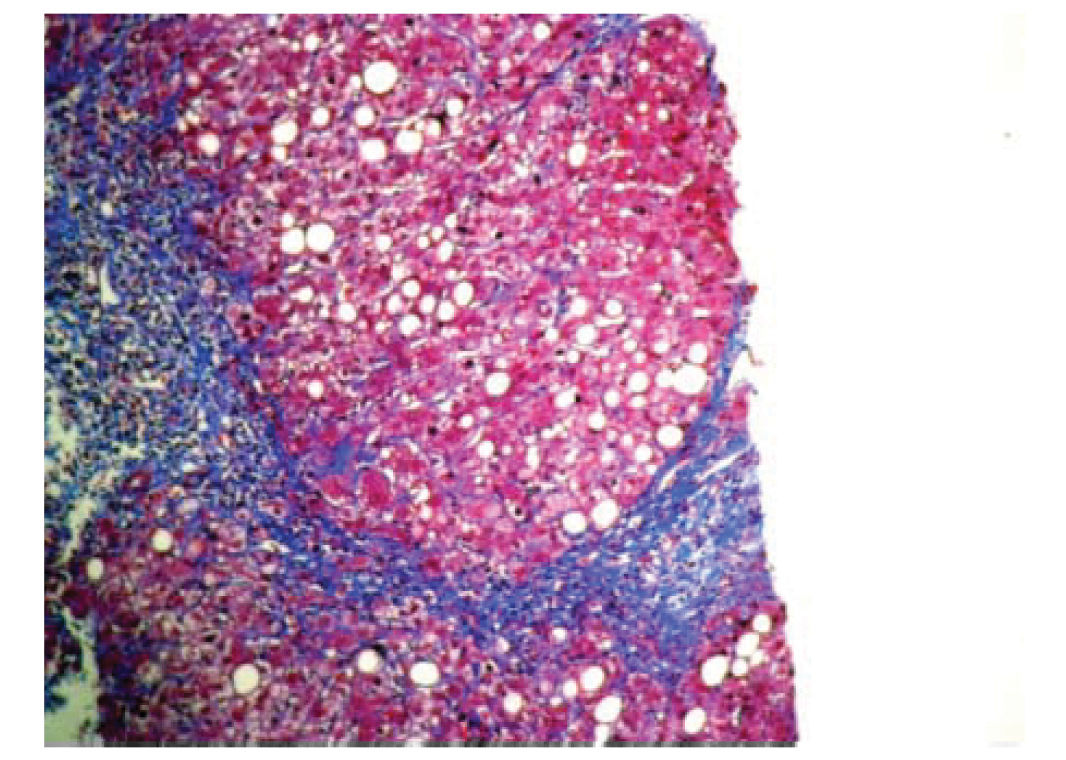
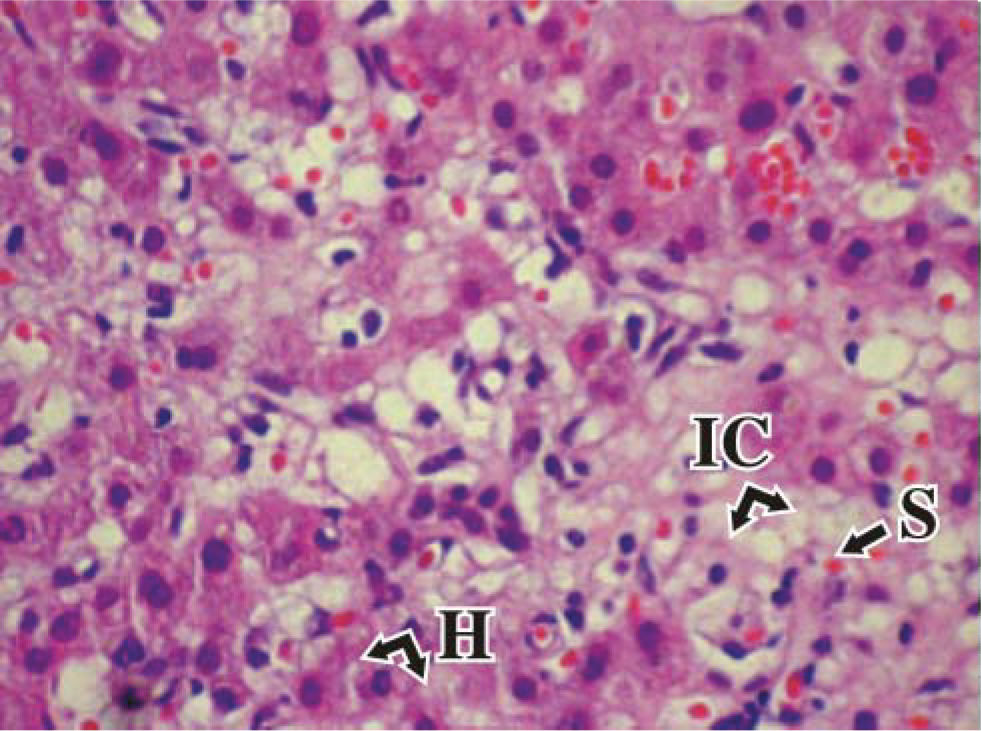
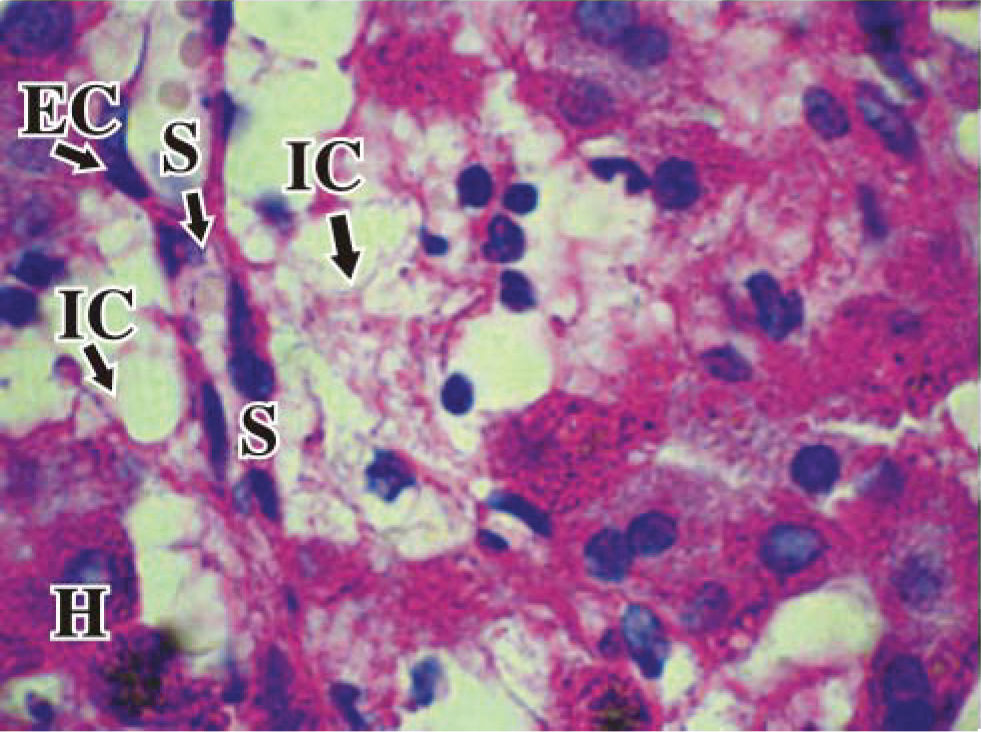
Ultrasound assisted liver biopsy was performed using modified Menghini needle of 1.4 mm diameter (Hepafix, Braun, Germany). Liver sample was fixed in 10% formaldehyde, embedded in paraffin and stained with hematoxylin and eosin, Masson’s trichrome, silver impregnation for reticular fibers, Perls blue and PAS. Histological liver specimen showed seven portal tracts with slight lymphocytic infiltrates and bridging fibrosis. In the lobuli, manifest hyperplasia of Ito cells, mild steatosis and regenerative changes of hepatocytes were observed (Figures 1and2).
Vitamin A was identified for nearly a century as an essential dietary constituent.4-6 The term vitamin A refers to a group of compounds, including retinol, retinaldehyde, and retinoic acid. Retinol may be obtained directly from foods of animal origin, mainly from liver, fish liver oils, eggs and cream, or be formed in the body from metabolism of ¡-carotene.7 Vegetables contain β-carotene and other provitamin carotenoids, which are absorbed and then partially converted to retinol in the enterocytes. Retinol is esterified and incorporated into chylomicrons, which are released into the lymph and later into the systemic circulation. Hepatocytes take up retinol esters from chylomicron remnants, and after hydrolysis, retinol is removed to the hepatic stellate cells or is oxidized and excreted to the bile.2 Within the hepatic stellate cells, retinol may either be stored as esters of long-chain fatty acids in rich lipid droplets in the cytoplasm or transferred to the plasma bound to retinol binding protein and prealbumin to peripheral target tissues.8,9 Nuclear hormone receptors like the peroxisome proliferator-activated receptors (PPA-Rα, β, and γ) are possibly involved in the control of retinol esterification and storage (10)- Near 90% of vitamin A reserve is stored in the liver; other sites of major vitamin A storage include the eye and the lung.7
In addition to vitamin A storage, hepatic stellate cells control the extracellular matrix turnover in the space of Disse and contribute to the control of sinusoidal blood flow.11 Acute and chronic liver injury activates hepatic stellate cells to undergo transition into myofibroblast-like cells.12 Activated hepatic stellate cells play a key role in the fibrotic response to liver injury by means of an enhanced proliferation and increased synthesis of extracellular matrix proteins,13 and are target for several antifibrotic therapies.14-16
Excessive ingestion of vitamin A may produce acute or chronic toxicity. It has been known since XIX century that the ingestion of polar bear and seal liver may be toxic for humans, and in 1943 this fact was associated to vitamin A toxicity.17,18
Acute toxicity in children and adults may produce nausea, vomiting, diarrhea, fever and increased intracranial pressure. High dose vitamin A supplements can cause teratogenic effects, particularly if consumed during the first trimester of pregnancy.2
Chronic vitamin A toxicity can occur in adults who commonly consume doses of 100,000 IU per day for months or years, about 40 times the recommended dietary allowance,2,19 and may result in severe liver disease.20
Histological abnormalities include perisinusoidal fibrosis and liver cirrhosis, correlating the severity of perisinusoidal fibrosis with the dose of vitamin A.21 Hypertrophy of Ito cells is usually present and may be the clue in the diagnosis.22 Unfortunately, the mechanisms involved in liver fibrosis induced by vitamin A are not clear.23 Although vitamin A administration may prevent hepatic stellate cells transition and CCl4-induced injuries in rat livers,24 it was recently described in humans the relationship between the amount of liver fibrosis and the quantity of activated hepatic stellate cells in cases of vitamin A toxicity.21
Alcohol abuse, viral hepatitis, some medications and the presence of other liver diseases may accelerate this liver damage, which can be fatal. In a large series of forty one patients with chronic vitamin A liver toxicity, cirrhosis was present in seventeen.25 Cirrhotic and non-cirrhotic portal hypertension with ascites and hydrothorax may be also present.25-29 Nonetheless, with early diagnosis reversal of the abnormalities can be obtained.29
Our patient showed chronic liver disease with severe fibrosis, signs of portal hypertension and marked hyperplasia of Ito cells. This pathological condition was associated with a history of increased vitamin A intake from natural source and supplements, although additional toxicity produced by anabolic intake could not be ruled out. Patients consuming vitamin A supplements should be aware of the toxic effect of vitamin A overdose, and physicians should recognize this entity in the differential diagnosis of chronic liver diseases.