Cirrhosis, a progressive and often irreversible liver condition, poses a significant and escalating global public health challenge. It is characterized by the formation of scar tissue in the liver, a consequence of various factors, including chronic alcohol consumption, viral hepatitis, metabolic dysfunction-associated steatotic liver disease/metabolic dysfunction-associated steatohepatitis (MASLD/MASH). Cirrhosis can lead to severe complications, including liver failure and hepatocellular carcinoma, contributing to over 2 million deaths annually, which accounts for approximately 4 % of total global mortality [1,2]. These conditions not only have a profound impact on individual health but also place a substantial burden on healthcare systems worldwide. In 2021 alone, cirrhosis was estimated to be responsible for a significant loss of 560.4 age-standardized disability-adjusted life years per 100,000 population [3,4].
Understanding the evolving landscape of cirrhosis incidence and prevalence is critical to addressing this growing health challenge. In recent years, the dominant risk factors have shifted. Historically, chronic hepatitis C and heavy alcohol consumption were the primary causes of cirrhosis but advances in treatment reduced the burden of chronic hepatitis C [5,6]. Instead, MASH has emerged as a leading cause, closely tied to rising obesity, diabetes, and metabolic syndrome worldwide [7]. In Canada, MASH is now a significant cause of cirrhosis, especially among postmenopausal females, and is projected to become the primary cause by 2040 [8]. While viral hepatitis incidence has declined in developed countries, alcohol consumption remains high, particularly among young adults. Alcohol-associated liver disease is a prominent concern, especially in younger populations [9]. These shifting trends emphasize the importance of ongoing efforts to prevent and manage cirrhosis. Since both alcohol-associated liver disease and MASH are preventable, early detection and management hold the potential to alleviate the burden of cirrhosis.
However, despite the pressing need for accurate and up-to-date data to address this evolving landscape, there remains a significant gap in the epidemiological estimates of cirrhosis over time. The lack of comprehensive data hinders our understanding of future mortality trends and healthcare needs for cirrhosis-related treatments such as liver transplantation, esophageal banding, and specialized care. This research sought to estimate cirrhosis incidence and prevalence in Manitoba from 2010 to 2019, shedding light on changes in cirrhosis rates across age groups and between males and females.
2Materials and methods2.1Data sourcesThis population-based study utilized administrative health care data from Manitoba, Canada, a province with a population of approximately 1.3 million individuals. Manitoba, like other Canadian provinces, operates a publicly funded healthcare system that systematically collects data for healthcare services on nearly the entire population. The data for this study were obtained from the Manitoba Population Research Data Repository housed at the Manitoba Centre of Health Policy in Canada. Importantly, these data are anonymized and possess the capability for individual-level linkage across databases and over time through the utilization of a scrambled Personal Health Identification Number derived from the Manitoba Health Insurance Registry (MHIR). Diagnoses were coded according to either the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) or the ICD 10th Revision, Canadian enhancement (ICD-10-CA) diagnosis codes [10].
We linked three anonymized databases in this study: hospital discharge abstracts, physician billing claims, and MHIR. The Discharge Abstract Database captures diagnosis and procedure codes recorded at the point of discharge from acute-care facilities. It provides a comprehensive overview of healthcare services rendered to patients in these settings. The Medical Claims Database captures physician billings for both in-hospital and outpatient visits (each claim contains a single ICD-9-CM diagnosis code). The MHIR encompasses a comprehensive record of all individuals registered with the provincial health insurance plan and comprises information about dates of health insurance coverage, reasons for termination of health insurance coverage, and demographic attributes such as age, sex, and residence location (postal code) for each resident. In addition, Statistics Census data from 2011 and 2016 were used to define household income quintile, an area-level measure of socioeconomic status. The integrity and reliability of administrative health care data within the Manitoba Population Health Data Repository have been rigorously validated and documented in previous studies [11,12].
2.2Study populationThe study population consisted of individuals 18 years of age or older who registered in the MHIR for at least five years between Jan 1, 2005, and Dec 31, 2019.
2.3Measuring cirrhosisWe applied two previously validated case-ascertainment algorithms in our study population to identify cirrhosis cases [13,14]; Algorithm 1 required at least one hospitalization or at least two physician claims, and Algorithm 2 required at least one hospitalization or physician claim for cirrhosis (Supplemental file for relevant diagnosis and procedure codes). The estimates of sensitivity and specificity of the algorithms when compared to a reference standard of validated primary care case definition ranged from 43-68 % and 96-97 %, respectively, using longitudinal data from 1998 to 2020 [14].
2.4Statistical analysisBaseline demographic and clinical characteristics of the incident cirrhosis population are presented as frequencies, percentage and mean (standard deviations; SD), as appropriate.
2.4.1Annual incidence and prevalence ratesThe crude and age- and sex- adjusted annual incidence, and prevalence rates were estimated (with corresponding 95 % confidence intervals [95 % CIs]) by dividing the number of individuals aged ≥18 years classified as having cirrhosis by the number of eligible Manitobans in the study population on July 1 of each calendar year for both ascertainment algorithms. To establish incidence, we used a five-year look back window to confirm the individual had not received any health services for cirrhosis previously and calculated annual incidence from January 2010 onward. Individuals with prior health services utilization for cirrhosis in these years were counted as prevalent until they left the province, died, or reached the end of the study (December 2019). This five-year washout period has been used previously in cirrhosis studies based on administrative health data [15].
2.4.2Time Trend AnalysisChanges in incidence and prevalence rates were tested using generalized linear models with generalized estimating equations, in order to account for correlation in the data [16]. A negative binomial distribution was selected to model cirrhosis rates, as the dependent variable [17]. In all the models, we adjusted for year (continuous variable), age group (ordinal variable: (18-44, 45-64 and 65+ years), and sex (categorical variable), with the natural algorithm of the Manitoba population as the model offset. We considered a model to have a good fit to the data when the ratio of the deviance to the degrees was close to 1.
If a time trend was observed, the rates of change in incidence and prevalence were analyzed by replacing the set of categorical variables for the calendar year with a continuous variable defined as time (in years). The terms of the age group variable multiplied by the time variable and sex variable multiplied by the time variable were added as covariates to examine the effects of the interaction between age group and time, and sex and time, to test whether the rates of change over time in incidence and prevalence differed across age groups and between males and females. A statistically significant interaction between time and a given age group; time and sex indicated that the rate of change in incidence/ prevalence differed over time compared with the reference age group (18-44 years) and sex (female). A nominal α =0.05 was adopted for all tests of statistical significance. SAS version 9.4 (SAS Institute, Cary, NC, US) with the GENMOD procedure was used for all analyses.
2.5CovariatesCalendar year, sex, age group, income quintile, Charlson comorbidity Index scores, and geographic residence location (Winnipeg/urban and non-Winnipeg/rural) were defined at the study index date. Age at the index cirrhosis diagnosis was classified as 18-29, 30-49, 50-59, 60-69 and 70-79 and 80+ years. Income quintile is an area-level measure of socioeconomic status defined using Statistics Canada Census data and based on total household income for dissemination areas, the smallest geographic unit for which Census data are publicly released [18]. Postal codes from the MHIR were used to assign individuals to income quintiles based on their geographic residence location. We captured the presence of comorbidities using the Charlson Comorbidity Index [19] from hospital discharge abstract and physician billing claims [20] with a 1-year look back window prior to the cirrhosis index date. Liver disease was excluded from the Charlson Comorbidity Index, whereas liver cancer was counted as comorbid cancer. The Index score was defined as a categorical variable with values of 0, 1-2 and 3+ representing absent, mild and moderate/severe comorbidities.
2.6Ethical statementThis study involved human participants and was approved by the University of Manitoba, Human Research Ethics Board: No. HS25263 (H2021:406). The Manitoba Government's Health Information Privacy Committee (HIPC No. 2021/2022-26) waived the requirement for individual informed consent on the basis that the study used de-identified administrative data, none of the participants were directly involved in the study, and there was low risk of any individual being personally identified.
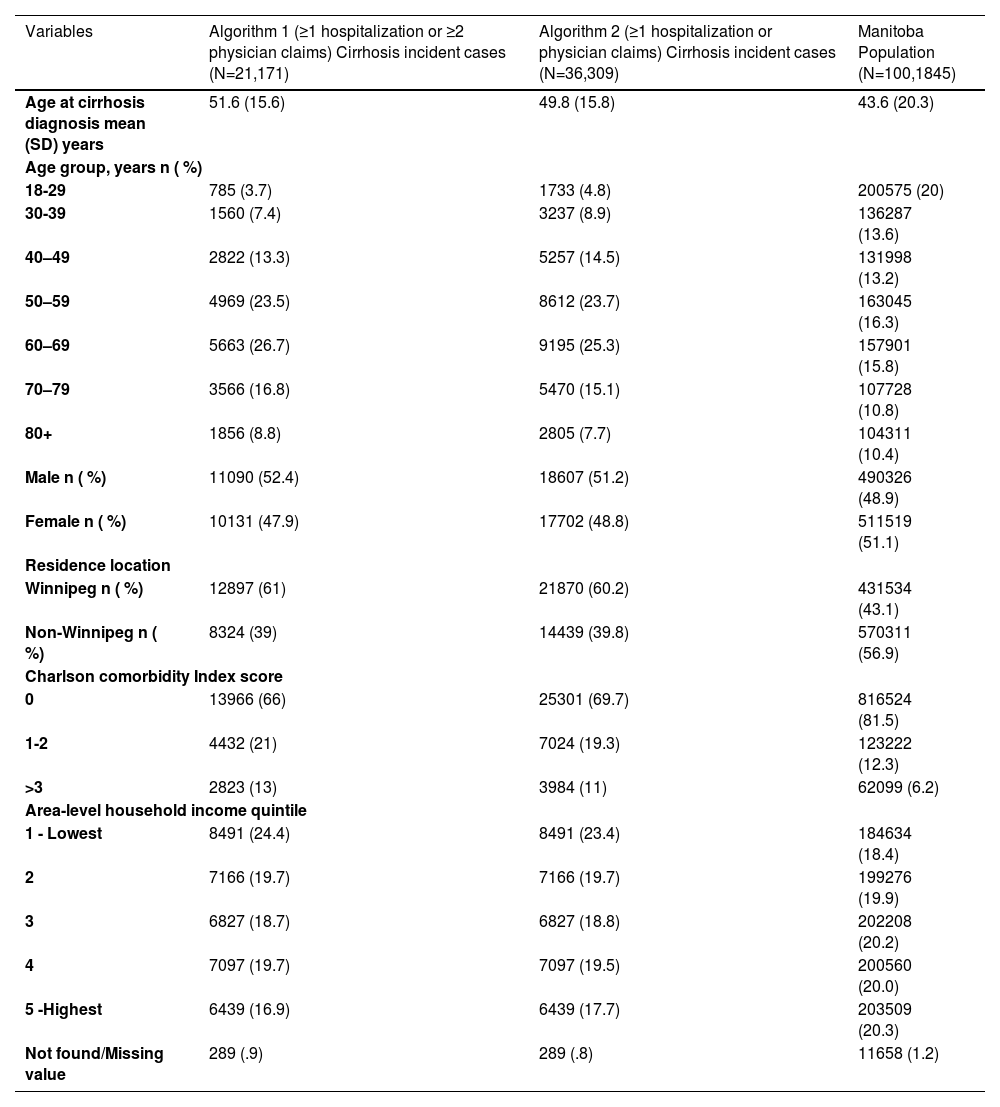
3Results3.1Incidence and prevalence of cirrhosisFrom 2010 to 2019, we identified 21,101 incident cases of cirrhosis with algorithm 1 (defined as having either ≥1 hospitalization or ≥2 physician claims) and 36,309 cases with algorithm 2 (defined as having either ≥1 hospitalization or ≥1 physician claim) in Manitoba. Among these cases, 52 % were male, with a mean age of 50 years at the time of diagnosis. Table 1 presents the baseline characteristics of the entire cohort. Approximately 60 % of incident cases resided in Winnipeg, and over 40 % of individuals with cirrhosis were categorized to the bottom two income quintiles. Regardless of the algorithm used for case identification, the distribution of sex, age, Charlson comorbidity index, and income quintiles among people with cirrhosis remained similar.
Demographic characteristics at diagnosis index date for incident cases of cirrhosis from 2010 to 2019 and for the Manitoba population aged 18+
SD = standard deviation.
In 2019, we observed an overall crude estimated incidence of 202 (95 % CI 187.8-216.3) per 100,000 population and crude estimated prevalence of 1.9 % (95 % CI 1.6-2.6) using algorithm 1 (≥1 hospitalization or ≥2 physician claims). In contrast, algorithm 2 (≥1 hospitalization or ≥1 physician claim) yielded an overall crude estimated incidence rate of 411.8 (95 % CI 369.9-453.7) per 100,000 population and a crude estimated prevalence rate of 3.6 % (95 % CI 3.0-4.2). Additionally, the proportion of incident cases that were female increased from 46 % in 2010 to 50 % in 2019 when using algorithm 1 and from 47 % in 2010 to 51 % in 2019 when using algorithm 2.
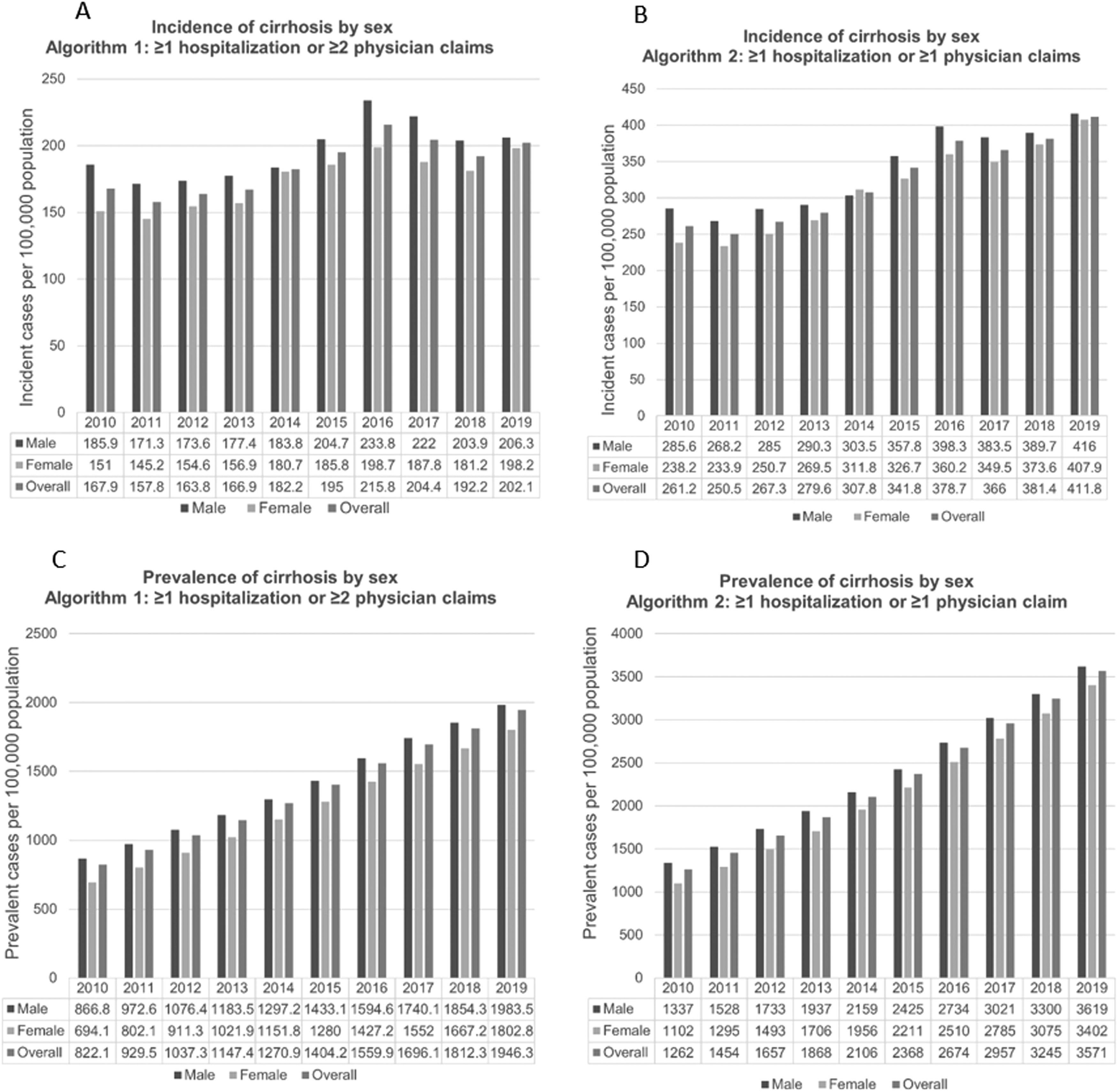
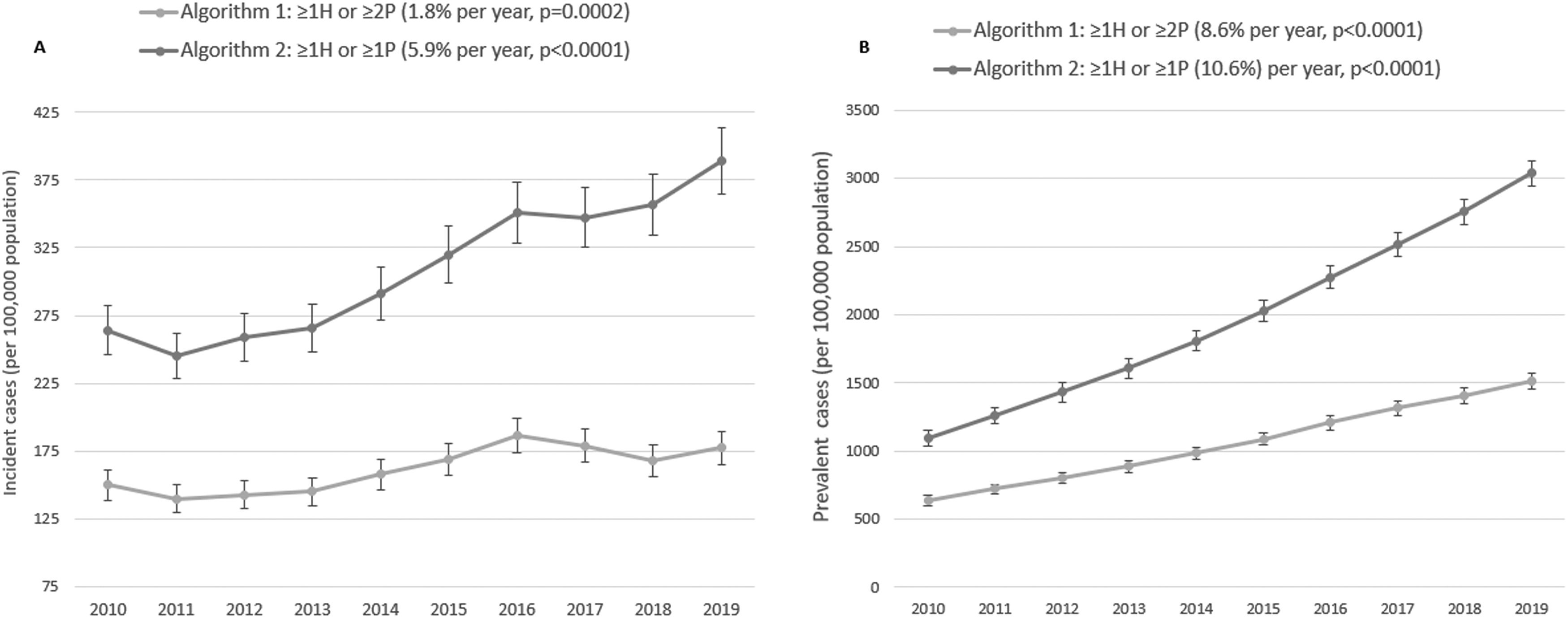
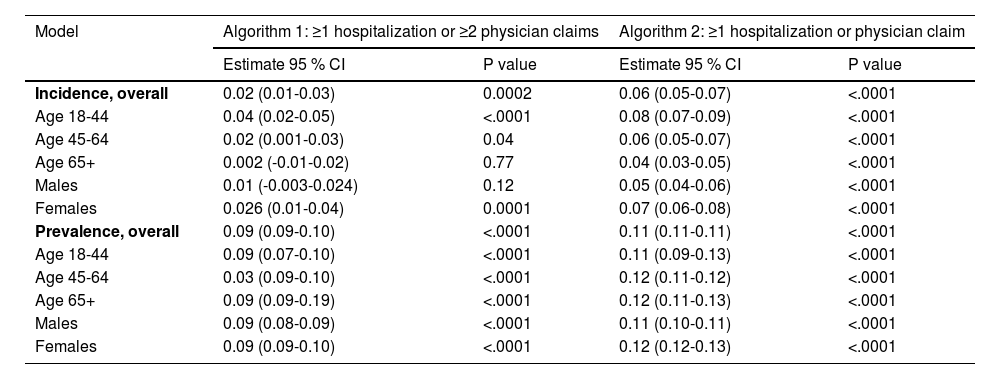
3.2Temporal trends for cirrhosisBetween 2010 to 2019 crude cirrhosis incidence estimates increased by 20 % when using algorithm 1 (≥1 hospitalization or ≥2 physician claims) and 58 % when using algorithm 2 (≥1 hospitalization or ≥1physician claim) (Fig. 1). The age- and sex- adjusted estimated incidence rates showed a gradual increase over this period for both algorithms. Specifically, the adjusted rates per 100,000 population were as follows: for Algorithm 1, 149.7 (95 % CI 139.3-160.9) in 2010 and 177.2 (95 % CI 165.5-189.8) in 2019; for Algorithm 2, 264 (95 % CI 246.6-282.6) in 2010 and 388.8 (95 % CI 365.0-414.1) in 2019 (Fig. 2). On average, the estimated incidence increased by 2 % per year (95 % CI 1 % to 3 %, P = 0.0002 for linear trend) when using algorithm 1, and by 6 % per year (95 % CI 5 % to 7 %, P <.0001 for linear trend) when using algorithm 2, between 2010 and 2019 (Table 2).
Estimated incidence (A and B) and prevalence (C and D) of cirrhosis per 100,000 population overall and by sex from 2010 to 2019 for algorithm 1: ≥1 hospitalization or ≥2 physician claims and algorithm 2: ≥1 hospitalization or ≥1 physician claim.
Estimates for annual rate of change of cirrhosis incidence and prevalence from 2010 to 2019*.
Over the same ten-year span (2010-2019), the estimated prevalence rate increased by 2.4-fold when using algorithm 1 and 2.8-fold when using algorithm 2 (Supplemental Fig. 2). Estimated prevalence rates increased on average by 9 % per year (95 % CI 9 % to 10 %, P <.0001 linear trend) with algorithm 1 and by 11 % per year (95 % CI 11 % to 12 %, P <.0001 linear trend) with algorithm 2 (Table 2).
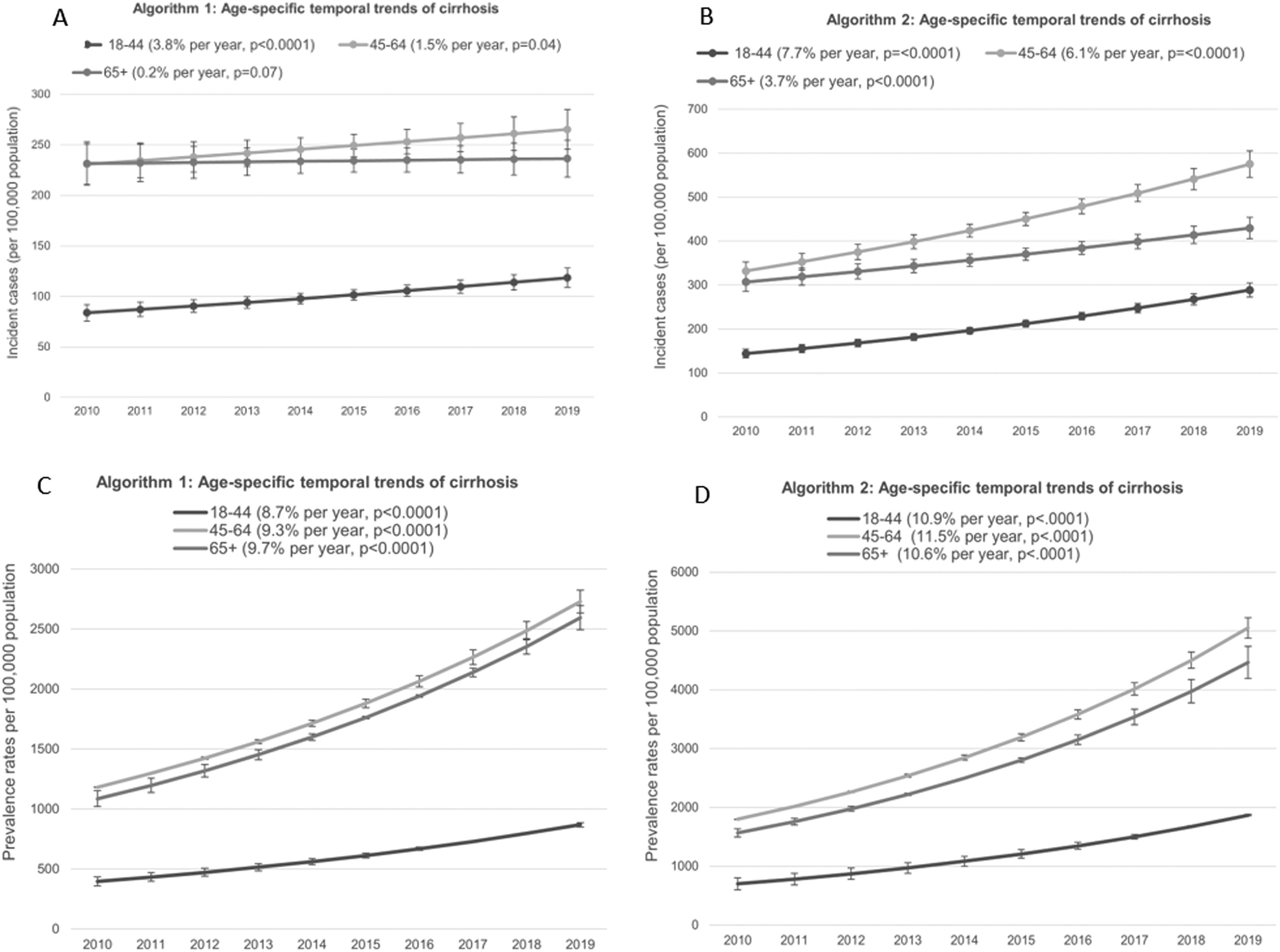
3.3Age-specific temporal trends for cirrhosisThe temporal trends in age-specific and sex-adjusted cirrhosis incidence and prevalence estimates are shown in Fig. 3. Overall, the highest incidence rates were observed among individuals aged 45-64 for both algorithms between 2010 and 2019.
Age-specific temporal trends of cirrhosis incidence (A and B) and prevalence (C and D) per 100,000 population for Algorithm 1: ≥1 hospitalization or ≥2 physician claims and Algorithm 2: ≥1 hospitalization or ≥1 physician claim (2010-2019)
For algorithm 1 (≥1 hospitalization or ≥2 physician claims), the incidence increased by an average of 4 % per year (95 % CI 2 % to 5 %, p <.0001) among individuals aged 18–44 and by 2 % per year (95 % CI 0.1 % to 3 %, p = 0.04) among those aged 45–64, but there was no significant change in incidence among individuals aged 65 and over (0.2 %, 95 % CI .1 % to 2 %, p = 0.76). Conversely, with algorithm 2 (≥1 hospitalization or ≥1physician claim), incidence of cirrhosis increased across all age groups, with the greatest average increase observed in the youngest category [18-44]: 8 % per year (95 % CI 7 % to 9 %, p <0.0001); 45-64: 6 % per year (95 % CI 5 % to 7 %, p <0.0001) and 65+: 4 % per year (95 % CI 3 % to 5 %, p <0.0001). The rate of change in the incidence of cirrhosis was highest among the youngest age group [18-44] for both algorithms. Estimated prevalence exhibited a consistent increase across all age groups for both algorithms, with an annual growth rate ranging from 9 % to 11 %. Notably, the rate of change in prevalence remained similar across age groups over time.
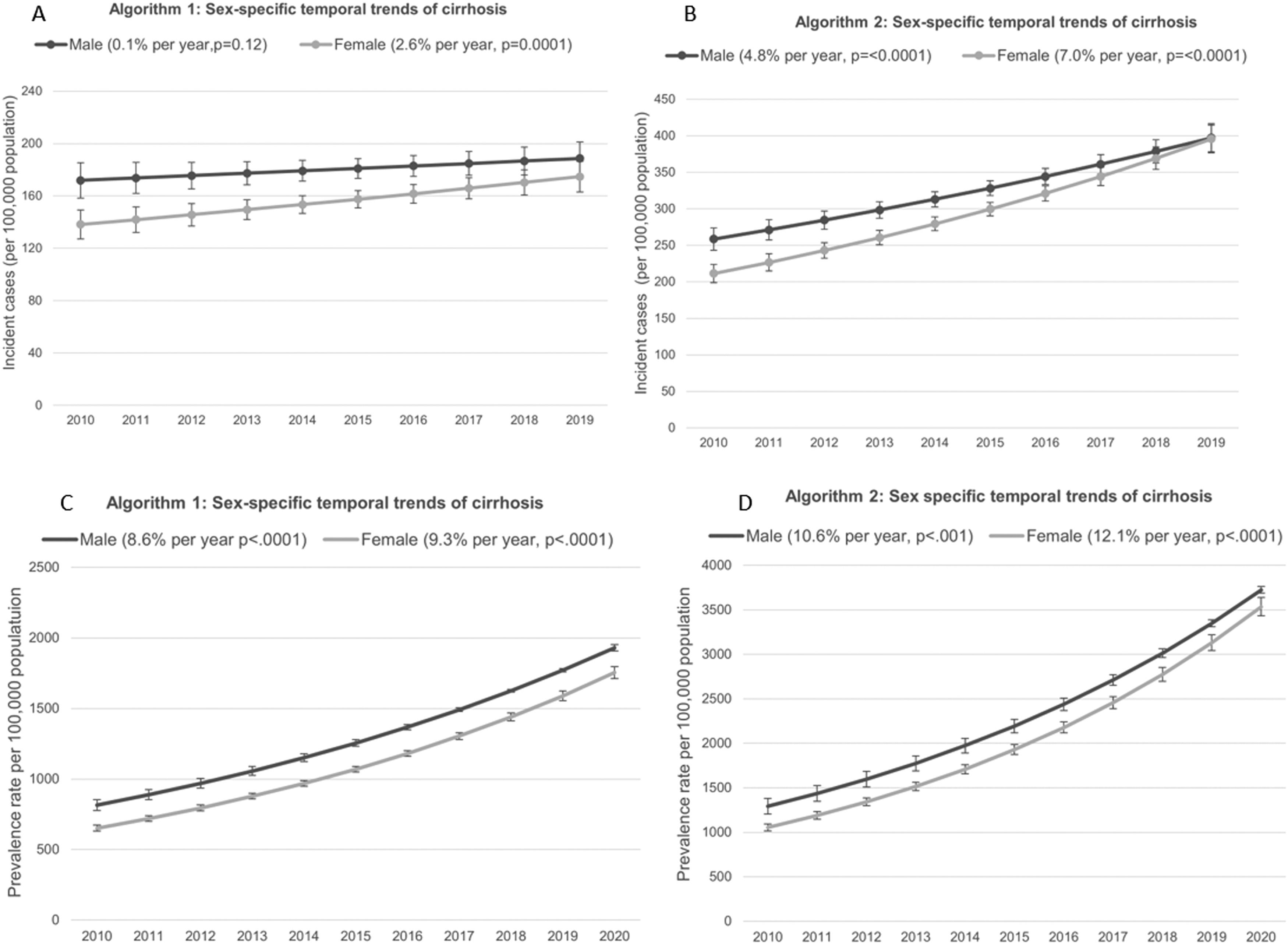
3.4Sex-specific temporal trends for cirrhosisThe temporal trends in sex-specific and age-adjusted cirrhosis incidence and prevalence are displayed in Fig. 4. Among females, both incidence and prevalence rates showed a statistically significant increase over time when using both algorithms. In contrast, among males, the increase in rates was only observed when using algorithm 2 (≥1 hospitalization or ≥1physician claim) (Table 2). Specifically, females experienced a more pronounced average annual increase of 7 % (95 % CI 5 % to 8 %, p< 0.0001) compared to males when using algorithm 2, who also saw an increase, albeit at a slightly lower rate of 5 % per year (95 % CI 4 % to 6 %, P < 0.0001) between 2010 and 2019. Furthermore, females exhibited a significantly higher rate of change in cirrhosis incidence compared to males (P=0.0025). Estimated prevalence increased among both sexes, but females demonstrated a higher rate of change in prevalence estimates of cirrhosis between 2010 and 2019 compared to males for both algorithms.
Sex-specific temporal trends of cirrhosis incidence (A and B) and prevalence (C and D) per 100,000 population for Algorithm 1: ≥1 hospitalization or ≥2 physician claims and Algorithm 2: ≥1 hospitalization or ≥1 physician claim (2010-2019)
In this retrospective population-based study conducted in Manitoba, Canada, we observed a significant increase in the incidence of cirrhosis over the study period. While the highest estimated incidence rates were observed among middle-aged populations, it is particularly concerning that the younger age category (18-44 years) experienced the most substantial rise in cirrhosis incidence from 2010 to 2019. Furthermore, our analysis illuminated a steady increase in cirrhosis incidence among females, now surpassing the rates observed among males. These findings signal a troubling shift in the burden of cirrhosis, affecting younger individuals and females at an increasing rate. These trends are likely driven by heavy alcohol consumption and escalating rates of obesity, underscoring the pressing need for preventive measures. In 2019, we identified 649 incident cases likely attributed to ALD-associated cirrhosis using ICD codes for alcohol-related conditions. These cases accounted for approximately 20 % of all new cirrhosis cases identified by algorithm 2.
The findings of this study highlight the ongoing and significant disease burden imposed by cirrhosis, which not only strains the healthcare system but also carries substantial socio-economic implications. The disproportionate impact on young and middle-aged individuals, who are in their prime working years, may lead to considerable disruptions in employment, productivity, and income due to cirrhosis-related health issues. Consequently, this translates into an increased burden of disease-adjusted life years. Our study underscores the urgency of directing more targeted efforts towards cirrhosis and serves as a clear alarm for the healthcare system.
It is noteworthy that the rates of cirrhosis in Manitoba appear to be higher than those reported in other population-based studies conducted in Ontario [15], the United States [21], and Europe [22]. These discrepancies may be due to several factors, including differences in population demographics, healthcare access, screening practices, and regional variations in risk factors and healthcare resources. Notably, Manitoba exhibits elevated rates of cirrhosis risk factors, including obesity, metabolic syndrome, and alcohol consumption [23,24].
Our study is consistent with recent research that has also reported a higher incidence of cirrhosis among young adults and females in North America and other regions where risk factors such as metabolic syndrome and alcohol misuse are increasing [9,15,25]. These epidemiological trends likely reflect a lack of early diagnosis of alcohol liver disease and MASH, as well as the scarcity of effective therapies for halting disease progression. The projected burden of MASH further exacerbates the strain on the healthcare system, emphasizing the urgent need for preventive measures. Heightened awareness and education among patients and healthcare providers is imperative, focusing on the consequences of unhealthy alcohol consumption, the importance of regular screening for alcohol use disorder and MASH in primary care settings, and the timely implementation of prevention and intervention strategies to alleviate the growing burden on healthcare resources.
4.1Strength and limitationsThe strengths of our study encompass the utilization of administrative health data, representing the entire Manitoba population over 15 years, allowing for a robust assessment of temporal trends. Additionally, we provided cirrhosis incidence and prevalence estimates using two case-defining algorithms, each likely capturing individuals at different stages of the disease course. One algorithm identified individuals at a later stage of the disease with two physician visits, while the other identified people in an early disease course with only one physician visit. We acknowledge the inherent limitations of administrative health databases, including the potential for misclassification bias [26]. To mitigate this bias, we captured patients only if they had physician claims or hospitalizations with ICD-9 or ICD-10 diagnosis codes for cirrhosis, which have been previously shown to be reliable and accurate [13,27]. While the algorithms used in the study exhibited modest sensitivity and high specificity when compared with diagnoses captured in primary care electronic medical records, they showed higher sensitivity and accuracy when compared with hepatology patients’ medical records [13]. These algorithms offer valuable insights for different purposes in estimating disease burden and healthcare planning. Challenges remain in defining the date of disease onset in administrative health data, and it is possible that prevalent asymptomatic cirrhosis cases that rarely interacted with the medical system were misclassified as incident cases. Additionally, stigma associated with cirrhosis can significantly impact healthcare access and utilization, particularly among lower-income populations. Despite Canada's universal healthcare system, socioeconomic disparities may contribute to underreporting and underdiagnosis, potentially leading to an underestimation of the true disease burden. This issue and the potential for selection bias must be acknowledged.
5ConclusionsThis population-based study highlights the temporal trends in cirrhosis, characterized by rising incidence and prevalence estimates, particularly among young adults and females. The notable acceleration in cirrhosis among females compared to males underscores the urgency for further research to identify contributing risk factors. These findings emphasize the imperative for healthcare planning and interventions to curb the increasing burden of cirrhosis in these demographics.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contributionsNF, LML, AS, HS, ER, and AM participated in the study concept, design, and interpretation. NF, LK and RW contributed to data acquisition and analysis. NF drafted the manuscript. LML, RW, AS, LK, ER, and HS and AM contributed to critical revision of the manuscript for important intellectual content.
Data availability statementThe data that support the findings of this study are not publicly available, in accordance with site-specific privacy restrictions. The data that support the findings of this study are from the Manitoba Population Research Data Repository housed at the Manitoba Centre for Health Policy, University of Manitoba, and were derived from data provided by Manitoba Health and the Winnipeg Regional Health Authority. Data are available, with submission of appropriate ethics and data access approvals, from the Manitoba Centre for Health Policy.
The authors acknowledge the Manitoba Centre for Health Policy for use of data contained in the Manitoba Population Research Data Repository under HIPC project # 2021/2022-2. The results, conclusions, opinions, and statements expressed are solely those of the authors and no official endorsement by the Manitoba Centre for Health Policy, Manitoba Health, or Health Information Privacy Committee/Provincial Health Research Privacy Committee is intended or should be inferred.