Interpersonal stress factors contribute to common mental health problems measured as anxiety and depression. Recently, it is emerging that anxiety precedes depression but not the reverse, and markedly increase in response to stress giving way to depression. As such, anxiety itself could be a predictive risk factor, and mediate the associations between stress and depression. While resilience protects against exposure to stress and common mental health problems, it is unclear to what extent different resilience factors are differentially involved in protection against anxiety and depressive symptoms. This study explored complex theoretical associations between interpersonal stress, anxiety and depressive symptoms and resilience factors.
Materials and methodsParticipants (N=210 adults) completed the Resilience Scale for Adults (RSA), Patient Health Questionnaire (PHQ-9), Generalized Anxiety Disorder Questionnaire (GAD-7) and the Stressful Life Events Questionnaire (SLE) in a cross-sectional survey. Hierarchical linear regressions and moderated-mediation analyses were performed using PROCESS macro.
ResultsInterpersonal stress explained more variance in depressive than anxiety symptoms. Support was found for the mediating effect of anxiety symptoms in the relationship between interpersonal stress and depressive symptoms. Resilience factors are differentially involved in protection against anxiety and depressive symptoms.
ConclusionExposure to interpersonal stress is not only directly associated with depressive symptoms but also indirectly through high scores on anxiety symptoms. Uneven functioning and differential impact of resilience factors can help us understand the mixed successes in implementing resilience-based interventions for positive mental health and judiciously allocate scarce and finite resources for intervention.
Los factores de estrés interpersonal contribuyen a problemas comunes de salud mental como ansiedad y depresión. Recientemente, se está demostrando que la ansiedad precede a la depresión, pero no al revés, y que aumenta notablemente en respuesta al estrés dando paso a la depresión. Como tal, la ansiedad en sí misma podría ser un factor de riesgo predictivo y mediar las asociaciones entre el estrés y la depresión. Si bien la resiliencia protege contra la exposición al estrés y los problemas comunes de salud mental, no está claro en qué medida los diferentes factores de resiliencia están involucrados de manera específica en la protección contra la ansiedad y los síntomas depresivos. Este estudio exploró asociaciones teóricas complejas entre estrés interpersonal, ansiedad, síntomas depresivos y factores de resiliencia.
Instrumentos y MétodoLos participantes (N = 210 adultos) completaron la Escala de Resiliencia para Adultos (RSA), el Cuestionario de Salud del Paciente (PHQ-9), el Cuestionario de Trastorno de Ansiedad Generalizada (GAD-7) y el Cuestionario de Eventos Vitales Estresantes (SLE) en una encuesta transversal. Se realizaron regresiones lineales jerárquicas y análisis de mediación moderada utilizando PROCESS.
ResultadosEl estrés interpersonal explicó más variaciones en los síntomas depresivos que en los de ansiedad. Se pudo demostrar el efecto mediador de los síntomas de ansiedad en la relación entre el estrés interpersonal y los síntomas depresivos. Los factores de resiliencia intervienen de manera diferencial en la protección contra la ansiedad y los síntomas depresivos.
ConclusionesLa exposición al estrés interpersonal no solo se asocia directamente con los síntomas depresivos, sino también indirectamente, a través de puntuaciones altas en los síntomas de ansiedad. El funcionamiento desigual y el impacto diferencial de los factores de resiliencia pueden ayudarnos a comprender los resultados mixtos obtenidos en la implementación de intervenciones basadas en resiliencia para la salud mental positiva, y asignar juiciosamente los recursos escasos y finitos para la intervención.
Palabras clave
Exposure to interpersonal stress is implicated in undermining interpersonal functioning, which may lead to disappointment and development of common mental health problems such as depression (Ingram & Luxton, 2005; Vrshek-Schallhorn et al., 2015). General anxiety is characterized by uncontrollable worry, apprehensions, and tensions in response to stress that precedes or gives way to depression, making anxiety itself a risk factor for the development of depression (Higa-McMilla, Francis, & Chorpita, 2014). In addition, other researchers have long ago documented the direct relation between interpersonal stress and depression (Grant & McMahon, 2005; Ingram & Luxton, 2005). Recently, it is emerging that in the context of anxiety and depression, anxiety symptoms markedly increase in response to stress and predict depression (Higa-McMilla et al., 2014). This may explain an indirect pathway between interpersonal stress and depression, making anxiety symptoms a mediating variable. However, conceptual mechanisms that underlie these associations are underexplored as only few studies (Anyan, Worsley, & Hjemdal, 2017; Kok et al., 2016) have explored the mediating role of anxiety symptoms between stress and depression. Kok et al. (2016) found that trait anxiety was an important mediating variable of postoperative posttraumatic stress disorder (PTSD) and depression. Anyan et al. (2017) found that transient/state anxiety mediated the relation between eight of ten stressor dimensions and depressive symptoms. In the current study, a complex theoretical model that explores both mediating (i.e., anxiety symptoms) and moderating (i.e., resilience factors) variables in the association between interpersonal stress and symptoms of depression was tested.
Resilience has been defined as the capacity to overcome adversities leading to positive adaptation and growth despite ongoing negative stressful experiences, thus providing protection against common mental health problems such as anxiety and depression related to stress (Anyan, Bizumic, & Hjemdal, 2018; Anyan & Hjemdal, 2016; Anyan et al., 2017; Hjemdal, Friborg, Stiles, Rosenvinge, & Martinussen, 2006). An emerging problem in recent theoretical and empirical writings is the tendency to emphasize that all resilience factors equally contribute and shape resilience processes and outcomes, failing to show (any, if they exist) uneven impacts among the different factors (Theron & Ungar, 2018). Evidence for the uneven impact of different resilience factors comes to bare when an individual can show resilience based on a particular protective factor in overcoming adversity, but this same individual may not show the requisite competence to succeed when facing other risks or adversities, therefore, requiring a different resilience factor to succeed (Luthar, Cicchetti, & Becker, 2000). Additionally, depending on the nature and severity of adversity, some protective factors may not be adequate to yield resilience (Theron & Ungar, 2018). Operationalizing resilience as a unitary construct may obscure important differences and subtle variations in the unique contributions and impacts of individual resilience factors involved in the protection against common mental health problems. The current study also answers a differential impact question by investigating how resilience protective factors are differentially involved in protection against depressive symptoms associated with interpersonal stress.
Exposure to interpersonal stress and mental health problemsInterpersonal factors can be either vulnerability (when maladaptive) or protective (when supportive) factors against depression (Orden, Wingate, Gordon, & Joiner, 2005). While interpersonal relationships can contribute to social-behavioural gains, they can also foster social-behavioural deficits by undermining interpersonal functioning, which may lead to disappointment and development of depression (Ingram & Luxton, 2005). Chronic interpersonal stress and major interpersonal stressful life events are unique predictors for major depressive onsets over other non-interpersonal forms of stress (Vrshek-Schallhorn et al., 2015). Interpersonal chronic stress also mediated the effect of childhood adversity on later depression (Vrshek-Schallhorn et al., 2015). These findings highlight the impact of interpersonal stress on mental health.
Relationship between resilience factors and mental healthIn the current study, resilience factors were derived from the Resilience Scale for Adults (RSA; Hjemdal, Friborg, Martinussen, & Rosenvinge, 2001). The RSA, which is counted as one of the best in a metholodigcal review of resilience measurement scales (Windle, Bennett, & Noyes, 2011), operationalizes six protective factors of resilience based on the three overaching dimensions of the resilience construct (Hjemdal et al., 2001). These are (i) internal positive dispositions, capacities and strengths, (ii) positive family environments, and (iii) external social support systems outside the family (Infurna & Luthar, 2017; Rutter, 2006). Protective factors in the RSA comprise four personal factors (perception of self, planned future, social competence and structured style), one family factor (family cohesion), and one external social factor (social resources).
Perception of self (PS) assesses a basic trust or confidence in one's own ability to solve, manage or cope well with adverse life events. Belief in one's self and one's own resources to get through difficult periods in life plays an important role when facing stress. By elevating one's self-esteem, it can in turn serve as an important protective factor for how well an individual adjusts to psychological adversities (Tetzner, Becker, & Baumert, 2016). Planned future (PF) assesses a positive outlook on one's own future, a preference for making plans and formulate clear future goals. Research has shown that the ability to make plans and concentrate on what to do next is negatively associated with depression (Standardized: β=−.29, p<.01), and state anxiety (β=−.28, p<.05) (Catz, Gore-Felton, & McClure, 2002). Structured style (SS) involves goal orientedness and planning ability, organization of own time and routine (Hjemdal et al., 2001). Individuals with these attributes are often more persistent in the face of challenges and engage more in active coping with psychological adversity.
Social competence (SC) asks for the ability to engage socially and create new friendships, feel at ease in social settings and being flexible in social interactions. Difficulty in engaging socially thwarts a need to belong, which may play a role in the development and maintenance of mental health problems (Van Orden, Wingate, Gordon, & Joiner, 2005). In a 2-wave panel study, difficulty in social skills and engagement was found to be a vulnerability for psychosocial problems, and poor social skills were related to depression and anxiety (Segrin & Flora, 2000). Social resources (SR) entails social support, presence of important persons outside family, encouragement and appreciation by people in one's social networks, and opportunities for getting help when needed (Hjemdal et al., 2001). Family cohesion (FC) assesses shared familial values, family loyalty, and mutual appreciation. Previous studies have favoured a stable and supportive family home environment marked by coherence in family relationships and significant emotional bonding as a protective factor. Family disruptions can interfere in adaptive interpersonal behaviours, increasing the risk for subsequent mental health problems (Hjemdal et al., 2001; Hjemdal, Friborg, Stiles, Martinussen, & Rosenvinge, 2006).
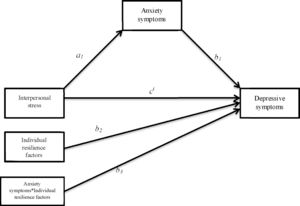
The current studyThe current study explored a conceptual model of the underlying mechanisms between interpersonal stress and depressive symptoms. This model included both mediating (i.e., anxiety symptoms) and moderating (i.e., individual resilience factors) variables. Positive associations were expected among interpersonal stress, anxiety and depressive symptoms. Anxiety was also expected to mediate the association between interpersonal stress and depressive symptoms (Anyan et al., 2017; Higa-McMilla et al., 2014; Kok et al., 2016).
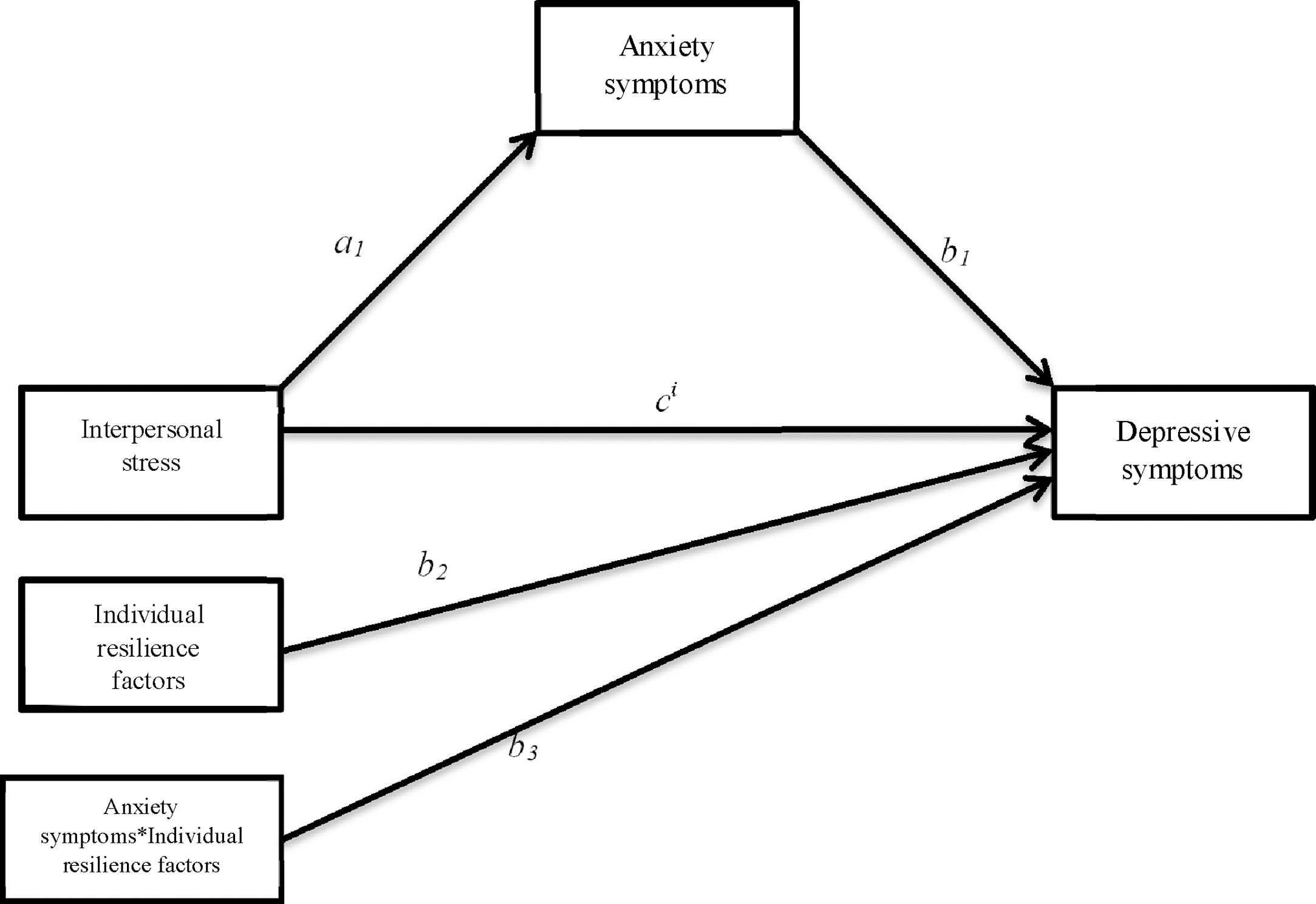
Individual resilience factors were hypothesized to be negatively associated with interpersonal stress, anxiety and depressive symptoms. The resilience factors were individually expected to moderate the mediated associations between interpersonal stress, anxiety and depressive symptoms. More specifically, it was hypothesized that the mediated effect of anxiety symptoms between interpersonal stress and depressive symptoms would be most strongly associated with adults with lower levels of resilience protective factors as compared with adults with higher levels of resilience protective factors (Anyan et al., 2018; Anyan & Hjemdal, 2016; Hjemdal, Friborg, Stiles, Rosenvinge, et al., 2006). The complete statistical model is presented in Fig. 1.
Moderated mediation model displayed in statistical form for interpersonal stress as the focal predictor, anxiety symptoms as mediator variable, depressive symptoms as outcome variable and individual resilience factors as moderator variables. Note: a1=Direct relation of interpersonal stress and anxiety symptoms. b1=Direct relation of anxiety symptoms and depressive symptoms. c1=Direct relations of interpersonal stress and depressive symptoms, controlling for anxiety symptoms. b1+b3*Resilience factors=Conditional relations of anxiety symptoms on depressive symptoms (i.e. moderated by separate resilience factors). a1(b1+b3*Resilience factors)=Conditional indirect relations of interpersonal stress on depressive symptoms through anxiety symptoms. a1b1=Intercept. a1b3=Slope. The slope is the index of moderated mediation.
A total sample of 231 adults was recruited, but a final sample size of 210 was used for analyses due to missing responses. The sample comprised undergraduate students of the Research School of Psychology, graduate students of Graduate House and University House of the Australian National University (ANU), waiting passengers at bus stops in Canberra, and visitors to a psychology clinic in Sydney. Eighty-two respondents were aged between 18 and 25 years, 47 respondents were aged between 26 and 30 years and 81 respondents were aged 31 years and above. One hundred and eighteen were females, 91 were males, and one reported ‘other’ as gender. This study was approved by the Human Research Ethics Committee of the Australian National University (Reference Number 2015/549) as part of a bigger research project for the doctoral project of the first author. All participants gave written informed consent in accordance with the Declaration of Helsinki. Respondents completed a paper-and-pen questionnaire.
MeasuresResilience Scale for Adults (RSA)The RSA (Hjemdal et al., 2001) is a 33-item self-report scale for measuring resilience to psychosocial adversities among adults. It consists of six factors namely perception of self (PS), planned future (PF), social competence (SC), structured style (SS), family cohesion (FC), and social resources (SR). The RSA has been found to have cross-cultural validity and uses a 7-point semantic differential scale format. Each item has two opposite attributes at each end of the scale continuum to prevent acquiescence bias. Higher scores indicate higher levels of protective resources associated with resilience.
Patient Health Questionnaire (PHQ)The PHQ-9 (Kroenke, Spitzer, & Williams, 2001) is a nine-item self-report measure that assesses the frequency of depressive symptoms over the past two weeks. All items are answered using a 4-point Likert-type scale format ranging from 0 (not at all) to 3 (nearly every day) with total scores from 0 to 27. Example items include “Little interest or pleasure in doing things”, and “Trouble concentrating on things, such as reading the newspaper or watching television”. Higher scores indicate higher levels of depressive symptoms.
Generalized Anxiety Disorder (GAD-7)The GAD-7 (Spitzer, Kroenke, Williams, & Löwe, 2006) is a seven-item self-report measure that assesses anxiety-related symptoms in primary care. All items are answered using a 4-point Likert-type scale format ranging from 0 (not at all) to 3 (nearly every day) with total scores from 0 to 21. Example items include “Feeling nervous, anxious or on the edge” and “Trouble relaxing”. Higher scores indicate higher levels of anxiety symptoms.
Interpersonal stressInterpersonal stress was assessed by using the Stressful Life Events Questionnaire (SLE; Hjemdal, Friborg, Stiles, Rosenvinge, et al., 2006). SLE is self-report questionnaire designed to measure exposure to stressful life events. The total number of events is summed up in one sum score for everyone. Response categories were 0 (No) and 1 (Yes). Total scores ranged from 0 to 15. Example items include “break in relationship” and “unexpected death among close relatives”. Higher scores indicate higher exposure to stressful negative life events.
Statistical analysesStatistical analyses were conducted using SPSS version 24. Frequencies and mean scores were analyzed on all measures. Pearson product-momentum correlation was used to explore bivariate associations between continuous variables in the study. Spearman's rank correlation was computed to examine the relationship between ordered categorical variable (age) with continuous outcome variables (symptoms of anxiety and depression). Hierarchical linear regressions were performed to explore the contribution of individual resilience factors in protection against depressive symptoms while controlling for age and gender in step one. From step two to seven, the different factors were entered in the following order: FC, SR, SS, PS, PF, and SC, respectively. Moderated mediation models using PROCESS (Hayes, 2012) were estimated for all six resilience factors as moderators. Evidence of moderated mediation was assessed by using the index of moderated mediation (Hayes, 2015). Using a 95% bias-corrected bootstrap confidence interval based on 1000 bootstrap samples, a significant moderated mediation was confirmed if the 95% bias-corrected bootstrap confidence interval for the index of moderated mediation did not contain zero.
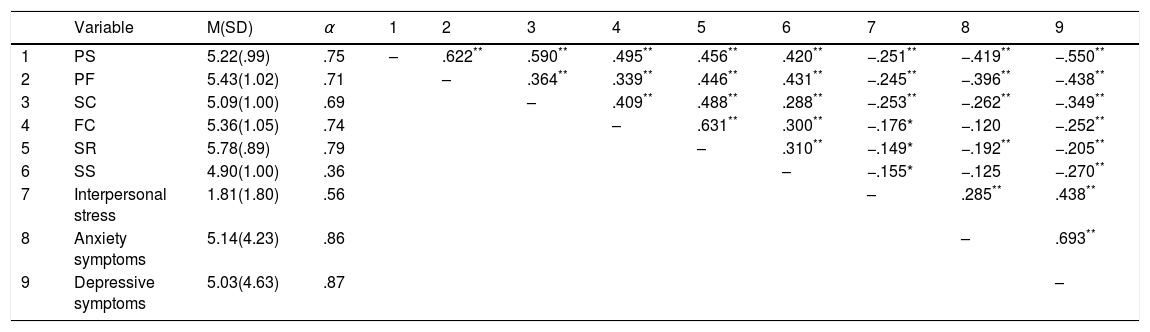
ResultsPreliminary resultsTable 1 displays the means, standard deviations and Cronbach's alphas of the measures used and their inter-correlations. Individual resilience factors were all significantly negatively associated with interpersonal stress, symptoms of anxiety and depression, except two resilience factors namely, family cohesion and structured style, which were not significantly associated with symptoms of anxiety. The Cronbach's alpha for the structured style factor was low.
Table of means, standard deviations, Cronbach's alpha estimates (α) and correlations for all the measures (N=210).
| Variable | M(SD) | α | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | PS | 5.22(.99) | .75 | – | .622** | .590** | .495** | .456** | .420** | −.251** | −.419** | −.550** |
| 2 | PF | 5.43(1.02) | .71 | – | .364** | .339** | .446** | .431** | −.245** | −.396** | −.438** | |
| 3 | SC | 5.09(1.00) | .69 | – | .409** | .488** | .288** | −.253** | −.262** | −.349** | ||
| 4 | FC | 5.36(1.05) | .74 | – | .631** | .300** | −.176* | −.120 | −.252** | |||
| 5 | SR | 5.78(.89) | .79 | – | .310** | −.149* | −.192** | −.205** | ||||
| 6 | SS | 4.90(1.00) | .36 | – | −.155* | −.125 | −.270** | |||||
| 7 | Interpersonal stress | 1.81(1.80) | .56 | – | .285** | .438** | ||||||
| 8 | Anxiety symptoms | 5.14(4.23) | .86 | – | .693** | |||||||
| 9 | Depressive symptoms | 5.03(4.63) | .87 | – |
Note. Intercorrelations among variables are shown above the diagonal. PS: perception of self; PF: planned future; SC: social competence; FC: family cohesion; SR: social resources; SS: structured style.
Since only one respondent reported ‘other’ as gender, this was removed when testing gender effects. Potential gender differences on all continuous variables were explored with independent t-tests. Gender differences were found for only social resources, with females scoring higher than males. The difference of 0.334, BCa 95% CI 0.094, 0.575, was significant t(207)=2.810, p<.01, with a small effect, d=.387. As age significantly negatively correlated with anxiety symptoms (r=−.225, p<.01) and depression (r=−.372, p<.001), a one-way MANOVA was performed. The multivariate effects on the combined dependent variables was significant for age, Wilks’ lambda: λ=.857, F (4, 412)=8.242, p<.001, partial η2=.074. Follow-up tests revealed significant effects of age on anxiety symptoms, F(2, 207)=4.855, p=.009, partial η2=.045 (accounting for 4.5% variance), and symptoms of depression F(2, 207)=16.648, p=.007, partial η2=.139 (accounting for 13.9% variance). Post hoc pairwise comparisons with Scheffé revealed significant group differences for participants aged 18–25 years, reporting higher symptoms scores than participants aged 31 years and above (mean difference: MD=1.817, 95% CI 0.214, 3.419) for anxiety symptoms. Significant group differences were found for participants aged 18–25 years, reporting higher symptoms scores than participants aged 31 years and above (MD=3.465, 95% CI 1.796, 5.134), and also participants aged 26–30 years reporting higher symptoms scores than participants aged 31 years and above (MD=3.646, 95% CI 1.693, 5.599) for depressive symptoms.
Main resultsWe report the squared semi-partial correlations as an indicator of the unique contribution of each factor; FC (sr2=.040, p<.01), SR (sr2=.019, p<.05), SS (sr2=.028, p<.01), PS (sr2=.184, p<.001), PF (sr2=.014, p<.05), SC (sr2=.005, p=.218). The results showed that except for social competence, individual resilience factors uniquely explained the variance in depressive symptoms. All observed associations were negative.
Exposure to interpersonal stress contributes to the explained variance in anxiety and depressive symptomsInterpersonal stress was significantly positively related to levels of anxiety (standardized: β=.29, p<.001) and depressive symptoms (β=.43, p<.001) when controlling for age and gender, accounting for 13.50% and 29.02% variance, respectively.
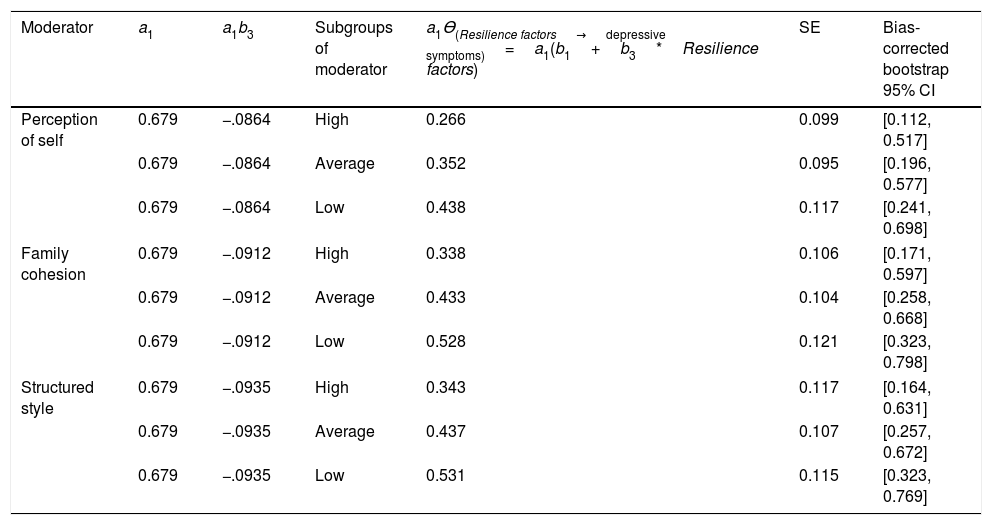
Moderated mediation modelAnxiety symptoms significantly mediated (completely standardized indirect effect: β=.176, CI: 1030, 0.2640) the association between interpersonal stress and depressive symptoms. In the moderated-mediation analyses, significant interaction effects were found for perception of self (β=−.027, p=.004), family cohesion (β=−.030, p=.004) and structured style (β=−.030, p=.002). The index of moderated mediation was significantly different from zero for perception of self (a1b3PS=−0.086, 95% CI −0.203, −0.003), family cohesion (a1b3FC=−0.091, 95% CI −0.199, −0.020) and structured style (a1b3SS=−0.094, 95% CI −0.190, −0.013). The confidence interval for the index of moderated mediation contained zero for planned future (a1b3PF −.035, 95% CI −0.126, 0.029), social competence (a1b3SC −.0734, 95% CI −0.198, 0.027) and social resources (a1b3SR −.0094, 95% CI −0.089, 0.066).
Table 2 displays the results of mediated effects by anxiety symptoms between interpersonal stress on depressive symptoms for high, medium and low subgroups of perception of self,family cohesion and structured style. It was found that the effect of interpersonal stress on depressive symptoms mediated by anxiety was strongly associated with adults with lower perception of self, family cohesion and structured style as compared to adults with higher levels. More specifically, high scoring subgroups showed a significantly lower effect of interpersonal stress through anxiety symptoms on depressive symptoms, than medium scoring subgroups whereas low scoring subgroups showed the highest negative effect. Additional results from the moderated-mediation analyses are shown in the supplementary material.
Derivation and quantification of, and inference about the conditional indirect relations as a function of resilience factors.
| Moderator | a1 | a1b3 | Subgroups of moderator | a1ϴ(Resilience factors→depressive symptoms)=a1(b1+b3*Resilience factors) | SE | Bias-corrected bootstrap 95% CI |
|---|---|---|---|---|---|---|
| Perception of self | 0.679 | −.0864 | High | 0.266 | 0.099 | [0.112, 0.517] |
| 0.679 | −.0864 | Average | 0.352 | 0.095 | [0.196, 0.577] | |
| 0.679 | −.0864 | Low | 0.438 | 0.117 | [0.241, 0.698] | |
| Family cohesion | 0.679 | −.0912 | High | 0.338 | 0.106 | [0.171, 0.597] |
| 0.679 | −.0912 | Average | 0.433 | 0.104 | [0.258, 0.668] | |
| 0.679 | −.0912 | Low | 0.528 | 0.121 | [0.323, 0.798] | |
| Structured style | 0.679 | −.0935 | High | 0.343 | 0.117 | [0.164, 0.631] |
| 0.679 | −.0935 | Average | 0.437 | 0.107 | [0.257, 0.672] | |
| 0.679 | −.0935 | Low | 0.531 | 0.115 | [0.323, 0.769] | |
Note: SE: standard error; CI: confidence interval; a1: effect of interpersonal stress on anxiety symptoms; a1b3: index of moderated mediation; a1(b1+b3*Resilience factors): conditional indirect effects at levels of resilience factors.
The current study examined a complex conceptual model that explored anxiety symptoms as mediating the association between interpersonal stress and symptoms of depression, and the protective value of individual resilience factors to understand how resilience factors are differentially involved in protection against common mental health problems. Overall, three main findings stand out. Firstly, interpersonal stress was significantly positively associated with levels of symptoms of depression and anxiety. Secondly, anxiety mediated the associations between interpersonal stress and depressive symptoms. Thirdly, except for the social competence factor, individual resilience factors in the RSA uniquely contributed to explaining the variance in symptoms of depression, while three factors (perception of self, family cohesion and structured style) moderated the associations between interpersonal stress, anxiety and depressive symptoms, suggesting protective value against common mental health problems.
Interpersonal models to understanding common mental health problems implicates interpersonal stress in the onset and development of anxiety and depression whereby, particularly for depression, it has been found that vulnerabilities to depression (whether cognitive or emotional) are expressed in interpersonal contexts, predicting and maintaining depression (Hammen, Rudolph, & Abaied, 2003). This may elucidate why interpersonal stress explained more variance in depressive symptoms than anxiety symptoms as well as explain the significant positive associations between interpersonal stress, anxiety and depressive symptoms. Interpersonal approaches to understanding common mental health problems suggest that depression is fundamentally an interpersonal disorder that is particularly damaging to relationships (Hammen et al., 2003). The current findings are also consistent with previous studies of depression and anxiety (Ingram & Luxton, 2005; Vrshek-Schallhorn et al., 2015). The fact that interpersonal stress explained portions of variance in both anxiety and depressive symptoms can be explained by the human need for interpersonal relationships.
The need to belong and the desire for interpersonal attachment, is a fundamental motivation among human beings. For example, it was found that lack of supportive interpersonal relationships could contribute to the onset of depression (Vrshek-Schallhorn et al., 2015). People with psychological difficulties such as anxiety and depression have interpersonal behaviours that produce an interpersonal space filled with rejection from others. This phenomenon causes the individual to seek reassurances as to whether people truly care about them, which may be perceived as exhausting by other people. For some this might lead to further rejection and more interpersonal stress, which shows transactional and bidirectional relationships between interpersonal stress and depression (Ingram & Luxton, 2005).
According to cognitive vulnerability theories, uncontrollable worry, apprehensions, and tensions in response to stress characterizing generalized anxiety could precede or give way to depression (but not the reverse), making anxiety itself a risk factor for the development of depression (Higa-McMilla et al., 2014). When conceptualized in this way, exposure to interpersonal stress could activate anxiety symptoms, which in turn, as a predictive risk variable, could markedly increase the likelihood of developing depression and could also act in concert with a predisposition factor for the onset of depression (Ingram & Luxton, 2005). This may explain our finding that anxiety symptoms measured by the Generalized Anxiety Disorder Scale mediate the association between interpersonal stress and depressive symptoms. Although this presents the research community with a starting point in this underexplored conceptual mechanism, more longitudinal studies are required to investigate this finding.
Consistent with previous studies (Anyan et al., 2018; Anyan et al., 2017; Hjemdal, Friborg, Stiles, Rosenvinge, et al., 2006) the current findings show that perception of self, family cohesion, and structured style moderated the indirect associations between interpersonal relationships, anxiety and depressive symptoms. Negative self-system processes and explanatory styles have been implicated as central components in theories of depression. Elevating people's self-confidence and self-worth may attenuate negative interpretations and attentional biases from the lack of one's own ability and resources in forming and maintaining interpersonal relationships. This in turn can result in a higher perception of self, sense of autonomy and independence to overcome depression associated with interpersonal stress (Nolen-Hoeksema, Girgus, & Seligman, 1992). In overcoming depressive feelings, family cohesion provides affective qualities for emotional bonding and regulation to promote intra- and inter-personal resilience that help individuals spiral upwards when facing stressful life events. For example, previous studies have favoured stable and supportive family home environment marked by coherence in family relationships emotional bonding as a protective factor against depression (Hjemdal, Friborg, Stiles, Rosenvinge, et al., 2006). Individuals showing structured style attributes are often more persistent in the face of challenges and engage more in active and problem-focused coping by employing proactive strategies, rather than avoidance strategies when under pressure which may explain overcoming depressive symptoms (Grevenstein, Aguilar-Raab, Schweitzer, & Bluemke, 2016).
High scoring subgroups in perception of self, family cohesion, and structured style were associated with lower effect of stress from interpersonal relationships through anxiety symptoms on depressive symptoms, compared to the low scoring subgroups. Thus, the indirect effect of exposure to interpersonal stress on depressive symptoms systematically varied across subgroups of perception of self, family cohesion and structured style. As with a previous study (Anyan et al., 2017), the authors found that negative effect of exposure to stressful life events mediated by anxiety on depressive symptoms systematically varied across subgroups of resilience. The authors concluded that more access to resilience resources or high resilience resources available, could serve as a protective factor against direct negative life events as well as negative life events that may confront them indirectly through other channels of adversities.
Limitations and future directionsThere are some limitations in the present study. The structured style factor had a low reliability score, but still appeared useful for research purposes to detect expected effects at conventional significance levels (John & Soto, 2007). Additionally, since the factors were derived from the subscales of the RSA, there could be multicollinearity issues. However, as indicated in the descriptive statistics in Table 1, the intercorrelations were generally moderate, which means that the factors relate to measuring resilience but also contain unique aspects as constructs. We have provided strong evidence by using conditional process modelling (i.e., moderated mediation) to explain how different resilience factors are differentially involved in the protection against anxiety and depressive symptoms. However, cross-sectional research designs are not able to explain protective processes and temporal changes. Longitudinal studies are needed to investigate the hypotheses further. It will be interesting to see how the different resilience factors also perform depending on the nature and severity of different levels of stress exposure. It remains unclear whether interpersonal processes associated with the generation of interpersonal stressors contribute to anxiety and depression in the same way. Future research may benefit from examining the specificity and overlap of interpersonal processes that account for anxiety and depression. In future studies, it is recommended that researchers examine subgroups in the nature and severity of stress exposure. The measures used in this study were self-report questionnaires, which pose challenges resulting from social desirability and general false answers for a study that relied on retrospective behaviours and thoughts. Finally, respondents from the general population were recruited for this study with a few who had visited a psychology clinic in Sydney but have not been assessed or diagnosed. It will be interesting to see how resilience factors are differentially involved in protecting against common mental health problems among a clinical sample, which could also enrich targeted interventions.
ConclusionsResults from this study support the mediating effect of anxiety symptoms between interpersonal stress and depressive symptoms and further show that resilience factors are differentially involved in protection against common mental health problems. The results also show that individuals who score high on the different factors namely, perception of self, family cohesion, or structured style will show lower negative effects of exposure to interpersonal stress on common mental health problems. Our results can contribute to developing health interventions that use a resilience approach by increasing perception of self, family cohesion, and structured style while reducing stress from interpersonal relationships. Furthermore, the present study provides knowledge that can help understand how adults may overcome common mental health problems, and how we can use that knowledge to enhance, strengthen and reinforce coping efforts among adult populations. Different resilience resources may exert greater or lesser impact in resilience processes and outcomes. Evidence of uneven functioning across different resilience factors will contribute to understanding the mixed successes in implementing resilience-based interventions and favour the prudent use of limited resources.
Author's contributionsFA and SHI conducted data analysis. All authors contributed. FA drafted the initial study design, wrote the first and successive drafts of the manuscript. SHI and OH contributed to writing and revising the manuscript. All authors have read and approved the final manuscript.
FundingThe Faculty of Social Sciences and Technology Management, Norwegian University of Science and Technology as part of the joint PhD in Behaviour and Health program with the College of Health and Medicine, Australian National University funded this study.
Competing interestThe authors declare that they have no competing interests.
We would like to express our gratitude to all participants who responded to participate in this study.