Introduction
Heart failure (HF) is recognized as an important and increasingly worrisome public health problem in developed countries.1 The aging of the population along with increased survival of patients with ischemic heart disease or hypertension and other diseases the cause HF mean that the incidence of HF is expected to increase in coming years. Patients with HF require different types of health care (i.e., primary, specialized, and hospital care) and incur considerable costs within the health care system. Despite the problems in obtaining precise data, some studies have estimated a prevalence in Spain of 5.3 per thousand, and a direct annual cost of 64 028 to 110 240 million pesetas, representing between 1.8% and 3.1% of the annual public health budget.2
The tendency in Spain toward decreasing mortality and increasing morbidity and hospitalization because of HF3,4 indicate a need for improved treatments and follow-up for diseases that cause HF, with the intention of decreasing its prevalence, morbidity and mortality. In addition, these trends illustrate the importance of improving coordination between different levels of care for patients with HF. An earlier study reported the results obtained with regard to hospital care.5 The present report offers further information in the form of an analysis of the health care process for patients who are hospitalized for HF at a tertiary center, and for surviving patients who are subsequently followed by a primary care service after discharge.
Material and methods
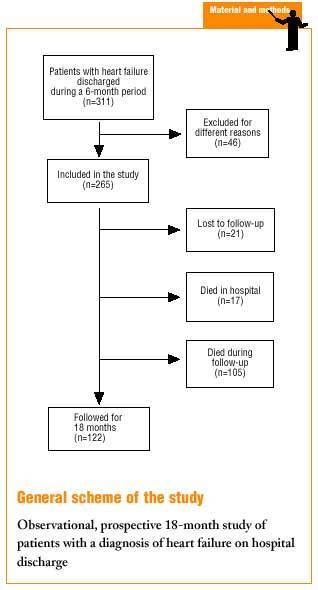
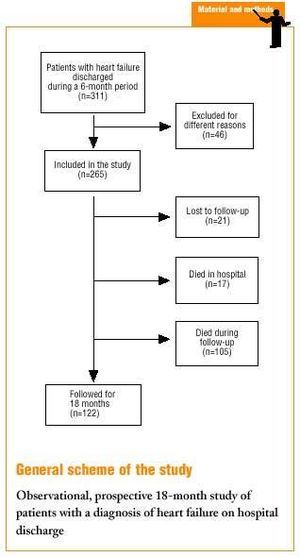
The methods were described in detail in a previous report.5 In summary, 311 patients with HF were identified as having been discharged between 1 July and 31 December 1998 from a tertiary hospital serving a reference population of 450 000 inhabitants. Heart failure (code 428 in the International Classification of Disease, Ninth Revision) was the first, second or third diagnosis. The diagnosis of HF was confirmed, on the basis of a slight modification of the Framingham criteria,6 by a physician who was one of the authors of this study. Global or biventricular HF was considered to exist if criteria for pulmonary vein congestion coexisted with physical signs of systemic venous hypertension. Patients with HF from a reversible cause, with terminal illness, or who resided abroad (and hence could not be followed for the full study period) were excluded. Patients seen in the emergency room but not admitted were also excluded because of difficulties in obtaining full clinical information for the present study.
Of the 311 patients identified whose hospital record was reviewed, 265 fulfilled all inclusion criteria (85.2%).
The hospital records were reviewed to note demographic, clinical and pharmacological data, and status upon discharge. Clinical and pharmacological data, and information on factors related with quality of life 18 months after discharge, were obtained with systematic telephone interviews. Some primary care center records were reviewed to verify the responses given in the telephone interview.
A total of 227 patients or relatives were contacted by phone (some after several tries); 8% were lost to follow-up. To validate the information regarding cause of death obtained from the telephone interview, the hospital record was reviewed for patients who died during a subsequent hospital readmission.
A descriptive analysis was done for all variables by calculating the frequency distribution for discrete variables, or the mean and standard deviation for continuous variables. Univariate analysis was used to compare the clinical characteristics of surviving patients who were discharged but who died during follow-up and discharged patients who were still alive at the end of follow-up. To compare the characteristics of patients with a good and a poor prognosis at the end of the follow-up period, the chi-squared test was used for qualitative variables, and Student's t test was used for continuous variables. Multivariate analysis with the Cox proportional risks model used mortality during follow-up as the dependent variable. As independent variables we used those demographic, clinical and treatment variables of relevance to the course of the disease that showed a significant relationship in the univariate analysis.
Results
The clinical outcomes in our sample of hospitalized patients were published in an earlier article.5 Briefly, the final number of patients included was 265; 57% were women and 43% were men, and mean age was 75 years. Almost 40% of the patients were more than 80 years old, and more than 70% were older than 70 years. Retired persons made up 85% of the sample; 12% were actively employed and 3% were incapacitated. The main cause of hospitalization was HF in 73.5% of the patients; 7.5% were admitted because of acute myocardial infarction, and the remaining 19% were hospitalized for a variety of reasons such as pneumonia or other respiratory disease, cerebrovascular accident or surgery. More than half (58%) were admitted through the internal medicine service, and 21% were admitted through the cardiology service; the latter patients were predominantly men and were younger than the mean age of the sample as a whole. The remaining 21% were admitted through other hospital services. Hospital mortality was 6.4%.
Table 1 shows the main clinical findings on discharge in surviving patients. There were antecedents of HF in 69% of the patients; the prevalence of hypertension was 54.8%; a previous history of angina was recorded in 25.4%, and a previous history of infarction was present in 22.6%. Significant underlying disease (e.g., chronic renal failure, neoplasm, cerebral or peripheral vascular ischemic disease) was present in 62.5% of the patients.
At the time of hospitalization 87% of the patients were classified as NYHA functional class III-IV, 24% were admitted for clinically acute pulmonary edema, and 56% had global HF.
The causal factors of HF identified were hypertension in 50% of the patients, coronary disease in 33.8%, valvular disorder in 23.4% (not related to valve replacement or already treated surgically), cardiomyopathy in 6.1%, and other factors in 3.2% (chemotherapy toxicity, congenital disease, amyloidosis). The underlying cause was unknown in 13.3% of the patients.
Electrocardiogram and chest x-ray were done in all patients. Ventricular function was evaluated in 67.7% (echocardiography, isotopic ventriculography or coronary arteriography done before or during hospitalization or during follow-up); the results showed normal function in 42.3% of the patients (ejection fraction >50%), slightly (ejection fraction 50%-40%) or moderately impaired function (ejection fraction 39%-30%) in 35.7%, and severe impairment (ejection fraction <30%) in 22%. Ventricular function was calculated in 92.2% of the patients younger than 75 years and in 50.7% of those older than 75 years; in 78.3% of the men and 59.8% of the women, and in 93.5% of all patients admitted through the cardiology service vs. 61.8% of the patients admitted through other services.
The drugs used most often on discharge were diuretics (93%) and ACE inhibitors (48%). Digitalis was used by 38% of the patients, and beta-blockers (carvedilol and others) by 4%. Angiotensin-converting enzyme inhibitors and angiotensin receptor antagonists (ARA-II) were prescribed for 61.3% of the patients for whom ventricular function had been determined, vs. 38.7% of those who had not undergone this test; these drugs were also prescribed for 72.2% of the patients with impaired ventricular function vs. 46.5% of those with normal functioning. There were no differences in the use of ACE inhibitors or ARA-II between patients older and younger than 75 years.
Results of follow-up
Follow-up data were obtained for 122 surviving patients; for patients who died, data were obtained only for cause of death. Overall mortality was 46.2%. In 76.8% of the patients the cause of death was heart disease; in the remaining 23.2% other causes were identified (e.g., neoplasm, cerebrovascular accident or renal failure). Mean age of the patients at the time of death was 80 years; mean age of survivors was 72 years. Of the latter, 60% were classified as functional class I-II, in contrast to the high percentage of patients in class III-IV at the time of hospitalization.
During the 18-month follow-up period 38.5% of the patients were hospitalized for HF; of these, 40% were seen in the emergency room (58% of the patients were seen 2 or more times in this service) and 60% were admitted (34% of these patients were admitted 2 or more times). Surgical treatment was used in 7% of the patients; of these, 86% underwent valve replacement and 14% underwent myocardial revascularization. Only 1 patient was awaiting heart transplantation. After discharge ventricular function was evaluated in 28.7% of the patients; testing was done in the hospital in most cases, whereas ventricular function was evaluated at a primary care service in only 6% of the surviving patients. The results were normal in 58% of the patients, and revealed slight or moderate impairment in 29% and severe impairment in 13%.
Pharmacological treatment during the 18-month follow-up period did not differ substantially from the treatment prescribed upon discharge. As shown in Table 2, the most frequent modification in drug prescription involved the ACE inhibitors (18%), which were stopped most frequently (10.6%) because of side effects (1.6%) or substituted with other drugs (9%). The drug added most frequently to the follow-up treatment regimen was spironolactone (13%). During the 18-month follow-up period most patients were seen by at least one physician, and often by a specialist in addition to the general practitioner (Table 3). The family physician was consulted most often (mean of 6 visits), followed by hospital out-patient clinic staff (mean of 4 visits, although it should be noted that 19% of these patients were participating in clinical trials) and cardiologists (mean of 3 visits). Seven percent of the patients consulted their private physician, 5% were living in a social health center and 2% were not seen by any physician after hospital discharge. Altogether, the patients made a total of 543 visits to family physicians, 161 visits to hospital out-patient clinics, and 118 visits to cardiologists. Of the primary care centers where patients were seen, 74% were operating under the new, reformed system; the remainder were operating under the previous set of regulations for the provision of primary care through the Spanish national health system.
Of all surviving patients, 76.4% went out and walked regularly, and 24.7% practiced some type of recreational activity and physical exercise. These results are consistent with the percentage of patients who enjoyed an acceptable functional capacity.
Multivariate analysis showed that the best predictors of mortality after 18 months were age 75 years or older, global HF and comorbidity (Table 4).
Discussion
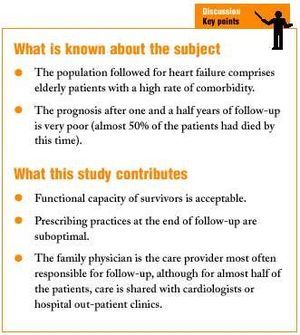
The results of this study confirm that in our reference area, HF affects mainly elderly patients; the prognosis is most likely to be poor in patients older than 75 years, as reported in earlier studies.7,8 The notable influence of comorbidity on the prognosis is clearly illustrated by the fact that 20% of the patients hospitalized for HF died of causes other than heart disease. An antecedent of noncardiac disease at the time of hospitalization was a predictor of mortality, and around half of the patients hospitalized for causes other than HF or acute myocardial infarction died of HF. The overall mortality rate in these patients was similar to that in patients admitted for HF. However, these data should be considered with caution because they were obtained by telephone interview, and because one of the noncardiac causes was cerebrovascular accident, which may well have been a complication of underlying heart disease. Nevertheless, as noted earlier, the reliability of the telephone survey data was verified in a small subgroup of patients who died during a subsequent hospital readmission, as many of these patients died of noncardiac causes. Our results suggest that the role of comorbidity is important, and this factor should be evaluated in depth in patients with HF not only because of its influence on the prognosis, but also because it may affect the approach to therapy.
A possible limitation of this study is the fact that we were dealing with a population of hospitalized patients discharged with a diagnosis of HF. Other published studies have centered on the diagnosis and follow-up of patients with HF in the community, and their results therefore can not readily be compared with ours. A study of patients in Olmsted County, Minnesota (U.S.A.)9 of the incidence and prognosis in patients with HF identified 216 patients and found a 1-year survival rate of 76%, a figure much higher than our 18-month survival rate. However, another population-based study --the Framingham study10-- identified 652 individuals with HF and found a 1-year survival rate of 57% in men and 64% in women, figures closer to (in fact, slightly lower than) ours, and somewhat hard to explain.
Although pharmacological treatment during follow-up in survivors did not vary in overall terms from that prescribed upon hospital discharge, some changes are worth mentioning. Angiotensin-converting enzyme inhibitors were stopped in 10% of our patients (almost always because of side effects), and were added to the regimen in 5.8% of the patients. Angiotensin receptor antagonists were added to the regimen in 7% of the patients (almost always as a substitute for ACE inhibitors). Side effects from ACE inhibitors are not infrequent. A recent systematic review11 found a 30% rate of undesirable effects for these drugs, which had to be stopped in 15% of the patients (twice the rate found for the placebo). Spironolactone was introduced only during follow-up treatment: no patient was taking this drug upon discharge, whereas it was later prescribed for 13% of the patients. The change in treatment may reflect the publication of the RALES study,12 which appeared during the follow-up period of the present study. This clinical trial showed that mortality was lower in patients with NYHA grade III-IV HF and ejection fraction <0.35; moreover, all patients were also taking ACE inhibitors and loop diuretics. However, the results of the RALES study were not translated to clinical practice strictly as reported: 62.5% of the patients treated with spironolactone had class I-II impairment, and only 37.5% were taking ACE inhibitors (although most --87.5%-- were also taking diuretics). Ejection fraction had been measured in only 44% of these patients, of whom 57% had normal or only slightly reduced function. These figures illustrate that the extrapolation of the results of clinical trials to practice is not always linear, for different reasons ranging from inadequate knowledge of the scientific evidence (possibly leading to over-reliance as well as to under-reliance on the findings) to a conscientious, reasoned use of the evidence, which in the case of spironolactone might reflect an actual clinical need. A current paradox in the treatment of HF is that the main results of clinical trials refer to improvements in survival, whereas the practicing physician´s priority is to improve symptoms.
Beta-blockers are another group of drugs whose use was unchanged between discharge and follow-up, although in this case the most notable finding was their relatively low use. At the time our patients were discharged, an earlier clinical trial13 had shown these drugs to be beneficial, and by the end of the follow-up period additional studies likewise reporting positive findings had appeared.14,15 The use of beta-blockers may be influenced by other factors such as the classic notion --possibly persisting to this day-- that these drugs are contraindicated in HF, or the difficulties involved in titrating the dose over a number of periodic visits.
An analysis of usage of medical services during the follow-up period shows that HF consumes a non-negligible amount of health care resources. The practitioners most often responsible for these patients are family physicians, although in 48% of the patients care was shared with cardiologists or hospital out-patient clinics. This finding is indirect evidence of some degree of coordination between levels of care, although a more specific study would be needed to describe the quality of the process.
About 25% of the population of surviving patients took part in recreational activities and physical exercise. This finding is consistent with existing evidence of the prescription of physical exercise for these patients,16,17 and although the data are not very robust, it appears that exercise improves functional capacity and quality of life.
The factors that predicted mortality in the present study --age and clinical severity-- do not differ substantially from those found in earlier reports.18,19 One study in our setting found that the most important predictors of hospital mortality were myocardial infarction, hyponatremia and renal failure.20 A remarkable fact is that simple clinical markers such as biventricular HF or comorbidity carry more weight than do coronary disease or degree of ventricular function impairment, a finding also reported by others.21,22
Among the limitations of the present study are its local nature and the uncertainties surrounding the applicability of our findings to the entire population of patients with HF, as our patients were selected as having been discharged from the hospital. Nevertheless, it is worth emphasizing the consistency between our results and those of other populations of hospitalized patients in a variety of other distant settings.9 This suggests that our findings are valid for this type of population.
In conclusion, patients hospitalized for HF and followed by primary care services comprised an elderly population with a high percentage of comorbidity. Hypertension was the most frequent risk factor, and the prognosis at one and a half years of follow-up was very poor. Prescribing practices during the follow-up period can be considered suboptimal.
Acknowledgments
We thank Aida Ribera Solé, Purificació Cascant Castelló, Josep Pinar Sopena and Marius Morlans Molina of the Vall d´Hebron University Hospital, Barcelona, and X. Mundet Tuduri of the El Carmel Primary Care Center for their contributions to the study design, statistical analysis and writing of the manuscript. The research was financed in part by the Agència d´Avaluació de Tecnologia Mèdica (12/15/98) of the Catalonian Department of Health and Social Security.
Corrrespondence: Carlos Brotons Cuixart. Unidad de Epidemiología Clínica, Servicio de Cardiología,
Hospital General Universitario Vall d´Hebron. Pge. Vall d´Hebron, 119-129. 08035 Barcelona, España.
E-mail: brotons@hg.vhebron.es