We present the case of a 16-year-old female adolescent with an increase of volume in the superior third of the medial face of the left thigh.
1.1HistoryThe patient's mother is a healthy 36-year-old housewife, and the 42-year-old father is an employee who smokes and refers social alcoholism. The patient's brother is a healthy 11-year-old boy. Native and resident of the State of Mexico (Tlalnepantla). She lived in Tucson, Arizona, for ten years in a borrowed house provided with all services. Her dietary intake was adequate regarding quantity and quality.
Psychomotor development. Concerned as appropriate. The patient attended the second year of high school with good grades (average of 9).
She was the product of a second pregnancy with regular prenatal control, born by vaginal delivery with a weight of 3800g. She cried and breathed at birth.
She had a mild traumatic brain injury at four years of age and chickenpox at 11 years of age. A biopsy was taken from the right inguinal region on September 18, 2013, in Tucson, Arizona. Allergies denied.
Lab tests. Blood count: hemoglobin 9.60g/dl, hematocrit 26.9%, mean corpuscular volume 85.70 fl, mean corpuscular hemoglobin concentration 30.50g/dl. Erythrocytes 3.15×100/μl, leukocytes 0.20×103/μl, platelets 26×103/μl, neutrophils 17.60%, lymphocytes 23.5%, eosinophils 58.90%. No monocytes or basophils observed.
Blood chemistry: glucose 91mg/dl, alkaline phosphatase 129 U/l, total bilirubin 2.52mg/dl, indirect bilirubin 1.11mg/dl, direct bilirubin 1.41mg/dl, albumin 1.6g/dl, globulin 2.1g/dl, aspartate amino transferase 13 U/l, alanine amino transferase 20 U/l, sodium 139 mmol/l, potassium 2.8 mmol/l, calcium 7.2 mmol/l, phosphorus 3.2mg/dl, chloride 101mg/dl, creatinine 1.0mg/dl. Prothrombin time 31.5 s, international normalized ratio 2.44, partial thromboplastin time 48 s, fibrinogen 420mg/dl.
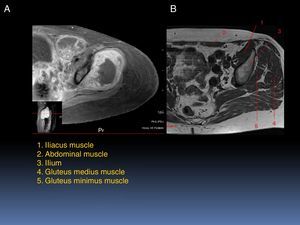
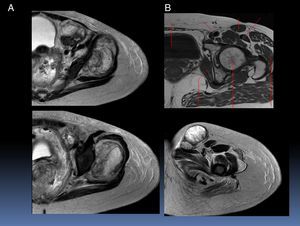
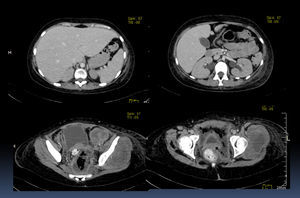
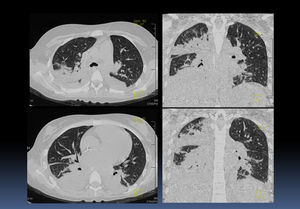
The patient began with an increase in the volume of the upper third of the medial side of the left thigh, which resulted in a limitation of mobility without reference to time evolution. A biopsy was performed, which reported a small and round cell tumor consistent with Ewing sarcoma with positive bcl-2, vicentin, and Ki67. A computerized axial tomography (CAT) scan was performed in three regions. In the left inguinal region, a soft tissue tumor of 2.5×2.7cm, adjacent to the femoral blood vessels was observed. Another hypodense tumor of 7.2×5.7×9.2cm involving the left gluteus minimus and adjacent to the ipsilateral iliac region was observed, as well as an increased volume and involvement of adjacent soft tissues, which measured 3.5×5.7×9.2cm, in the left iliac muscle. A lung nodule of 1.2×1×1.4cm and two small nodules in the upper right lobe were found, as well as mediastinum and abdominal lymph ganglia without apparent lesions. The patient was referred to the Hospital Infantil de Mexico Federico Gomez (HIMFG). Nuclear magnetic resonance (NMR) of the lower limb showed a 6.5×5.1×6.4cm solid appearance image at the gluteus minimus. At the ipsilateral iliac region, nodular images that extended to the inguinal neurovascular bundle were observed. Subsequently, a thallium-201 (201Tl) scintigraphy was conducted. A tumor in the hypogastrium was observed, with little uptake in cystic or necrotic areas in the soft tissue of the left gluteus and with probable bone metastases.
The patient began chemotherapy with vincristine, doxorubicin, and cyclophosphamide, and continued with a second cycle. Control NMR was performed. In T1 sequences, images of intermediate intensity related to bleeding were observed. In T2, a hyperintense heterogeneous gradient, and infiltration of the muscles were observed. An image with the same characteristics was noticed in the pelvic floor. The lesion infiltrated the hip bone.
When the third cycle of chemotherapy began, a deteriorating neurologic status, with 134/min heart rate and 52/min respiratory rate were detected. Chemotherapy improved general conditions. However, the patient developed nystagmus. Therefore, hospital discharge was delayed. She was evaluated by the Neurology service due to short and spontaneous blurred vision; 12h later, persistent horizontal eye movements were added. In the neurological exploration, she was found alert, active, cooperative, adequate person, time, and space orientation, with consistent, fluid, and clear language, gnosias, preserved calculation, abstraction and memory processes. It was concluded that probably the nystagmus was drug-induced. She presented oral candidiasis, which was treated with nystatin, as well as one-minute tonic-clonic seizures, which subsided with the administration of diazepam. She was treated with vancomycin, ampicillin, meropenem, and amphotericin due to fever peaks of 39.5°C and sepsis.
The following day, the patient developed cardiopulmonary arrest, which was treated with positive pressure ventilation, milrinone, norepinephrine, vasopressin and vasoactive amines. She responded to resuscitation maneuvers and remained intubated. An anterior nasal packing was placed due to epistaxis. Fresh frozen plasma was given, but the patient showed no improvement. Parenteral nutrition was added to the treatment. She presented impaired renal function with 1.6mg/dl of creatinine and diagnosed with multiple organ failure.
For a second time, the patient presented epistaxis, hypotension, and cardiopulmonary failure. Resuscitation maneuvers were suspended with the consent of the father. Final clinical diagnoses were primary Ewing sarcoma of the pelvic floor with treatment and multiple organ failure.
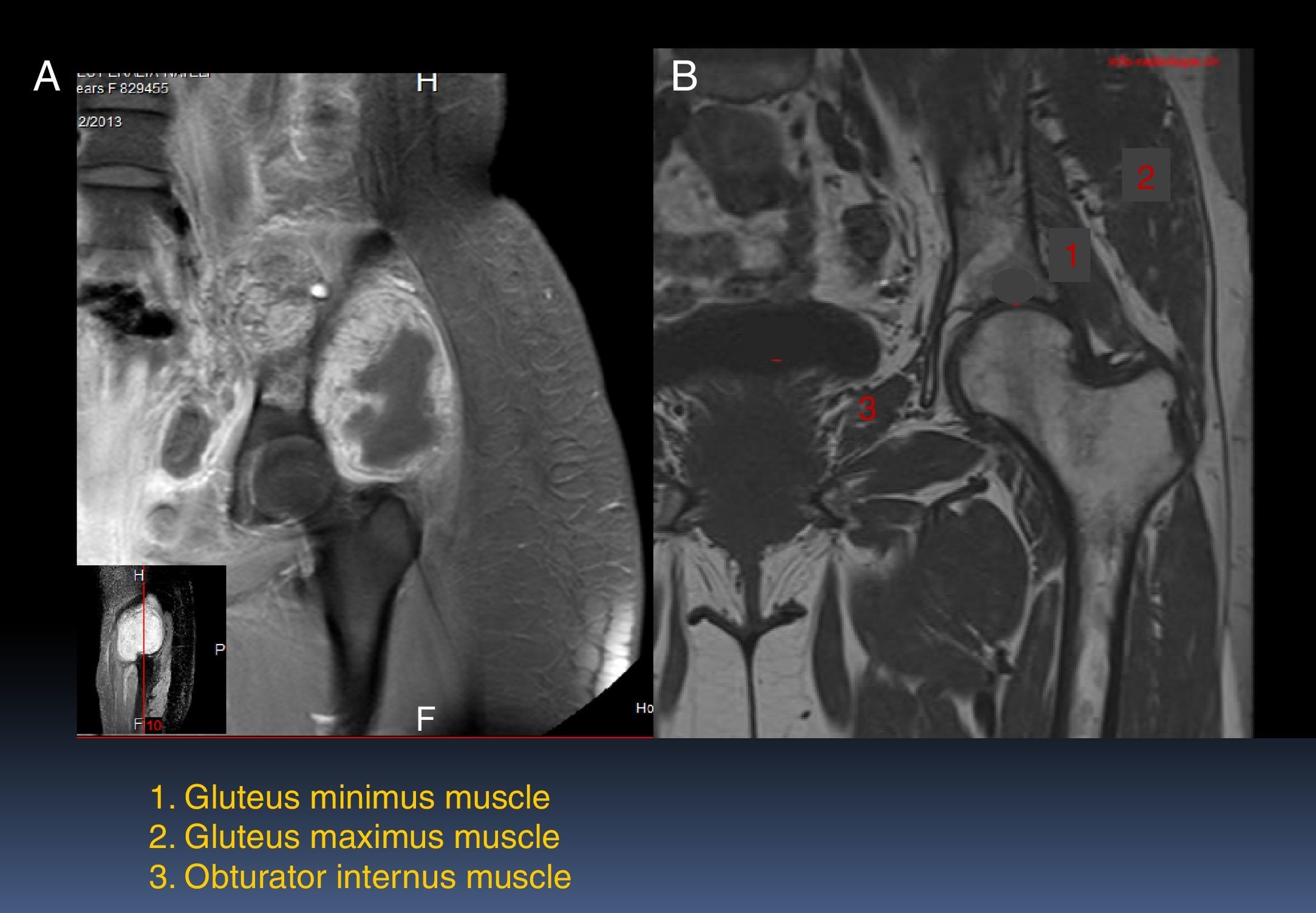
2ImagingThe patient underwent T1-gadolinium MRI, where muscle groups involved in the condition of the patient (Fig. 1A) were compared with non-affected muscle groups (Fig. 1B). There are different components of the femur, gluteus medius, and obturator internus. In relation to the neoplasm, the injury is hypointense. The administration of the contrast dye presents a peripheral enhancement with the adjacent soft tissues edema. The lesion infiltrates and compromises the iliac and part of the obturator internus. The urinary bladder is displaced towards the right side.
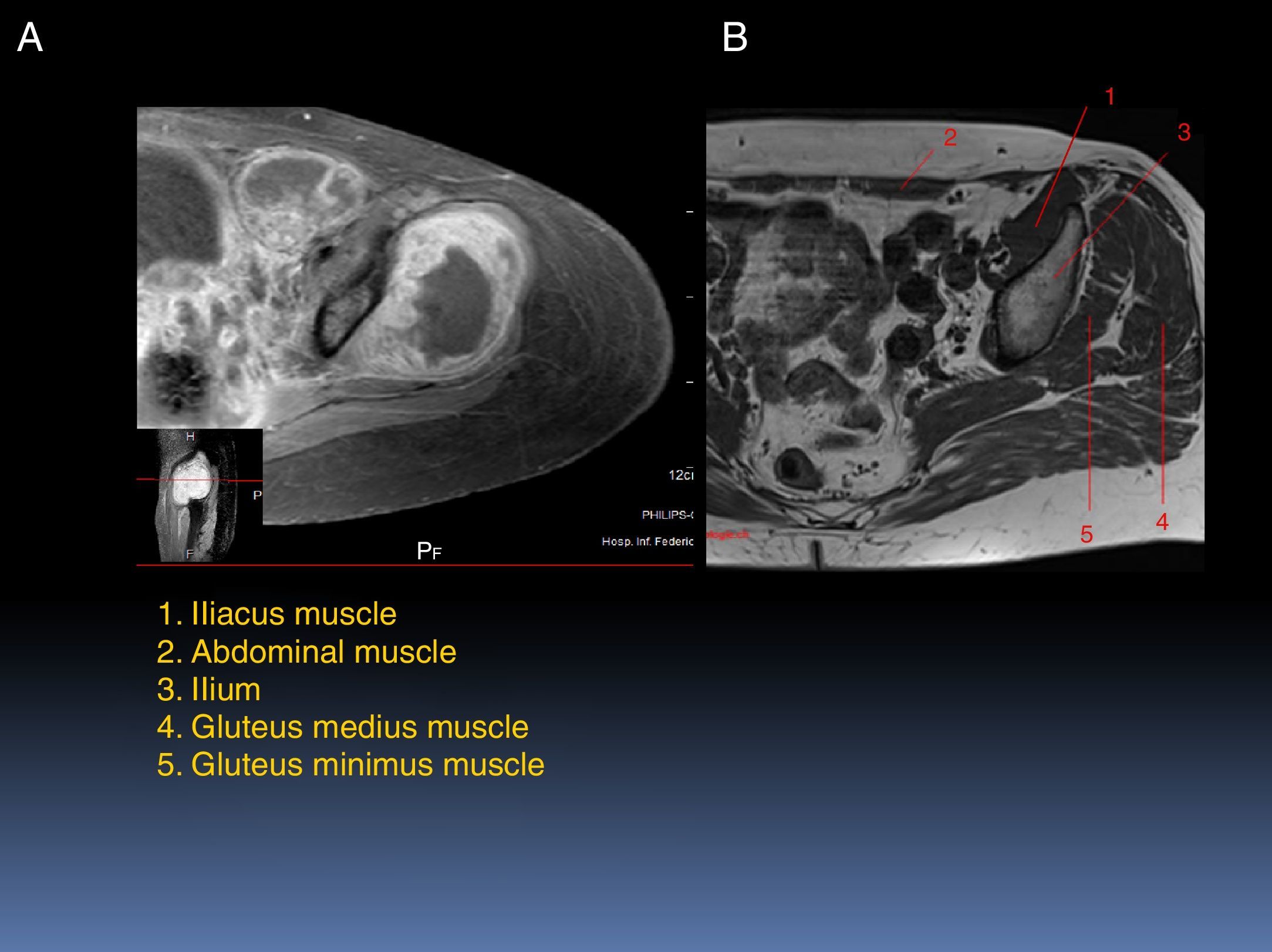
Figure 2 shows a T1 with the contrast dye, where the muscles are affected by the tumor can be observed (Fig. 2A). The lesion infiltrates muscle groups 4 and 5, which are gluteus medius and gluteus minimus, respectively (Fig. 2B). The abdominal muscle is displaced by both its own and the iliacus muscle edema, which is also affected by the tumor. In the pelvic floor, edema and hyperemia of the different components of the muscle are observed. Also, the pubococcygeus muscle shows edema.
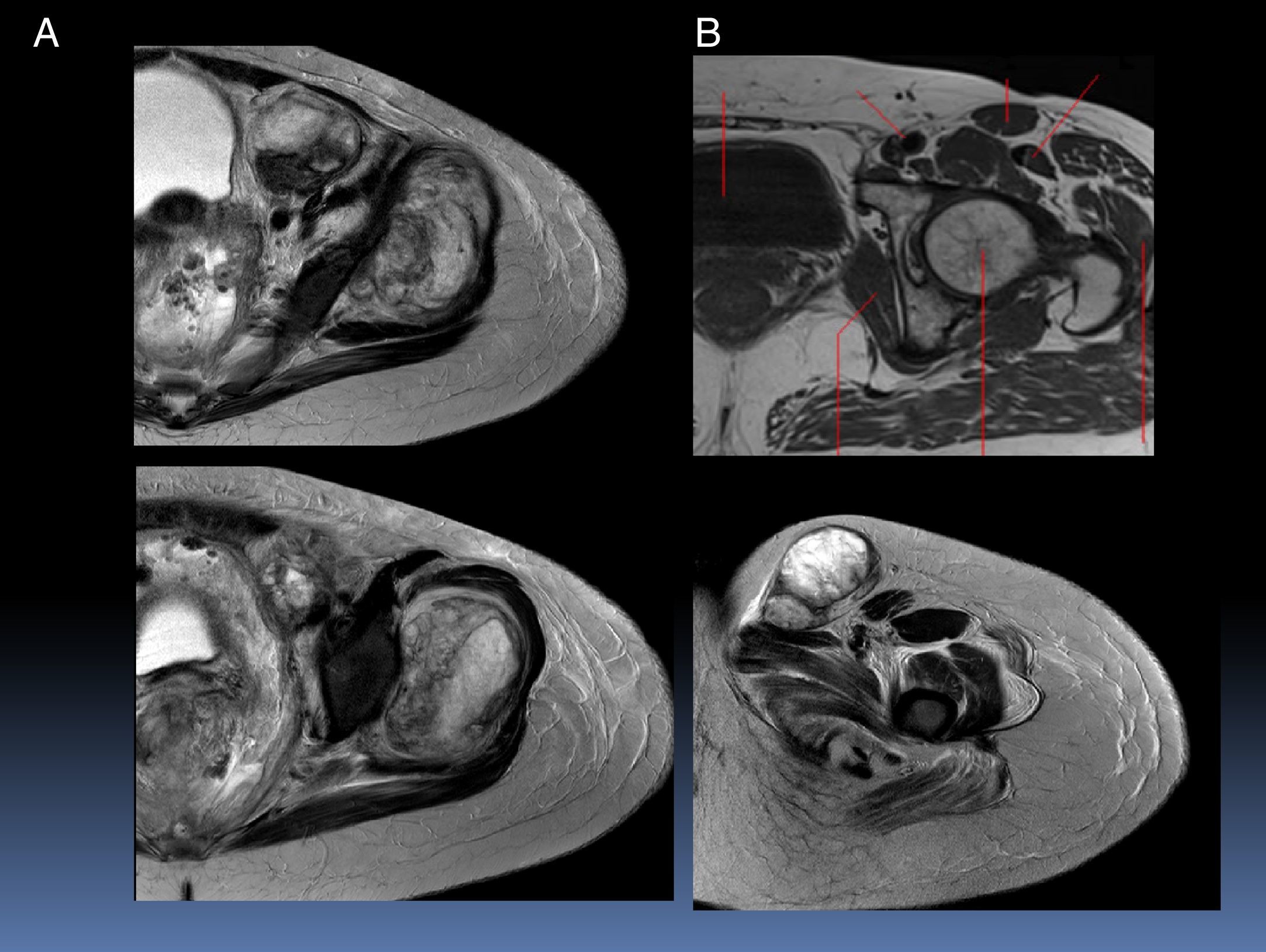
Figure 3 corresponds to T2, where the infiltration of the tumor causing striation of the adjacent adipose tissue can be observed. The lesion is nodular, adjacent to the femoral vessels and it extends through the inguinal canal. The urinary bladder is displaced to the right.
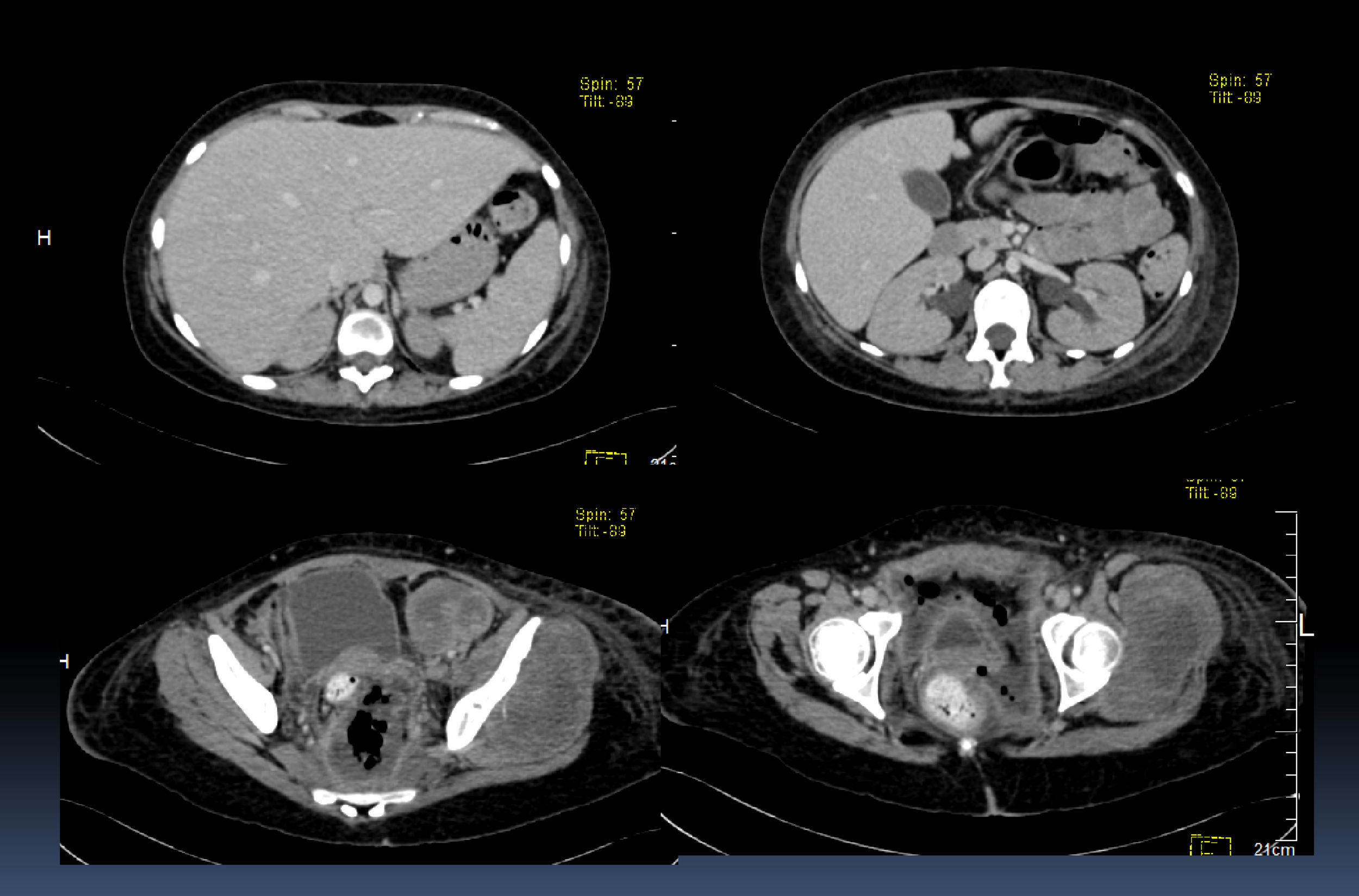
In a CT scan with contrast medium, an increased liver at the expense of the left lobe and bilateral hydronephrosis were observed. The gallbladder bile had no alterations. The tumor was observed in lower image slices. The displacement of the bladder and the uterus by the size of the tumor becomes clear two image slices below. Also, a part of the sigmoid colon and the rectal ampulla are slightly displaced towards the right by these lesions (Fig. 4).
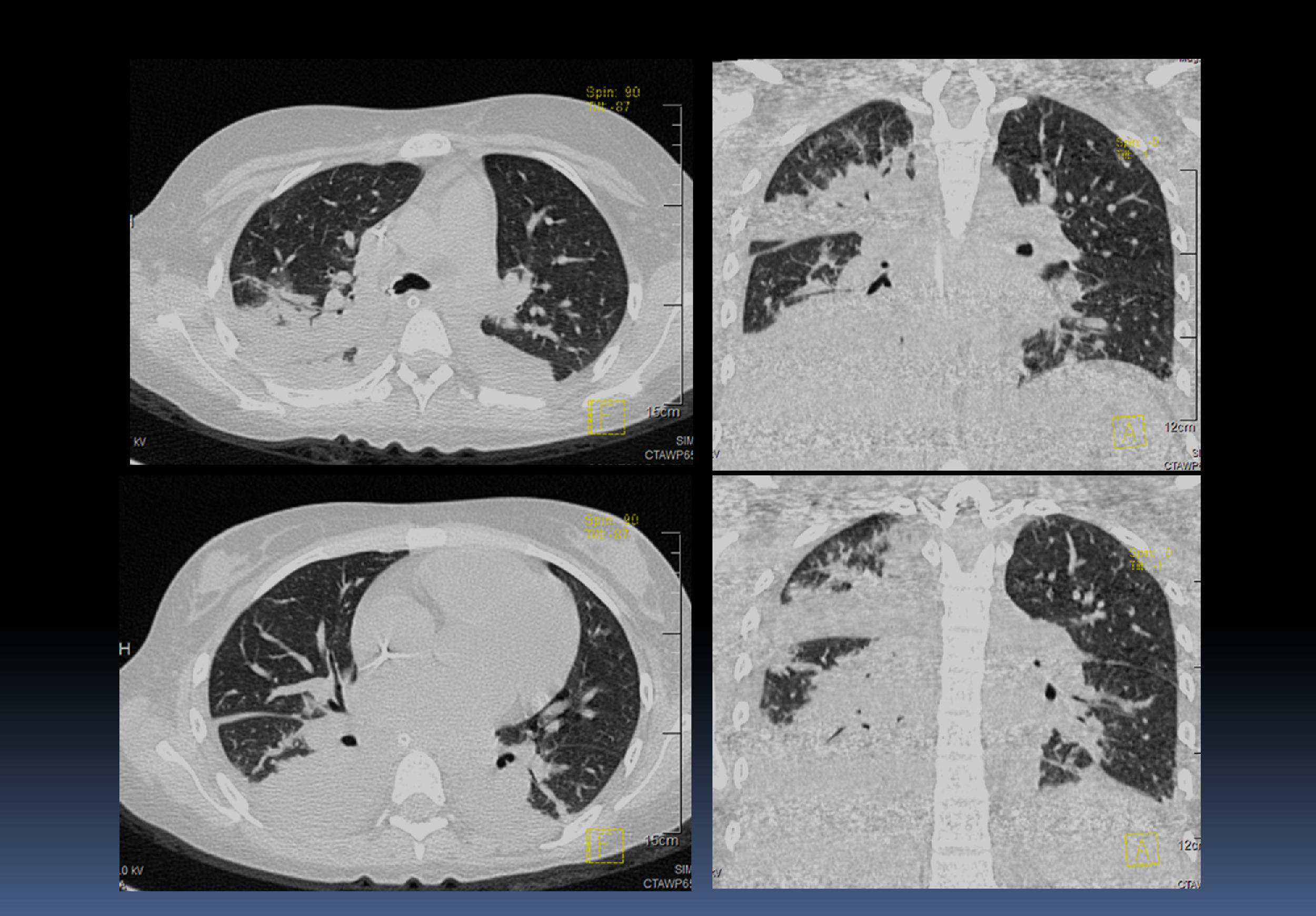
Different images of thorax axial and coronal sections showed consolidation in the posterior portion of both lungs, as well as air bronchogram and bilateral infiltrates, most apparent on the right side than the left side (Fig. 5). Metastasis was discarded by a specific scanning. Mostly superior mediastinal ganglion, pleural effusion on the right side, air bronchogram and a catheter that reached right cavities with the bilateral basal consolidation of right dominance were observed in the lung and mediastinal window.
The diagnostic radiology findings were the following:
- •
Tumor that infiltrates the gluteus minimus, part of the gluteus medius, obturator internus, iliacus, pubococcygeus, and puborectalis muscles
- •
Hepatomegaly
- •
Bilateral hydronephrosis
- •
Bilateral pulmonary consolidation of right predominance
- •
Pleural effusion
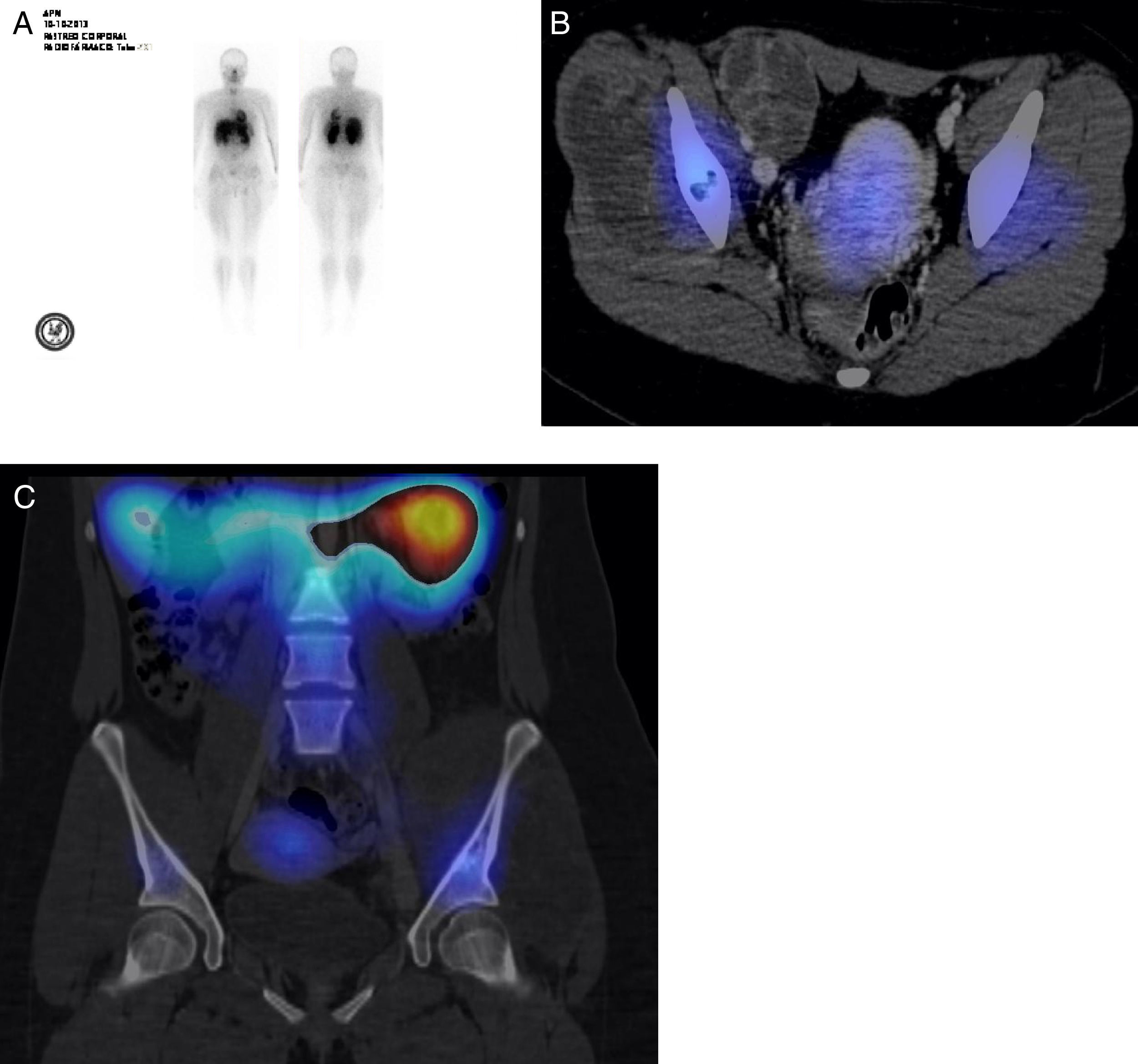
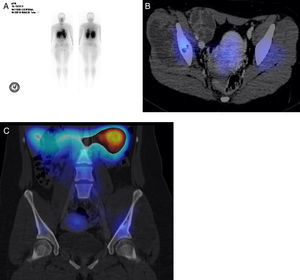
In this patient, with pelvic floor Ewing sarcoma diagnosis, thallium 201 SPECT-CT showed no images that suggested pulmonary metastasis. Due to an increased uptake (Fig. 6A), a SPECT-CT study with fusion was performed, where a part of the left iliac bone showed an increased uptake area (Fig. 6B). The bone injury showed no uptake, which suggested sites of necrosis. In the iliac bone, injured zones with no uptake were noticed (Fig. 6C). Multiple factors can influence thallium uptake, as tumor vascularization and metabolic rate, or cellularity. Thallium is effective for tumor detection and gives the possibility to differentiate among a residual tumor, a local recurrence, necrosis, or scarred fibrosis1. In patients with bone tumors, thallium has been used to evaluate the preoperative chemotherapy response and the correlation with the histological tumor grade and necrosis with positive and negative predictive values of 88 and 94, respectively2. It should be noticed that radiation levels to which patients are exposed to are extremely low (similar to those that patients absorb when a tomography, a PET or a SPECT are performed).
3Case presentationAccording to the medical history, the following syndromic diagnoses were established:
- •
Tumor symptoms supported by a progressively increased volume in the proximal third of the left thigh, which led to functional limitation
- •
During the evolution of the patient, a systemic inflammatory response syndrome was developed, supported by tachycardia, polypnea, and hypothermia
- •
Hemorrhagic syndrome, with thrombocytopenia and epistaxis
- •
Anemic syndrome characterized by paleness and hemoglobin and hematocrit levels below the normal values for the age
- •
Respiratory failure syndrome characterized by polypnea. Subsequently, the increase of the ventilatory deterioration required orotracheal intubation
- •
Infectious syndrome supported by neutropenia and hypothermia, with an abdominal cavity focal point
- •
Seizures with tonic-clonic movements, as well as a decrease in alertness
- •
Depressive syndrome characterized by increased sensitivity, sadness, and hopelessness
Accordingly, the following nosological diagnoses were integrated:
- •
Extraskeletal pelvic Ewing sarcoma versus rhabdomyosarcoma, due to a tumor syndrome with a histopathological report of small-blue-round-cell tumor, as well as the age and presentation site
- •
Neutropenic enterocolitis due to an infection syndrome, abdominal pain, distension, decreased fecal consistency, and image evidence of bowel wall thickening (ascending colon)
- •
Septic shock with systemic inflammatory response data, which required fluid (crystalloid) and vasopressor management
Initially, this patient presented with an increase in the volume of the left thigh and functional limitation for ambulation. The initial evaluation was at a hospital in Tucson, Arizona, where a biopsy of the lesion was performed and reported as a small-blue-round-cell tumor.
Differential diagnoses according to the clinical features and time of evolution of patients with soft tissue tumors may include a neoplastic etiology; for example, soft-part sarcomas, rhabdomyosarcomas, other sarcomas different from rhabdomyosarcoma, or primitive neuroectodermal tumors (bone or extraosseous origin). When signs such as erythema and functional limitation accompany the differential diagnosis, they should be considered as possible manifestations of soft tissue infection or osteomyelitis, especially when presented in this anatomical region. Symptoms such as progressive pain that causes functional limitation, as well as the increase in the volume, should be evaluated by a primary care physician, who must request an ultrasound study, in the case of soft tissue involvement, or a comparative X-ray study, in the case of bone condition, to refer immediately to a specialist. In the present case, a delay in referral to a specialist (one-month evolution of symptoms) was described. The family of small-blue-round-cell tumors represents a group of embryonal appearance neoplasms lacking precise morphological criteria that allow specific identification. This term defines tumors that involve the skeletal system as well as soft tissues and include different biological strains in children, adolescents, and young adults; within these tumors, Ewing sarcoma, rhabdomyosarcomas, neuroblastomas and lymphoblastic lymphoma, among others, are found. According to the age, clinical features, site of presentation, as well as imaging studies, a soft-part sarcoma, particularly an extraskeletal Ewing sarcoma was diagnosed. This tumor is present in a broad range of ages, from infants to older adults, with a peak of incidence in the second decade of life, such as the present case. It emerges with greater frequency in the skeletal tissue but also develops in soft tissues. Ewing sarcoma often expresses a balanced translocation, t(11;22) (q24; q12), involving the fusion of the EWS-FLI1 gene, which is described in 85% of patients. It has been mentioned that, at the time of diagnosis, up to 34% of the patients with skeletal Ewing sarcoma and 29% with extraosseous Ewing sarcoma present distant metastases, as reported in this case. A better prognosis is expected if the metastasis involves only the lung, in comparison with bone and bone marrow involvement. In the case Ewing sarcoma, metastasis is the major prognosis factor, followed by the size of the tumor3–6. A worse prognosis is considered if the size of the tumor is > 8cm or > 260cm3, as in this case. Also, the site of presentation (pelvic extremities show less response to the treatment) and the age are important factors. Age>15 years has been established as a poor prognosis for survival, which together with metastasis are the most important factors to consider. Multimodal treatment with chemotherapy, surgery, and radiation therapy has managed to increase the overall survival rate, from 10% to 50% at present. The diagnosis of rhabdomyosarcoma, a kind of neoplasm that is located within the category of tumors with small, round and blue cells, was considered as a second possibility. The latter is the most frequent tumor of soft tissues and represents approximately 3.5% of pediatric cancer. Although the most frequent primary sites are the head and the neck, 20% of rhabdomyosarcomas are present in the limbs, from which 80% of the patients are > 10 years of age (as in the present case). There are also various prognostic factors, such as age, the site of origin, resectability, metastases, and histopathology, among others. For the differential diagnosis, it is necessary to identify the characteristic myogenic lineage both by light and electron microscopy as well as immunohistochemistry and molecular biology. The identification of the characteristic rhabdomyoblasts, by light microscopy, and musculoskeletal proteins such as desmin, actin, myoglobin, Z-band based proteins and myosin, by immunohistochemistry, is essential to classify a rhabdomyosarcoma. In the case of Ewing sarcoma, S100 protein, neuron-specific enolase and CD99 are identified by immunohistochemistry. However, in this case, these studies were not available.
The patient received only three cycles of chemotherapy in five months since she developed secondary toxicity that led to infection complications. The chemotherapy scheme is of utmost importance since, in literature, cycles are recommended every 21 days, and local control is suggested to be achieved in a period no longer than 12 weeks, situation that was not feasible to establish in this patient due to multiple complications3.
During her evolution, the patient presented decreased fecal consistency, as well as pain and bloating. Radiology studies, ultrasound, and abdomen CT corroborated the increase of bowel wall thickness above 4mm; thus, neutropenic enterocolitis was diagnosed. This pathology can be secondary to chemotherapy toxic effects on the mucosa and intestinal muscle tissue, which cause bacterial invasion of the intestinal wall—secondary to neutropenia—decrease intestinal motility and cholestasis, among other mechanisms. Although no microbial isolation was reported, the mainly associated agents include Clostridium difficile, Pseudomonas aeruginosa, Escherichia coli, and Enterobacter. This complication is a morbidity and mortality factor of utmost importance in the pediatric population. Clinical diagnosis is supported by radiology with an ultrasound image. The use of CT allows diagnosis confirmation and additional associated complications.
A drug dosage adjustment was required due to the increase in creatinine levels. Data suggested renal tubulopathy (RT), for which phosphorus, magnesium and potassium supplementation was required. Many factors might influence RT, such as sepsis and nephrotoxic drugs, as well as those antimicrobials and chemical therapeutic agents used. Although cyclophosphamide may cause changes at a renal level (such as tubular necrosis), it is uncommon, and much less feasible with the dose that the patient received. Therefore, it is more likely that these changes were secondary to sepsis.
Finally, she presented seizures. Etiologic factors can be considered in this case. Due to the thrombocytopenia, a possibility could be that the intracranial hemorrhage might have conditioned neurological alterations, at least in part. However, drugs that can cause neurological disorders such as cyclophosphamide, which is considered as a drug that can condition encephalopathies, were used. The manifestations are diverse and include alterations of consciousness, psychomotor agitation, convulsive crisis and cerebellar symptoms. Most symptoms and signs are present in a dose-dependent manner. In this case, a strong dose of 4.1g/m2SC was used. The evidence of a previous kidney disease predisposes the risk. Another drug that produces encephalopathy is vincristine, although peripheral polyneuropathy is a better-known consequence of its toxicity (distal onset and ascending evolution). It may manifest as a multiple mononeuropathy and affect some cranial nerves. The presence of nystagmus could be considered as secondary to demyelination of specific areas in the central nervous system or the optical nerve by the use of this drug. In this case, it was considered as a multifactorial origin encephalopathy.
The deterioration of the patient included infectious complications, which led to the administration of a wide spectrum of antibiotics. Subsequently, a fungal infection was developed. On several occasions, she presented data of severe sepsis and septic shock for which a crystalloid solution, amines and various antimicrobial schemes management (including amphotericin b, vancomycin, meropenem, ciprofloxacin, and amikacin) were required. Despite this treatment, she persisted with the symptomatology. Finally, the patient had a cardiac arrest. The final diagnoses were the following:
- •
Extraskeletal pelvic Ewing sarcoma versus rhabdomyosarcoma with lung metastasis
- •
Septic shock
- •
Neutropenic enterocolitis
- •
Respiratory failure
- •
Cause of death: septic shock and neutropenic enterocolitis
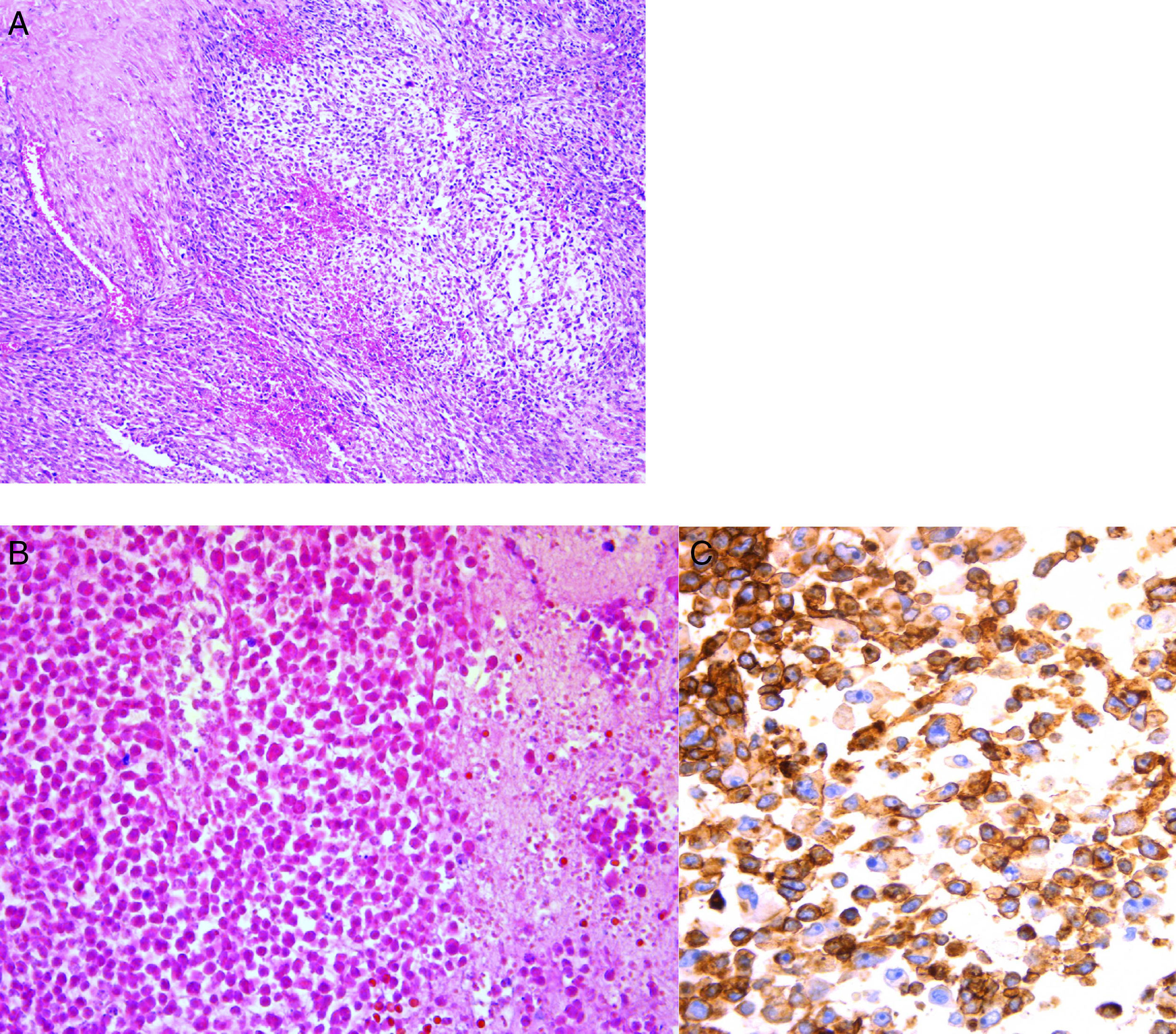
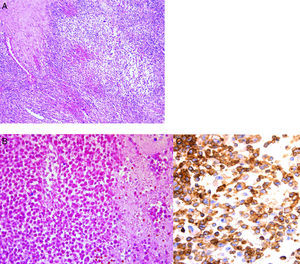
A postmortem study of an obese patient with generalized edema, more pronounced in the limbs, as well as areas extensive of ecchymosis in the chest and abdomen, was conducted. Bedsore by decubitus was present in the gluteal region. Microscopically, the tumor was constituted mostly by small cells of immature aspect that showed, in a panoramic view, a nodular form disposition. At higher magnification, it was observed that these cells were round, with round and hyperchromatic nuclei and scant cytoplasm (Fig. 7A). Other areas of necrosis with cell ghosts were identified (Fig. 7B). Necrosis corresponded approximately to 50% of the studied tissue. It is essential to complete the study of small, round and blue cell tumors with immunohistochemistry. In this case, CD 99 antibody was used. The reaction was positive on the membrane and diffuse approximately in 99% of the neoplastic cells (Fig. 7C). FLI1 antibody, which is a nuclear marker, also was used. A broad panel of antibodies was analyzed by immunohistochemistry to discard other tumors present. Morphological and immunohistochemical findings supported the diagnosis of Ewing sarcoma/peripheral primitive neuroectodermal tumor. As stated earlier, these neoplasms correspond to a clinical and pathological spectrum of the same entity, with histopathological, immunohistochemical and genetic common features based on the t(11;22) translocation. This family of tumors includes entities earlier known as Ewing sarcoma of bone, extraosseous Ewing tumor, peripheral primitive neuroectodermal tumor of soft tissues and Askin's sarcoma.
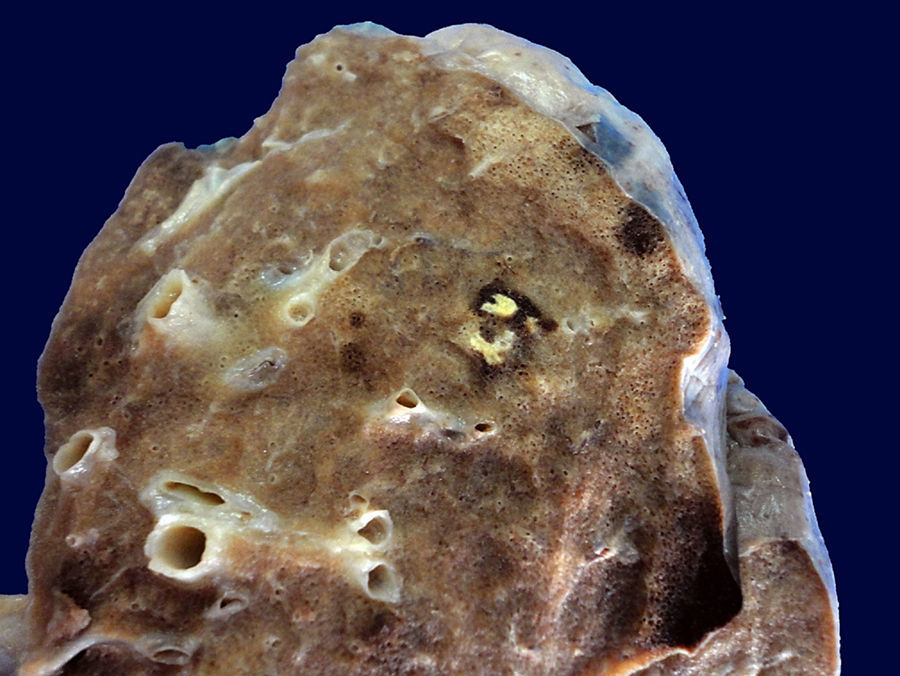
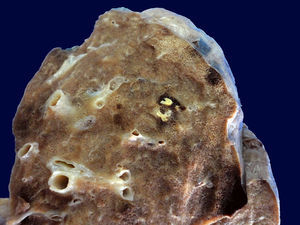
The surface of the lungs showed dark brown areas corresponding to hemorrhage, which affected 70% of the pulmonary parenchyma. A well defined nodular white lesion surrounded by a dark brown ring of bleeding was identified, which microscopically corresponded to a metastatic nodule (Fig. 8).
Edema and inflammatory infiltrate in other areas within the bronchi and bronchioles, as well as in the alveolar spaces were observed, which mainly corresponded to lymphocytes.
The macroscopic appearance of the esophagus showed a diffuse condition with areas of ulceration, hemorrhage, and fibrin adhered to the surface. Microscopically, an ulceration of the epithelium with necrosis, attached fibrin, edema, and fibrosis with the presence of coccoid bacteria was observed. No other microorganisms were identified. The larynx showed extensive areas of ulceration and bleeding.
Hypocellular bone marrow with a decrease of the three hematopoietic series was observed. The myeloid series was diminished, and megakaryocytes were not identified. Stroma had no fibrosis. However, edema and an important hemorrhage were present.
The heart showed petechial hemorrhage in the epicardium. Histology sections of the left ventricle showed mild hypertrophy, which was confirmed microscopically. Large cardiomyocyte cytoplasm and hyperchromatic pleomorphic nuclei were observed.
The liver showed increased weight, granular aspect and reddish-brown darkened areas alternating with clearer areas, which microscopically corresponded to congestion.
The small intestine folds were preserved, and the mucous membrane showed vascular congestion. The colon presented edema and dilated areas; the intestinal mucous presented no alterations.
Both kidneys kept the medulla-cortex ratio, with a slight dilation of the pyelocaliceal system. Microscopically, vascular congestion of medullar prevalence and acute tubular necrosis data were identified.
The study of the brain showed congestion of the meningeal vessels. Hemorrhage areas or metastases were not identified.
4.1Final diagnosesEwing sarcoma/extraskeletal peripheral primitive neuroectodermal tumor with lung metastases and changes after treatment.
4.2Concomitant alterations- •
Toxic damage to bone marrow
- •
Acute ulcerative esophagitis
- •
Ulcerative acute laryngotracheitis
- •
Acute bilateral pneumonia
- •
Congestive hepatomegaly
- •
Mild hepatic cholestasis
- •
Liver and spleen hemosiderosis grade III
- •
Cerebral edema
- •
Shock
- •
Acute alveolar injury
- •
Acute tubular necrosis
- •
Hypoxic-ischemic visceral myopathy in the gastrointestinal tract and bladder
Pulmonary hemorrhage with postmortem negative cultures.
5Final comments5.1OncologyExtraskeletal or bone primitive neuroectodermal tumors are highly aggressive neoplasms, for which the treatment is intense. Previously, it was mentioned that the patient received only three cycles of chemotherapy in approximately five months. The administration of an intense scheme was required due to the location, size of the tumor and age of the patient, which meant giving the permissible highest doses of these schemes—approved internationally. Moreover, the cyclophosphamide doses administered were very close to those used in hematopoietic progenitor cell transplantation. The scheme of treatment for these tumors consists of three cycles of chemotherapy alternating every three or four weeks, depending on the tolerance of the bone marrow; myelosuppression is expected up to 28 days at most. Three high-dose drugs were used, including cyclophosphamide at a total dose of 4.1g per cycle. Assuming that it was the ninth week of treatment, the patient was close to being evaluated, which was impossible due to her death. However, the prognosis factor for necrosis of 50% was very poor since > 90% of necrosis is expected to consider an appropriate response to chemotherapy. The reason for which the chemotherapy scheme was not modified was that the most intense scheme to treat this type of tumors in this location and age group was already being used.
5.2Oncology surgeryAs stated before, this was a high-risk tumor due to both its poor response to treatment and its location and size. Although the SPECT/CT scan did not show any significant alterations in the iliac bone thickness, the surgical plan would have required a wide resection, including part of the iliac bone to reduce the risk of local relapse, an inguinal node dissection, and radiotherapy consolidation. Due to the response, it might have been necessary to include also hematopoietic cell transplantation once the disease was controlled, including the pulmonary metastasis. This case represented a surgical challenge since the technique involves the removal and reconstruction of the pelvis.
5.3Psychiatry and Adolescent MedicineEmotional factors can determine the evolution and outcome of almost all diseases. In the case of cancer patients, psychopathological problems are closely related to pain and some other symptoms. Certainly, cancer patients are those who present the highest psychopathology rates from all the hospitalized patients. In the present case, the prognosis was poor since some factors that predict the presence of psychopathology are associated with the nature of the tumor as well as a prior psychopathology in the family.
5.4Intensive careThe management of these patients in the Intensive Care unit is for support. It consists of a contact phase, regardless of the pathology of the child, to whom all the support is provided until the first phase of the treatment is completed and the prognosis is determined. Following the first phase, together with the service treating the patient, it is decided whether the child is a candidate for entering therapy—regardless of the response to the treatment. Under this circumstance, mainly the Oncology and Surgical Oncology departments determine if the patient requires the support of the Intensive Care unit, which in turn determines the admittance of the patient based on the information that both medical and surgical oncologists provide. In the case of being admitted, the type of support needed is decided. In this case, the patient did not finish the first phase of the treatment, for which all the possible assistance and the chance to overcome the disease were provided. This policy of the Intensive Care Unit at the Hospital Infantil de Mexico Federico Gomez has lasted for 20 years. Proudly, this Intensive Care Unit was the first in the country to receive pediatric patients with cancer and continues with very good results to this day.
5.5Palliative careThis patient is a clear example of the problems that cancer patients face at present since it is very difficult to declare a patient as incurable with the current therapeutic resources. The possibility of a good response to an appropriate treatment is always present. In addition, this situation was not only exemplified, but primarily psychological palliative care started although the patient was not declared as incurable since the treatment never ended. These aspects, besides the spiritual and pain control support, must apply to every cancer patient even though they are not declared as incurable.
In conclusion, the initial, early and timely diagnosis, and the multidisciplinary management of patients with muscle-skeletal system tumors are of the utmost importance since they affect the prognosis, survival, and quality of life.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare no conflict of interests of any nature.
Please cite this article as: López Sosa FH, Valadez MT, Cruz Contreras L, Perezpeña-Diazconti M. Sarcoma de Ewing extraóseo en una adolescente de 16 años. Bol Med Hosp Infant Mex. 2016;73:202–211.