Adnexal paraovarian cysts are not frequently seen during teen development, their incidence is around 10% and usually benign.
Clinical caseAdolescent female 15 years old with no pathological family and personal history relevant to her current condition. Chief complaint: six months ago she complained with abdominal pain in meso, hypogastrium and right iliac fossa. Later, she observed an increased volume on her lower quadrant of the abdomen, mostly on her right side. During physical examination an abdominal tumour was palpated. By an abdominal-rectal manoeuvre, the presence of tumour was confirmed and located in front of the rectum and no implants. Imaging studies confirmed a paraovarian cyst.
She underwent on surgical laparotomy and a paraovarian cyst was found. The histological diagnosis was a cystadenoma.
The postoperative course was satisfactory.
DiscussionEpidemiological data and ultrasonographic findings are examined to confirm the diagnosis of paraovarian cyst. The laparoscopic treatment for adnexal problems is described.
En la adolescencia el desarrollo de los quistes paraováricos anexiales son poco frecuentes; su incidencia es del 10% y generalmente son benignos.
Caso clínicoAdolescente femenino de 15 años de edad, sin antecedentes familiares y personales patológicos de importancia para su padecimiento; este fue de 6 meses de evolución, con dolor abdominal en meso e hipogastrio y fosa iliaca derecha, acompañado de estreñimiento de hasta 3 días y de un aumento de volumen en su parte baja del abdomen, apreciándose más en el lado derecho. En el examen físico se corroboró la presencia de tumour abdominal, y con la maniobra abdominorrectal se palpó un tumour por delante del recto y sin implantes. Los estudios de imagen ratificaron la presencia de un tumour de anexos del lado derecho.
Se practicó laparotomía encontrándose quiste paraovárico del lado derecho, el cual se resecó en su totalidad. El diagnóstico histológico fue de un cistadenoma.
La evolución postoperatoria fue satisfactoria.
DiscusiónSe discuten algunos datos epidemiológicos y los signos ultrasonográficos que ratifican la presencia del quiste paraovárico, y se menciona brevemente el tratamiento laparoscópico para esta patología.
Paraovarian cysts rarely develop in adolescents; their incidence is 10%, and they are generally benign. Their growth is slow and progressive, although occasionally they can increase rapidly in size. The most common symptoms are pain in the lower abdomen, which can be transient or intermittent. Large cysts can compromise the digestive and urological tracts; some patients experience mild constipation. They are diagnosed clinically and diagnosis is validated by ultrasound. This condition is usually treated surgically.1
We treated an adolescent with a par ovarian cyst which motivated us to present her case and perform a short review of the literature.
Clinical caseAn adolescent girl aged 15 years with no family or personal history of relevance. Her immunisation schedule was incomplete and she reported no allergies or previous surgical procedures. She started menstruation at the age of 13, and her periods were currently regular.
The disorder had started 6 months previously, with transient abdominal pain, located in the mesentery, hypogastrium and right iliac fossa, with constipation for up to 3 days. A month ago she noticed increased volume in the mesentery and hypogastrium that was more pronounced towards the right side of the abdomen. She had no urinary symptoms and did not have a fever.
Physical examination: a female patient with correct body development and oriented×3. Her secondary sexual characteristics corresponded to her age of 15 years according to the Tanner scale (stage 5).
Her vital signs were normal, BP 110/75mmHg, weight 55kg. No alterations were found on cardio-pulmonary examination, heart sounds were normal and no murmurs were detected.
Abdomen: there was increased volume in the lower part covering the mesentery, hypogastrium and right iliac fossa, and the fundus was above the umbilical scar; the surface was smooth, not very mobile and not painful; peristalsis was normal. A tumour was palpated in front of the rectum by abdominorectal examination; no implants were found (Fig. 1). There was no discharge of fluid or traces of blood via the vagina.
No abnormal data were found in the extremities or nervous system.
Laboratory test results were normal.
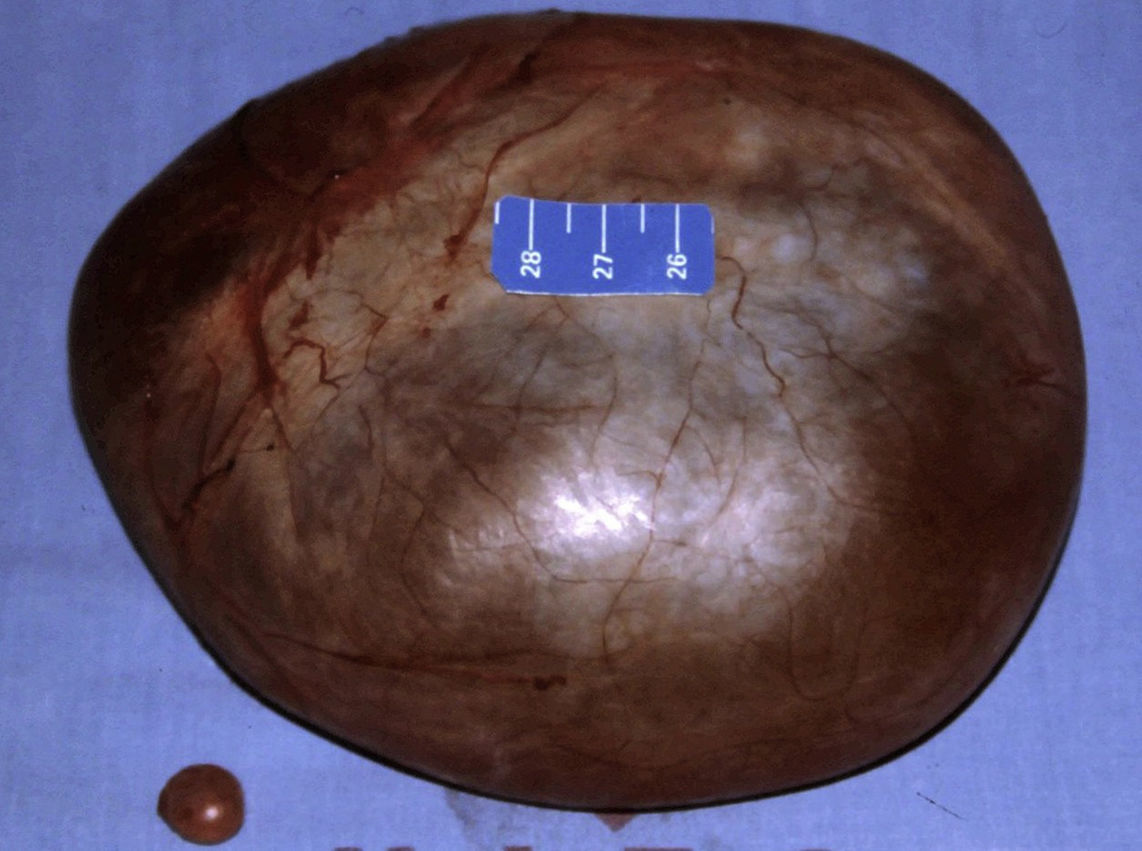
Abdominal ultrasound revealed a right-sided, thin-walled paraovarian cyst containing non-haemorrhagic fluid. The tumour was displacing the uterus towards the left and compressing the upper part of the bladder. The ipsilateral ovary showed no apparent alterations (Fig. 2).
Enema examination of the colon showed that the cyst was exerting pressure on the small bowel-ileum and displacing the sigmoid colon to the left and backwards (Fig. 3).
Shortly afterwards a laparotomy was performed under general anaesthetic with an infraumbilical transverse incision, revealing the right-sided tumour, compressing and displacing the uterus to the left. Immediately after opening the peritoneal covering the entire tumour was dissected and resected by blunt dissection. A small cyst (Morgagni's hydatid) was found on the left side and was removed. There were no complications (Figs. 4 and 5). The postoperative diagnosis was a paraovarian cyst.
The histopathological study described the surgical specimen as a 14cm long, thin and fibrous-walled and transparent cyst, covered by columnar epithelium and fibrous tissue. The fluid was clear and serous in appearance and the amount was not measured. A second check showed clear coffee coloured intracystic tissue as well, 5cm×5cm in length, papillary shaped and short in height. The histological diagnosis was paraovarian serous cystadenoma.
The patient made satisfactory postoperative progress and was discharged in a good general condition. At one-year follow-up, she remained asymptomatic and her psychomotor development and weight were normal for her age.
DiscussionParaovarian cysts are located in the broad ligament between the Fallopian tube and the ovary. Histologically, 68% are mesothelial in origin, 30% embryonic remnants of paramesonephric ducts and 2% of mesonephric ducts. They constitute 10% of adnexal lesions, and present in 3% of all gynaecological emergencies.2,3
As the condition progresses clinically, patients experience digestive symptoms in the majority, such as a heavy feeling in the lower abdomen and pain, which can be mild, transient or occasionally frequent, but tolerable. Other young women report urinary symptoms such as frequency, sometimes accompanied by fever.
A small number of adolescents start with an acute abdominal infection and then complications can arise such as intracystic haemorrhage, perforation of the cyst with haemoperitoneum, or torsion of the tumour or Fallopian tube on the same side.3–6
Ultrasound is of great use in confirming the clinical diagnosis of paraovarian cysts. In this case, ultrasound showed characteristics of benign disease and the signs were: ovoid in shape with thin capsular echotexture 3mm thick, with hypodense fluid that was not measured, located in the upper part of the ovary and below the Fallopian tube.1
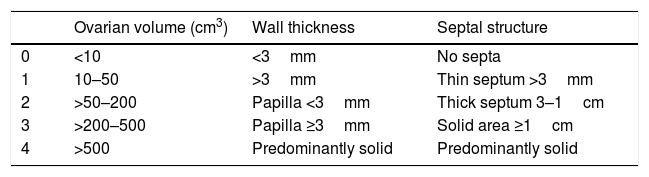
The pathological description of our case referred to papilliform tissue attached to the inner part of the cyst; this needs to be taken into account since tumours such as cystadenocarcinoma and papillary carcinoma have been reported arising from this tissue. This is why ultrasound should be performed by an experienced radiologist able to observe these structures, nodular or papillary tissue. Preoperative ultrasound can be very helpful according to Dr Priest, who uses it for ovarian tumours. This system takes into account the measurement and thickness of the cystic capsule, fluid volume, septations and intracystic tumour tissue7 (Table 1).
Differential diagnosis of paraovarian cyst should include, inter alia, some of the following disorders: intestinal duplication, internal hernias, intestinal lymphangioma and peritoneal inclusion cysts.8,9 Complicated appendicitis of several days’ onset, hydrosalpinx, ovarian torsion and ectopic pregnancy can be causes of acute abdomen.
Open surgery for patients with paraovarian cyst is still performed in some institutions with fewer resources and fewer expert personnel, as in the case we present. Currently laparoscopic surgery is usually performed in institutions with specialist practitioners and teams, this causes the patient less trauma with better outcomes. This procedure does not require bowel preparation and the bladder is emptied using a catheter once the patient has been anaesthetised. Three ports of 5mm and 3mm are placed; the camera port is situated in the umbilical scar, one of the other two ports placed in the right lower quadrant and the other in the left lower quadrant. If necessary, another supraumbilical port can be created. Once the internal anatomy has been observed, a window is opened in the broad ligament in the uppermost part of the cyst over the area of the mesosalpinx using bipolar electrocautery, which enables us to dissect around the entire cyst until reaching the fundus and then to resect it neatly. Occasionally large cysts are punctured to empty their content and achieve a good dissection. Once the cyst has been removed, the anatomy of the ligament, ovaries and Fallopian tubes is checked and they are returned to their usual location.10
All medical tasks must be handled with a hefty dose of humanism. We must be mindful that we live in an increasingly demanding society where doctors are required to maintain their continuous professional education.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Felipe JH, Alcantar AR, Franco RF. Adolescente con quiste paraovárico. Tratamiento quirúrgico. Cir Cir. 2017;85:535–538.