Optical coherence tomography is a useful tool in several diseases. Its intraoperative use with the intention of improving anatomical results has recently been described.
PurposeTo determine the usefulness and safety of optical coherence tomography during pars plana vitrectomy for several vitreoretinal diseases.
Material and methodsA prospective case series is reported, in which the decision that influenced the use of the optical coherence tomography imaging during pars plana vitrectomy is evaluated. A RESCAN 700 microscope that includes a spectral domain tomography was used to obtain the images. At the end of each procedure the surgeons completed a questionnaire to determine if the tomographic image had an influence when making decisions during the surgery, or change the decision during the procedure.
ResultsThirteen patients with pars plana vitrectomy were included, with cataract surgery also performed in 6 patients. The surgeon considered that the intraoperative image influenced the decision during the procedure in 8 cases.
ConclusionIntraoperative optical coherence tomography is helpful for a safe patient diagnosis. It does not affect the surgery time, and in some cases it is useful for optimising the procedure in vitreoretinal surgery.
La tomografía de coherencia óptica es una herramienta diagnóstica de gran utilidad en diversos padecimientos. Recientemente se ha descrito su uso transquirúrgico, con la intención de mejorar los resultados anatómicos.
ObjetivoDeterminar la utilidad y seguridad de la tomografía de coherencia óptica transquirúrgica, en el tratamiento de cirugías de retina y vítreo.
Material y métodosSerie de casos prospectiva. Se evalúa la influencia que tiene la imagen de tomografía de coherencia óptica en la toma de decisiones, durante la vitrectomía vía pars plana. Para la obtención de imágenes se utilizó RESCAN 700, un microscopio que cuenta con un tomógrafo de dominio espectral integrado. Al final de cada procedimiento, los cirujanos contestaron un cuestionario para determinar si la imagen tomográfica influyó en la toma de decisiones durante la cirugía.
ResultadosFueron intervenidos 13 pacientes mediante vitrectomía pars plana; en 6 de ellos se realizó también cirugía de catarata. En 8 casos, el cirujano consideró que la imagen transoperatoria influyó en la toma de decisiones durante el procedimiento.
ConclusionesLa tomografía de coherencia óptica transquirúrgica es un auxiliar diagnóstico, seguro para el paciente, que no influye en el tiempo quirúrgico y que en algunos casos es de utilidad para la optimización del procedimiento en cirugía vítreo-macular.
In recent years optical coherence tomography (OCT) has come to play a highly important role in eye and vitreous diseases, as its capacity to provide high resolution tomographic images of biological tissues1–3 has made it possible to gain better understanding of the physiopathology of a large number of illnesses. It also permits making early diagnoses, determining prognostic factors and, very importantly, in many cases it offers the guideline for decision-making in the follow-up of pathologies which affect the macula as well as the vitreoretinal interface.4–7
Devices have been developed that make it possible to use this technology in the operating theatre to better understand the behaviour of tissue and the affect of manipulating it during surgery. This aims to maximise surgical performance and thereby offer patients better anatomical and visual results.8,9
Transurgical OCT has been reported to be useful in a wide range of procedures. These include macular holes, epiretinal membrane, optic nerve pit and the vitreomacular traction syndrome, as well as anterior segment procedures such as cataract surgery and penetrating keratoplasty.10–14
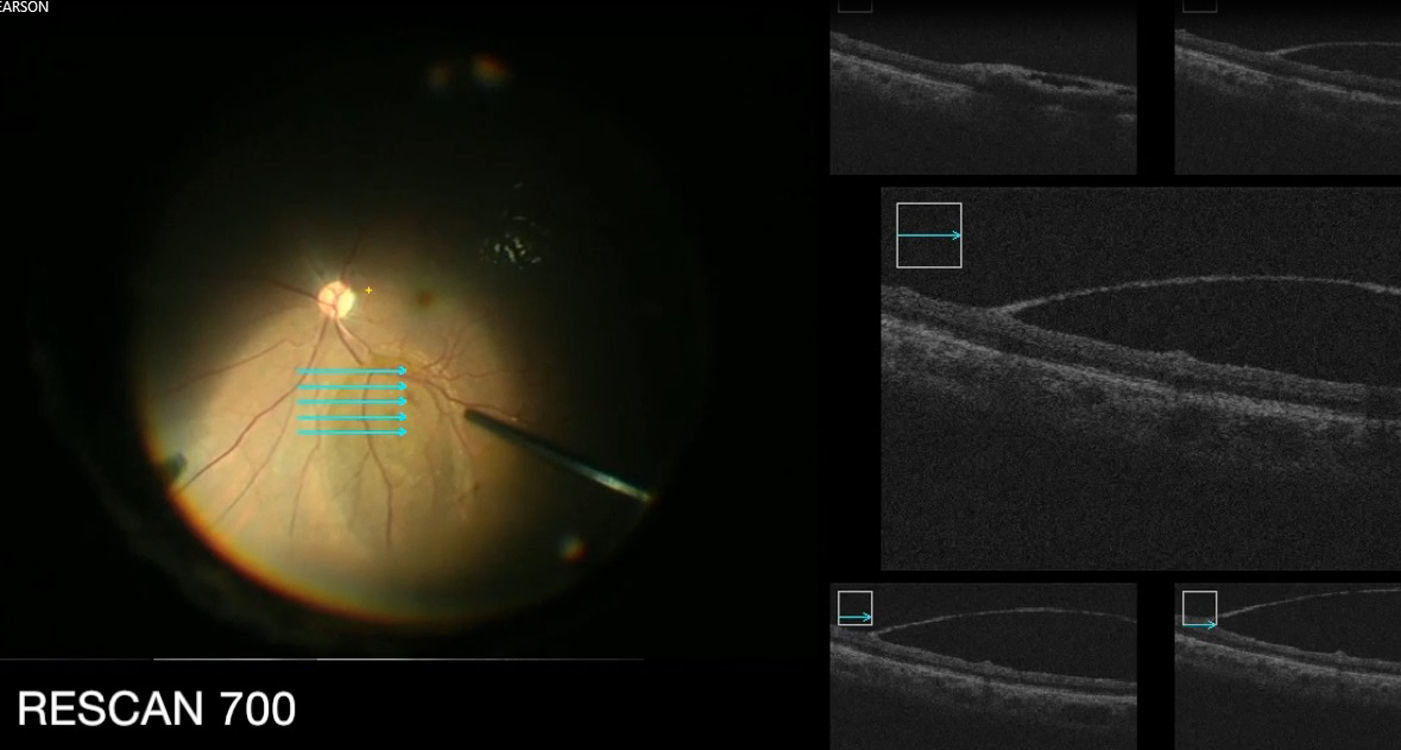
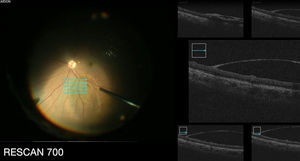
Studies have been reported that show the usefulness of a spectral domain OCT (SD-OCT) device mounted as an accessory on the surgical microscope. Another option for this purpose is the RESCAN 700 (Carl Zeiss Meditec, Germany), a visual domain tomograph included in the surgical microscope. This makes it possible to obtain images in real time and permits interaction with the X–Y functions of the microscope pedal to centre the image.8
The aim of this study is to determine the utility and safety of transurgical OCT in retina and vitreous humour surgery.
Material and methodsThis is a prospective series of cases. The study was conducted in 2 hospitals in Mexico during September and October 2015. The procedures were performed by 3 surgeons experienced in retina and vitreous humour surgery. All of the patients operated for conditions of the vitreous humour or retina were included, regardless of whether or not they also received cataract surgery. The Constellation Vision System (ALCON) platform was used for the surgical procedure, which used calibre 23 and 25. For correct visualisation of the epiretinal membrane and the internal limiting membrane (ILM) trypan blue and brilliant blue stains were used, respectively.
The RESCAN 700 system was used to obtain images. This microscope contains integrated OCT as well as an interactive screen system, an external display panel and the pedal to control the OCT scanner. This system is based on the Lumera 700 platform (Carl Zeiss Meditec).
During the procedure a compound stereoscopic image is projected consisting of the view through both microscope eyepieces. This makes it possible for the surgeon to identify the site being analysed by tomographic analysis. This image may be projected in 2 different ways: one in the form of a cross representing the X–Y axes, while the other consists of 5 lines showing 5 parallel slices at different levels. For this the X–Y function of the microscope pedal is replaced by control of the stereoscopic image that indicates the site of tomographic analysis. To visualise the posterior segment the RESIGHT non-contact lens system was used.
At the end of each procedure the surgeons answered a questionnaire to determine whether the OCT transurgical image had influenced their decision-making during the procedure, and whether the OCT transurgical image had led them to change their decision during the procedure.
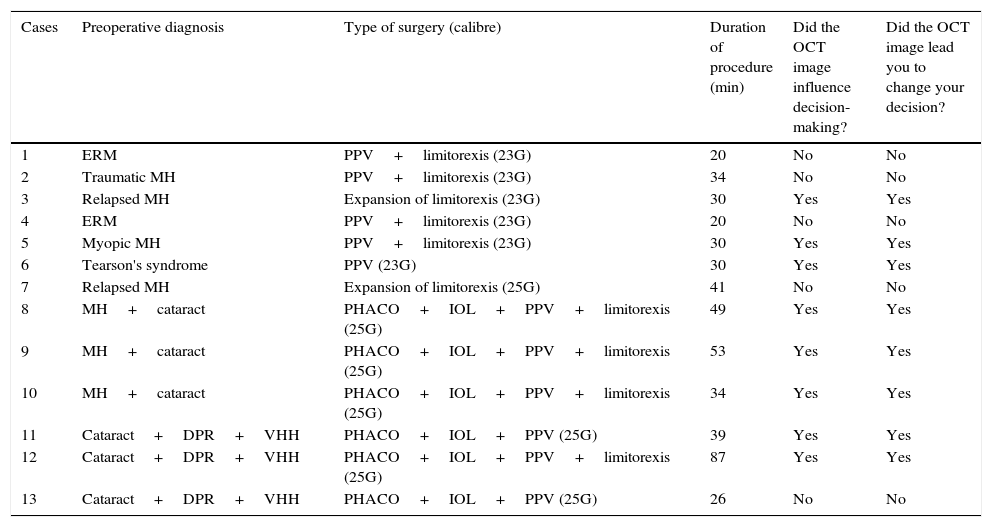
Results13 patients were included in the study, 8 women and 5 men aged from 16 to 70 years old. In 6 of the 13 cases combined cataract and retinal surgery was performed. In the solely vitreoretinal cases surgery lasted for an average of 29min (range 20–41min) while in the cases of combined surgery the operation lasted for an average of 48min (26–87min). Detachment of the rear vitreous humour was induced in all of the cases, and brilliant blue was used to stain the limiting external membrane while trypan blue was used in cases of epiretinal membrane (Table 1).
The clinical characteristics of the patients and remarks by the surgeons on the usefulness of transurgical optical coherence tomography.
| Cases | Preoperative diagnosis | Type of surgery (calibre) | Duration of procedure (min) | Did the OCT image influence decision-making? | Did the OCT image lead you to change your decision? |
|---|---|---|---|---|---|
| 1 | ERM | PPV+limitorexis (23G) | 20 | No | No |
| 2 | Traumatic MH | PPV+limitorexis (23G) | 34 | No | No |
| 3 | Relapsed MH | Expansion of limitorexis (23G) | 30 | Yes | Yes |
| 4 | ERM | PPV+limitorexis (23G) | 20 | No | No |
| 5 | Myopic MH | PPV+limitorexis (23G) | 30 | Yes | Yes |
| 6 | Tearson's syndrome | PPV (23G) | 30 | Yes | Yes |
| 7 | Relapsed MH | Expansion of limitorexis (25G) | 41 | No | No |
| 8 | MH+cataract | PHACO+IOL+PPV+limitorexis (25G) | 49 | Yes | Yes |
| 9 | MH+cataract | PHACO+IOL+PPV+limitorexis (25G) | 53 | Yes | Yes |
| 10 | MH+cataract | PHACO+IOL+PPV+limitorexis (25G) | 34 | Yes | Yes |
| 11 | Cataract+DPR+VHH | PHACO+IOL+PPV (25G) | 39 | Yes | Yes |
| 12 | Cataract+DPR+VHH | PHACO+IOL+PPV+limitorexis (25G) | 87 | Yes | Yes |
| 13 | Cataract+DPR+VHH | PHACO+IOL+PPV (25G) | 26 | No | No |
MH: macular hole; PHACO: phacoemulsification; VHH: vitreous humour haemorrhage; IOL: intraocular lens; ERM: epiretinal membrane; OCT: optical coherence tomography; DPR: diabetic proliferative retinopathy; PPV: pars plana vitrectomy.
Regarding the questions surgeons were asked about the influence of the OCT image on decision-making during the operation, in 8 cases they replied that the image had influenced their decisions. In case number 3, which was a relapsed macular hole, an expansion of the limitorexis had been planned; however, when the scan was performed remnants of the internal limiting membrane were found to still exist around one of the edges of the hole. The surgeon therefore changed his decision to solely increase the limitorexis and decided to complete it in the centre of the hole.
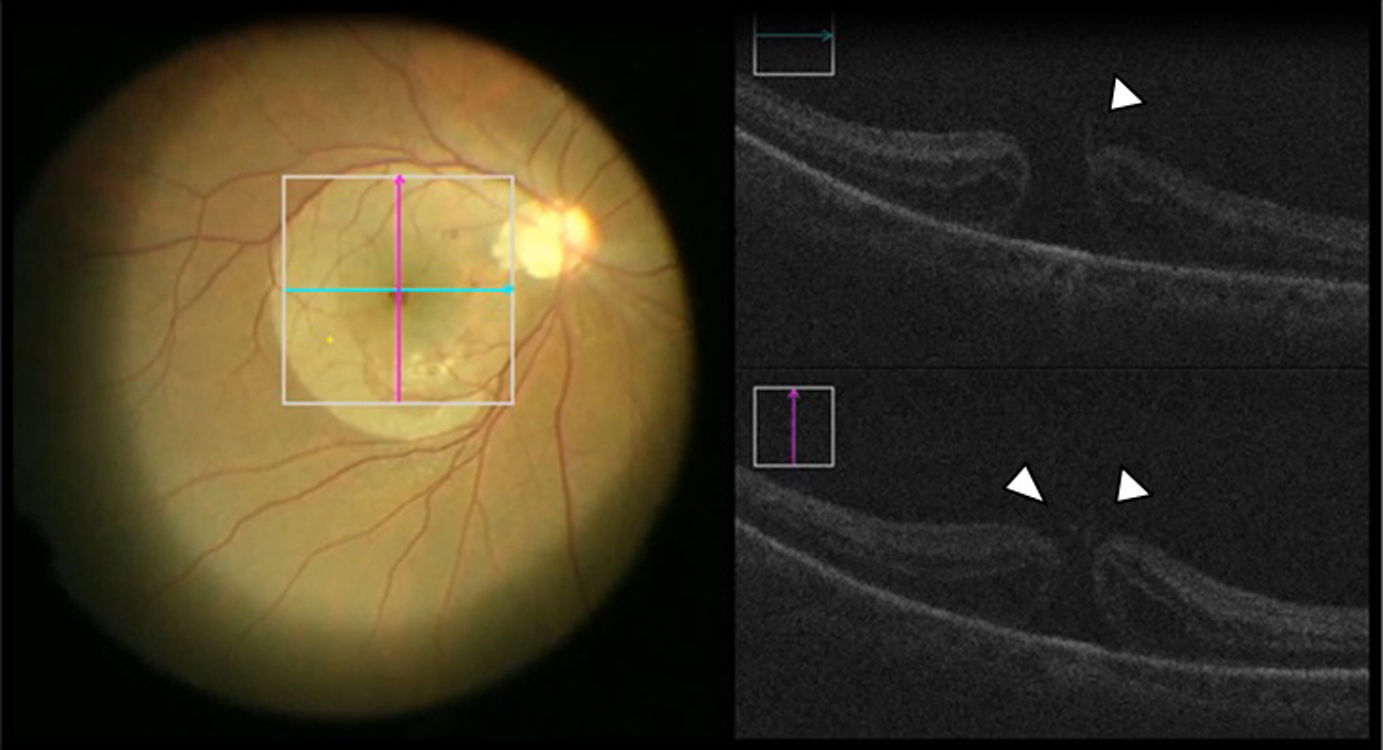
Case number 5 was a macular hole in a female patient with degenerative myopia; the internal limiting membrane was stained with brilliant blue and limitorexis was performed, which the surgeon believed was complete. Nevertheless, when the scan was made partially raised internal limiting membrane was found to remain on one of the edges, so the decision was taken to complete its removal (Fig. 1).
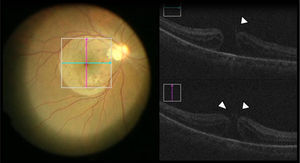
Case number 6 was a young female patient with Tearson's syndrome and grade III vitreous haemorrhaging. When the rear vitreous humour was detached an image persisted above the retina which seemed to be the hyaloid membrane; however, when the scan was performed it was found to be the limiting internal membrane which was raised in the form of a dome. This was therefore deduced to be the place where a sublimiting haemorrhage had occurred, and which had been absorbed prior to the surgery. Due to this the surgeon decided not to cut or manipulate the site any more (Fig. 2).
Cases 8, 9 and 10 consisted of macular holes in which, after performing limitorexis and air exchange, the hole seemed to continue open; nevertheless, when the OCT scan was performed the edges were found to have joined, so that the surgeon decided to end the procedure.
Case 11 was a male patient with diabetic retinopathy and vitreous humour haemorrhage, in which the macula could not be evaluated before surgery. After the vitrectomy the macular area seemed to be thickened; however, the OCT image ruled out the presence of a macular oedema, so that the surgeon decided not to perform limitorexis. Contrary to this, although in case number 12 the surgeon had not considered limitorexis in a diabetic patient, the OCT image showed intraretinal cystic spaces. The surgeon therefore applied brilliant blue and carried out limitorexis.
DiscussionTechnical advances in ophthalmology have helped to increase the understanding of the physiopathology of several diseases, as well as the development of treatment options that improve the functional prognosis of patients. Obtaining high resolution tomographic images in real time may contribute to this process.
There are cases in which transurgical OCT may be of greater utility, mainly macular complaints; we take cases 3 and 5 as examples, in which limitorexis seemed to be complete. However, there was still internal limiting membrane around the edges of the hole, so that the surgeon decided to remove it. It is known that in this pathology complete limitorexis must be carried out and that the edges of the hole must be checked, as otherwise the probability of the hole closing is reduced.15,16
Another example is the case of the epiretinal membranes. The need has been described to remove not only the membrane but also the internal limiting membrane, to prevent relapse.17–19 There are also cases of macula hole associated with rhegmatogenous retinal detachment, in which the presence of epiretinal membranes has been observed; in these cases it is indispensable to completely remove the epiretinal membrane, as if any remnants are left they may contract after surgery and make it more probable that the hole will re-open and therefore lead to failure of the surgery.20,21
Vitrectomy has been considered to be a therapeutic option for diabetic macular oedema, as it reduces angiogenic and proinflammatory factors.22 Studies have been performed which indicate that limitorexis in these patients to achieve decompression and dispersion of the intraretinal extracellular fluid into the cavity of the vitreous humour aids the resolution of the oedema.23,24 However, we know that one of the main indications for vitrectomy in patients with diabetic retinopathy is the presence of vitreous haemorrhage, which make it impossible to evaluate the condition of the macula before surgery. Transurgical OCT in these patients supplies the doctor with valuable information about the state of the macula and allows him to take the decision to perform limitorexis, as occurred in case 12 of our series.
There are stains such as trypan blue, brilliant blue, indocyanine green and triamcinolone, among others, that are highly useful for surgeons, given that they make it possible during surgery to view structures such as the vitreous humour, the internal limiting membrane and the epiretinal membranes. Their use has been associated with a higher rate of anatomical success.25,26
Nevertheless, cases exist in which the desired anatomical and functional results are not achieved, even though a perfected surgical technique has been performed. In these case transurgical OCT may help to clarify the causes that influenced the poor evolution of the patients in question. Cases 3 and 5 are examples of this, as in them and in spite of using brilliant blue it was impossible to identify the small remnants of internal limiting membrane that would have remained adhered to the edge of the macular hole if it were not for the OCT image.
As the images projected in the eyepieces of the microscope are stereoscopic, this prevents them from interfering with visualisation of the retina. They do not therefore interfere with the proper undertaking of the procedure.
Another advantage of the device is that the image is obtained in real time as a continuous video. It can be seen by the surgeon through the eyepieces and by other members of the surgical team on the screen included in the microscope. This is important, given that the time out arising from using the device in minimum, thereby avoiding a prolongation of the duration of surgery.
One of the drawbacks associated with the device is that the X–Y function of the microscope pedal is replaced by control of the stereoscopic image, indicating the location of tomographic analysis. Another restriction of the device is that, when instruments are inserted into the area being analysed, they cause a shadow that makes it impossible to see the structures underneath the instruments.
The DISCOVER study is currently underway, and this has the aim of clarifying the benefits and limitations of a system which supplies OCT images in real time during ophthalmological surgery.8
An outstanding limitation of our study is the small number of patients it includes, and it also lacks treatment of a broader range of complaints. It will be necessary to perform studies with larger numbers of patients with a broader range of complaints to understand the role that transurgical OCT imaging should play.
ConclusionsTransurgical OCT is a useful tool that is able to influence decision-making during surgery. It optimises the anatomical results of several ophthalmological complaints, not only in special cases but also in procedures considered to be routine; however, it must not replace the judgement of the surgeon.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Ramírez-Estudillo JA, Sánchez-Ramos JA, Pérez-Montaño CR, González-Cortés JH. Utilidad transquirúrgica de la tomografía de coherencia óptica en cirugía vítreo-retiniana. Cir Cir. 2017;85:21–26.