ALPPS (associating liver partition and portal vein ligation for staged hepatectomy), in 2-stage liver resections, achieves hypertrophy of the functional liver remnant (FLR) in 7 days, and the objective of this technique is the occlusion of the intrahepatic collaterals. In March 2012 we published a new surgical technique associating the insertion of a tourniquet in Cantlie line and right portal vein ligation (ALTPS: associating liver tourniquet and right portal vein occlusion for staged hepatectomy). In this paper we present this ALTPS technique placing the tourniquet in the umbilical fissure to obtain hypertrophy of segments II–III. It was performed in a 51-year-old patient with a recurrent right renal hypernephroma which involved all the anatomic right lobe and inferior vena cava. Preoperative FLR was 380ml (20% of the total volume) increasing 150% at 7 days (to 953ml, 31% of the total). In the second step, we performed a right trisectionectomy and retrohepatic inferior vena cava resection, replacing it by a 2-cm-ring goretex graft.
Associating liver partition and portal vein ligation for staged (ALPPS) para las resecciones hepáticas en 2 tiempos, consigue la hipertrofia del volumen funcional residual (VFR) en 7 días, al ocluir las colaterales intrahepáticas entre ambos lóbulos. En marzo de 2012 publicamos una nueva técnica quirúrgica, asociando la colocación de un torniquete en la línea de Cantlie con ligadura portal derecha (Associating liver tourniquet and right portal vein occlusion for staging hepatectomy [ALTPS]). Ahora presentamos la técnica ALTPS en la cisura umbilical para hipertrofiar los segmentos II–III, realizada en un varón de 51 años con recidiva de hipernefroma renal derecho que invade todo el lóbulo derecho y la vena cava inferior. El VFR preoperatorio fue de 380ml (20% del total) y aumentó un 150% a los 7 días (a 953ml; 31% del total). En el segundo tiempo se realizó trisectorectomía derecha con resección de la vena cava inferior retrohepática, siendo sustituida por un injerto de goretex anillado de 2cm de diámetro.
In extensive resections or in two-stage liver resections (TSLR),1,2 when there is insufficient residual functional liver volume (RLV), percutaneous portal vein embolisation (PPVE)3,4 or intraoperative portal vein ligation (IPVL) is performed.5–7 There are several problems associated with portal vein occlusion in both procedures: delayed (between 3 and 8 weeks) or no hypertrophy,3–7 due to the formation of intrahepatic collateral circulation (with a danger of posthepatectomy liver failure8,9 (PLF following major liver resection) and progression of the tumour,10,11 which could result in the patients becoming inoperable. In 2011, Baumgart et al.12 reported 3 patients with RLV in the left lateral sector treated with right portal vein ligation and in situ bipartition at the level of the umbilical fissure, achieving RLV hypertrophy of segments II–III in 9 days, in order to perform a TSLR and obtain right trisectionectomy. The same results were reproduced by other authors13,14 by sectioning in the Cantlie line, using the same technique. This new technique, called associating liver partition and portal ligation for staged hepatectomy (ALPPS),15 is a great step forward because it achieves quick hypertrophy and could prevent the classical occlusion technique problems of hypertrophy failure and tumour progression. This technique has not, however, been universally accepted because the first-stage surgery is very aggressive and there is a high rate of morbimortality (12%–27%)16–21 and some authors consider there is high risk of PLF.16–20 In September 2011 we performed a new alternative surgical technique, where we inserted a tourniquet in the Cantlie line instead of bipartition, associating liver tourniquet and portal vein occlusion for staged hepatectomy [ALTPS]), and obtained RLV hypertrophy in seven days.22
The aim of this paper is to present a clinical case in which we performed our technique, inserting the tourniquet in the umbilical fissure instead of the Cantlie line, to obtain hypertrophy of segments II–III in a patient with a large right lobe liver mass requiring right trisectionectomy.
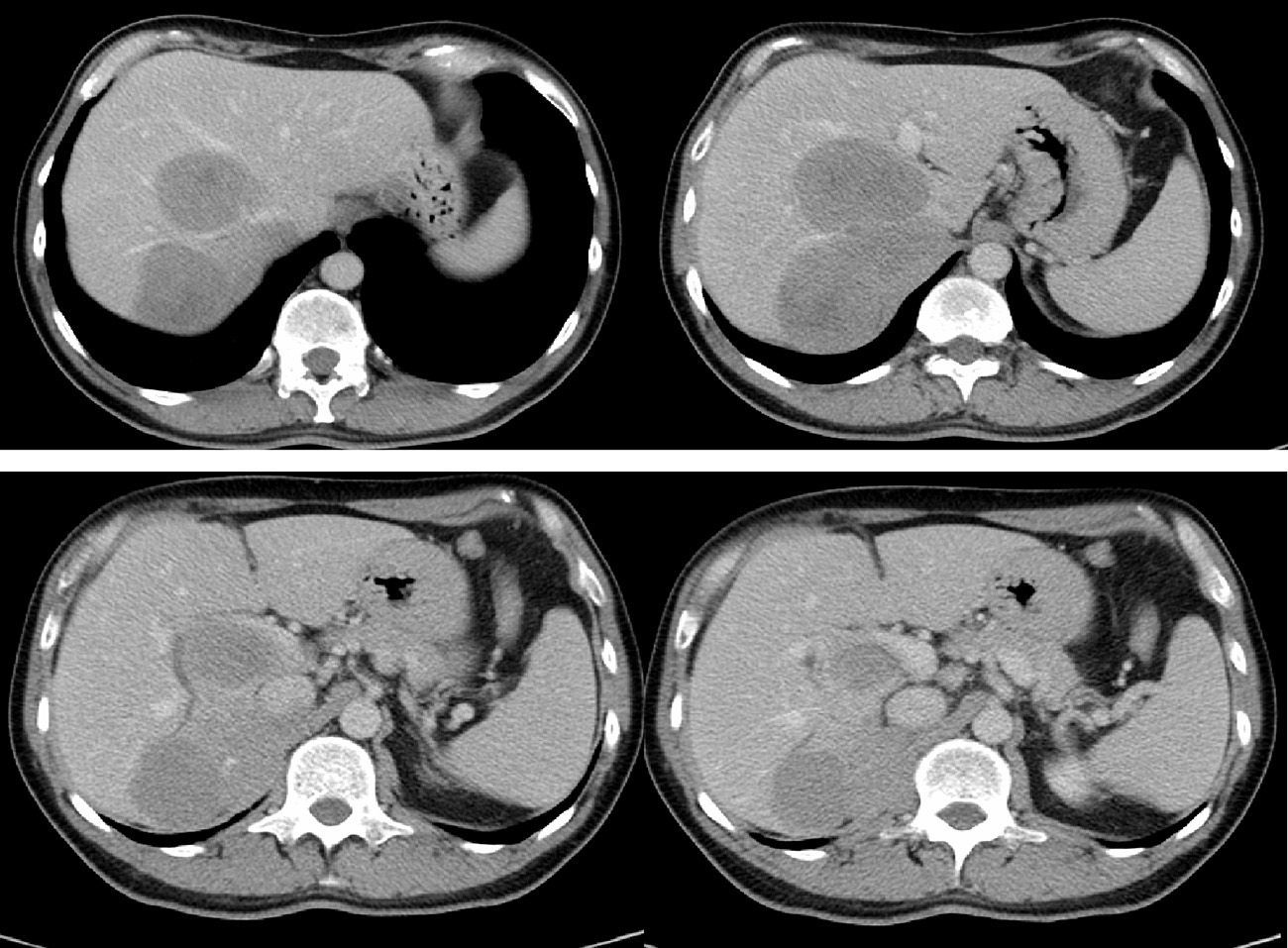
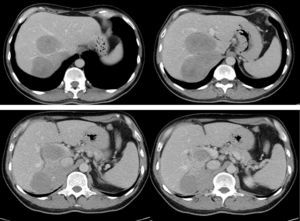
Clinical Case and Surgical TechniqueIn October 2002, a 51-year-old man underwent surgery for a 6cm right renal hypernephroma, with no adenopathy or vascular invasion. A right nephrectomy and lymphadenectomy were performed and the patient remained asymptomatic for nine years. In November 2011 an increase in transaminases was detected and an ultrasound scan was requested. This detected a large mass encompassing the right hepatic lobe, segment I and inferior vena cava (IVC). Bilirubin, transaminases, coagulation and tumour markers results were normal. Computed tomography (CT) detected a 20cm mass invading a large portion of the right lobe, right and median suprahepatic vein, segment I and the inferior vena cava around it in more than 70% of the circumference (invaded from 3cm above the left kidney bifurcation up to 2cm below the left suprahepatic vein) (Fig. 1). Hepatic volumetric analysis detected a RLV of 3870ml (20% total liver volume) with a liver volume/body weight quotient of 0.5. Extrahepatic disease was not detected by the PET. Our criteria23 led us to believe FLV was insufficient, and we therefore indicated a two-stage liver resection using the ALTPS technique.
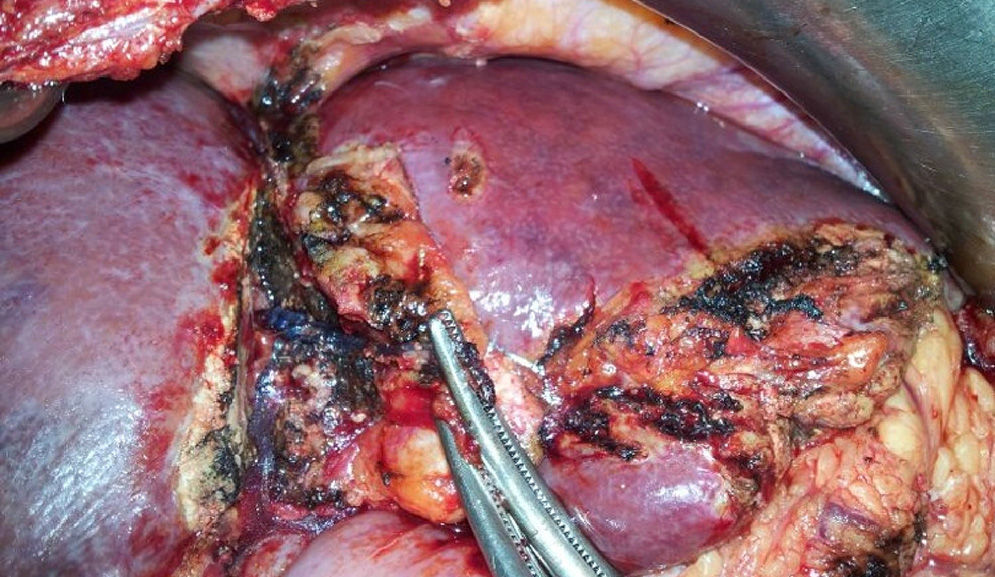
We examined the liver and the abdominal cavity through a subcostal bilateral incision, to rule out tumour dissemination. Cholecystectomy and transcystic drainage by cholangiography were performed. Dissection of the aforementioned right hepatic artery was performed using a vessel loop. The right portal vein was sectioned. The IVC was dissected above the left renal vein and below the left suprahepatic vein, using vessel-loop. Once it was confirmed that the tumour had not spread and that an R0 resection could be achieved at a second-stage, the Vicryl 3mm V152 Ethicon® tourniquet was inserted in the umbilical fissure. The tourniquet was passed between the middle and left suprahepatic veins, and continued around the base of the left lobe through the Rex recess to the left portal vein pedicle. Here it was passed in an extraglissonian manner to prevent pedicle occlusion when the tourniquet was closed. We then made a groove to the right side of the falciform ligament (umbilical fissure) which was knotted, occluding only the parenchyma and intrahepatic collaterals. Ultrasound showed the complete absence of circulation between segments II–III and segment IV. Operating time was 180min with minimal blood loss. During the postoperative period there was a 70% fall in Quick levels and increase in GPT to 240U/l. The patient was discharged on the fourth day following surgery with no complications. A CT scan with volumetrics was carried out on day seven.
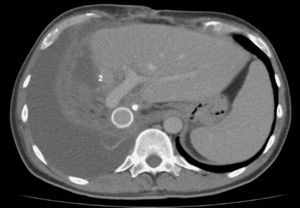
Postoperative Volumetrics and Secondary InterventionRLV rose to 953ml (31% of total hepatic volume), with an increase of 150% (573ml rise). The CT scan revealed the absence of collateral circulation through the tourniquet, the absence of tumour progression and tumour resectability (Fig. 2). Second stage surgery took place on the tenth day following the first stage, a VCI clamping test was performed, with perfect toleration and without the need for veno-venous by-pass. Ligation of the right bile duct, right hepatic artery and arterial branches of segment IV was made resulting in the complete separation and isolation of the left portal pedicle. Partition through the umbilical fissure (Fig. 3) was then performed, ligating the occluded portal branches of segment IV to the junction between the middle and left suprahepatic vein, the middle suprahepatic vein was ligated (the partition was performed in situ), completely separating segments II–III from the rest of the anatomic right lobe. The ICV was clamped above the left renal bifurcation and below the left suprahepatic vein, then sectioning the VCI above the left kidney and on the level of the right suprahepatic vein ostium. Finally, the ringed Gore-tex graft measuring 2cm in diameter and 8cm in length was inserted. Total VCI occlusion time was 70min, surgery time was 210min and blood loss was 600ml. A control cholangiography was carried out prior to closure, correctly displaying the remaining bile duct. There was a 57% postoperative drop in Quick levels, an increase of 2mg/dl in red blood cell count and of 267IU in GPT levels, requiring a 2IU blood transfusion. The patient was antiaggregated 48h after surgery and on the 5th day presented fever of 38°C; a perihepatic collection was revealed on CT scan. A radiological drain was placed to remove the collection, and the patient was discharged on the 12th day after surgery. The patient has since received periodic check-ups, the last with a CT-scan in July 2013 (Fig. 4). 20 months after the second surgical intervention there had been no disease recurrence.
The patient we present is the first case in the literature who associates complete retrohepatic IVG resection with right trisectionectomy, replacing it with a ringed Gore-tex 2cm graft and using the ALPPS or ALTPS hypertrophy technique. Using our technique, on the 7th postoperative day, we were able to achieve sufficient hypertrophy to perform the second surgical intervention, going from a baseline RLV of 20% to 31% (a 150% increase), which enabled the second-stage to be performed on the 10th postoperative day.
ALTPS is based on the same foundation as ALPPS: the intention of both is to achieve collateral circulation occlusion between both lobes24 to obtain faster hypertrophy. The advantage of our surgical technique is that we do not perform a split, we only insert a tourniquet in the bipartition line (in this case in the umbilical fissure); this alters the aggressiveness of both surgical interventions: “these are two TSLR interventions with the same physiopathological foundation”. This case demonstrates that with ALTPS the first intervention is much less aggressive: blood loss is lower, transfusion is unnecessary, the patient is discharged four days after surgery, and there is no need to use the Pringle manoeuvre, unlike the ALPPS in 22%16 and 33%,17 respectively. In a multicentre16 ALPPS study, blood loss during the first surgical intervention was 330ml, with a maximum of 7500ml, and 2 patients needed massive 15IU transfusions.
A frequent ALPPS complication is necrosis of segment IV due to ischaemia following ligation of the collateral branches during the first intervention,11,16–19 which results in infections, bile fistulas and delayed second surgery. This complication does not arise with our technique since we conserve part of the arterial vascularisation by not separating the Glissonian pedicle of segment IV.
After the second surgical intervention, our patient presented an infected collection which was treated with radiological drainage and antibiotics, with no signs of IHP. With ALPPS, morbidity varies between 53% and 64%,16–20 and some patients meet IHP criteria.16–20 Bile fistulas and infected collections are a frequent complication, with a risk of death in some series.16,18–20 The majority are associated with infected bile collections, sepsis, kidney failure, progressive cholestasis and multiple organ failure.
One drawback of traditional EPP and LPI is tumour progression,10,11 linked with prolonged regeneration time.7,11,25 In our case as the patient was reoperated on after ten days we found no evidence of tumour progression: an R0 resection was achieved and the patient was disease-free for 20 months after the second intervention.
In conclusion, our surgical technique is very different to the other described and obtains the same regeneration. It is less aggressive in the first intervention since we do not section the parenchyma and a tourniquet is positioned in the section line and in the right portal section. More extensive series are needed to assess the efficacy of ALPPS and ALTPS, and likewise the efficacy of these new techniques with regard to the classical portal occlusion techniques (EPP and LPI).
Conflict of InterestThe authors declare that there is no conflict of interest.
Please cite this article as: Robles Campos R, Parrilla Paricio P, López Conesa A, Brusadín R, López López V, Jimeno Griñó P, et al. Una nueva técnica quirúrgica para la hepatectomía derecha extendida: torniquete en la cisura umbilical y oclusión portal derecha (ALTPS). Caso clínico. Cir Esp. 2013;91:633–637.
Communication presented as a video at the European-African Hepato Pancreato Biliary Association Congress in Belgrade, from 28th May to 1st June 2013.