Aggressive angiomyxomas are mesenchymal tumors that are extremely rare in men. They most frequently affect adult women of reproductive age, and the female:male ratio is 7:1. Although they are usually benign tumors and distant metastasis is rare, there is a high rate of local recurrence. Described for the first time in 1986 by Steeper and Rosai, they originate in the soft tissue of the pelvic, perineal, vulvar or gluteal regions. In men, reported cases have been located in the groin, scrotum, and spermatic cord.1 Their name is related with the presence of spindle and stellate cells seen in histology studies, along with blood vessels of varying sizes in a myxoid matrix.2 There have been approximately 150 cases reported in premenopausal women and 43 cases in males; 70 of these were located in the pelvic and/or retroperitoneal regions.3,4 The clinical diagnosis is almost always difficult due to the lack of specific signs and symptoms.
In this present communication, we provide 4 new cases treated at Hospital de la Santa Creu i Sant Pau between 2011 and 2015: one male and 3 females, aged 40–65 (mean: 48 years) (Table 1). Their symptoms were nonspecific and related with compression and pelvic organ displacement (bladder, rectum, uterus, etc.), including 2 cases of dysuria, one case of rectal tenesmus and one case of pelvic pain. In the case of the male, physical exploration detected a right perineal mass that, on rectal examination, protruded laterally to the lumen of the rectum. In another case, the protrusion of the tumor appeared on the right labia majora of the patient's genitals. Radiologically, a retroperitoneal pelvic mass was seen with well-outlined edges, causing displacement of the pelvic organs and extension toward the ischiorectal fossa in the case of the male and toward the vulvar region in one woman. All patients were treated surgically with radical resection. The approach was abdominal in 3 patients and abdominoperineal in the case of the patient with vulvar extension, with mobilization to the plane of the levator ani and dissection of the mass from the adjacent planes to allow for specimen extraction. Care was taken to maintain adequate margins, and there was no tumor recurrence in any of the cases.
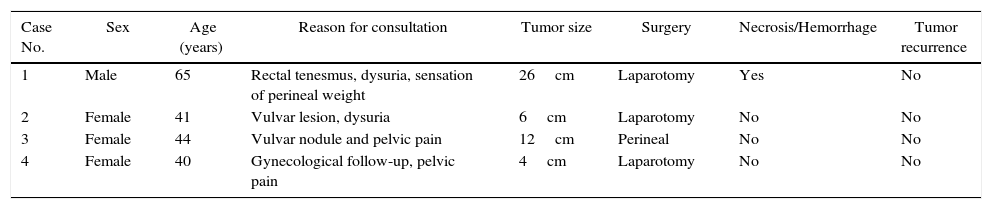
Anatomic and Clinical Data of Patients Treated for Aggressive Angiomyxoma.
| Case No. | Sex | Age (years) | Reason for consultation | Tumor size | Surgery | Necrosis/Hemorrhage | Tumor recurrence |
|---|---|---|---|---|---|---|---|
| 1 | Male | 65 | Rectal tenesmus, dysuria, sensation of perineal weight | 26cm | Laparotomy | Yes | No |
| 2 | Female | 41 | Vulvar lesion, dysuria | 6cm | Laparotomy | No | No |
| 3 | Female | 44 | Vulvar nodule and pelvic pain | 12cm | Perineal | No | No |
| 4 | Female | 40 | Gynecological follow-up, pelvic pain | 4cm | Laparotomy | No | No |
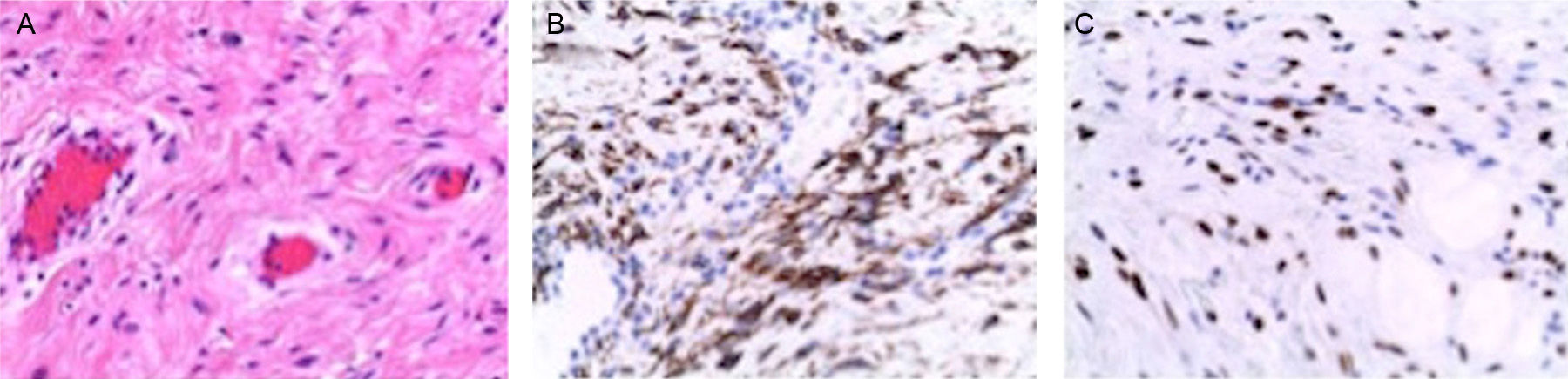
Macroscopically, the tumors were 4–26cm in size and had a soft, elastic consistency. The histopathologic aspect of all the lesions was fibromyxoid, with blood vessels of varying sizes and no areas of necrosis or hemorrhage, except for the male patient, where areas of superficial bleeding were observed (Fig. 1A). From an immunohistochemistry standpoint, there was positivity for desmin as well as estrogen receptors (Fig. 1B and C). During the current follow-up, none of the patients have presented tumor recurrence.
(A) Aggressive angiomyxoma (HE 200×): tumor cells with uniform oval nuclei without atypia, in an edematous stroma with collagen fibers and numerous dilated vessels; (B) Positive immunohistochemistry of the cells for desmin; (C) Positive immunohistochemistry of the cells for estrogen receptors.
CT images can be variable and often show a homogenous and hypodense mass compared to the muscle, and with slight intravenous contrast uptake. On MRI, their characteristics include an iso- or hypointense mass compared with the muscle in the enhanced images in T1 and hyperintense in T2 sequences, related with abundant myxoid matrix and high water content. They present notable enhancement in post-gadolinium sequences, with typical spiral-shaped uptake pattern and bands of different intensity inside caused by the fibrovascular stroma of the tumor.5,6
On histopathology, aggressive angiomyxomas are pseudopapillary in appearance. The surrounding myxoid tissue appears in places containing a proliferation of dense collagen. Generally, the tumor cells do not show cytonuclear atypia.7,8 A study by Rotmensch et al. demonstrated how aggressive angiomyxomas can be positive for estrogen and progesterone receptors and consequently be treated with hormone therapy.9
Surgical treatment is based on extensive surgery of the tumor while maintaining free margins, as this usually guarantees a cure with few functional consequences.5 Nonetheless, their infiltrating nature makes complete exeresis difficult, which occurred in our male patient. This is especially true when the location is pelvic and in contact with the rectum and/or bladder and reaches the ischiorectal space. In these cases, complete excision is more complex (either R1 or R2) and there is a greater risk of recurrence.
The success of radiotherapy and/or chemotherapy (especially given tumor recurrence) is low due to the existence of a large quantity of collagen in this type of tumors, associated with a low rate of mitotic activity and low cellularity.10
In conclusion, we can say that aggressive angiomyxomas are rare mesenchymal tumors that are benign in nature. They are more frequent in premenopausal women than in men and have a tendency toward local recurrence after their complete removal. There is no chemotherapy and/or radiotherapy that could improve the prognosis or could avoid or reduce the recurrence rate. It is therefore important to understand that the surgical exeresis of this tumor should be as complete and radical as possible.
Conflict of InterestThe authors have no conflict of interests to declare.
Please cite this article as: Artigas Raventós V, Rivero Cruces D, González López J, Rodríguez Blanco M, Boguña I. Angiomixoma agresivo. Un raro tumor mesenquimal pélvico. Cir Esp. 2016;94:359–361.