Trauma injuries are the main cause of death in the world. The aim of this study is to determine how trauma patients are treated in Spain at an organizational level.
Material and methodsA questionnaire was prepared consisting of 14 questions regarding aspects of the trauma care organization and trauma education. It was posted on the web site of the Spanish College of Surgeons and all members were encouraged to participate.
ResultsOne hundred and ninety questionnaires from 110 different hospitals were received. More than two-thirds (67.3%) of the centers had protocols for treating trauma patients, with 81% of them based on ATLS guidelines. Almost three-quarters (72.6%) of the doctors had completed the ATLS course, and 38.9% the DSTC course. There was a specific education program in trauma in 24.5% of the centers, and 35.5% had a Trauma Committee. There was a rehabilitation program in 24.5% of the centers.
ConclusionVery few of the participating centers would fulfill the requirements of the American College of Surgeons accreditation for trauma centers. Trauma care in Spain has improved a lot in the recent years, but there is still a lot to do to reach the level of that in the United States of America.
Las lesiones por trauma representan la principal causa de pérdida de años de vida en la población mundial. El objetivo es conocer qué grado de organización de la asistencia al paciente politraumatizado tenemos en España.
Material y métodosSe confeccionó una encuesta con 14 preguntas acerca de la organización de la asistencia al trauma y sobre la formación en aspectos de la atención al politraumatizado y se colgó en la web de la AEC, notificándolo por e-mail a todos los asociados.
ResultadosSe recibieron un total de 190 respuestas de 110 hospitales diferentes. El 67,3% de los centros encuestados tiene una protocolización de la asistencia al politraumatizado basada en el 81,1% en las directrices del ATLS. El 72,6% de los encuestados ha realizado el curso ATLS y el 38,9% el curso DSTC. De los centros encuestados, el 24,5% tiene un sistema formativo para su personal, el 32,7% tiene un registro o base de datos de enfermos politraumatizados, el 35,5% posee un Comité de Politraumatizados. El 24,5% de los centros facilita la rehabilitación y reinserción sociolaboral del paciente.
ConclusiónMuy pocos centros nacionales reunirían los requisitos completos para poder acreditarse como centro de trauma con los criterios americanos. La asistencia al trauma, si bien en los últimos años ha mostrado un creciente interés que se ha acompañado de un mayor desarrollo, todavía tiene un largo camino que recorrer hasta que lleguemos al nivel de implantación y desarrollo que poseen países como los Estados Unidos de Norteamérica.
Trauma injuries are one of the most important medical problems in our society because they are the main cause of loss of years of potential life in the population the world over.1,2 It is estimated that these injuries cause a loss of 500 years of annual productivity for every 100000 inhabitants3 and that they result in 5 million deaths per year.4,5 In Spain, trauma is the fifth most frequent cause of death according to the Spanish National Institute of Statistics, and it is the first cause of death in the population under the age of 40.6,7 In addition, the fact that trauma is the main cause of mortality in the youngest population age groups, which are the most productive, further compounds its costs. Even minor trauma is associated with a high rate of morbidity and mortality in the elderly.8 In some countries, the magnitude presented by the problem of trauma has led to the development of cost-effective systems to manage this type of patients, which help minimize the morbidity and mortality impact of this disease. These healthcare systems are called trauma care systems, and trauma centers are at their nucleus.
In Europe, the first trauma system was organized in Germany in 1972.9 Nowadays in most European cities, trauma care is organized and coordinated by general surgeons, acting as emergency surgeons or acute care surgeons.10 More recently created but much more advanced, homogenous and widespread is the trauma system used in the United States. In 1922, there started to be interest in developing a trauma system; the American College of Surgeons (ACS) created at that time the Committee on Treatment of Fractures, which is currently the Committee on Trauma (ACSCOT). This committee has provided the lead for conceptualizing and creating the trauma systems that were initiated in the US in 1966 with the publication of the National Academy of Sciences and the National Research Council: Accidental Death and Disability: The Neglected Disease of Modern Society.1 Afterwards, in 1976, hospital categorization was begun by ACSCOT and the first guidelines were published for trauma care.8 In 1980, the Advanced Trauma Life Support (ATLS) courses were standardized, and in 1987 the consultation/verification program was integrated into the trauma center formal designation process, defined in guidelines published by the ACS, and called Resources for the optimal care of the injured patient,11 which are periodically reviewed and modified. The impact of the implementation of trauma systems by the ACS has been analyzed in multiple publications and has been demonstrated to be a system that positively influences the survival of these patients, the quality of care provided, as well as costs.8,12–22
Although there is evidence that some European countries have organized trauma care, it is quite heterogeneous.9 In the case of Spain, the training of general and gastrointestinal surgeons does not specifically contemplate mandatory training in polytrauma. Nor is there a national trauma register in order to determine what is really happening in our country. As a consequence, we also do not know what level we are at in accordance with optimal care standards and to what extent we can improve quality of care while reducing medical expenses resulting from the care of these patients. Thus, the objective of the present study is to analyze the results of a survey on the organization of trauma care in our country.
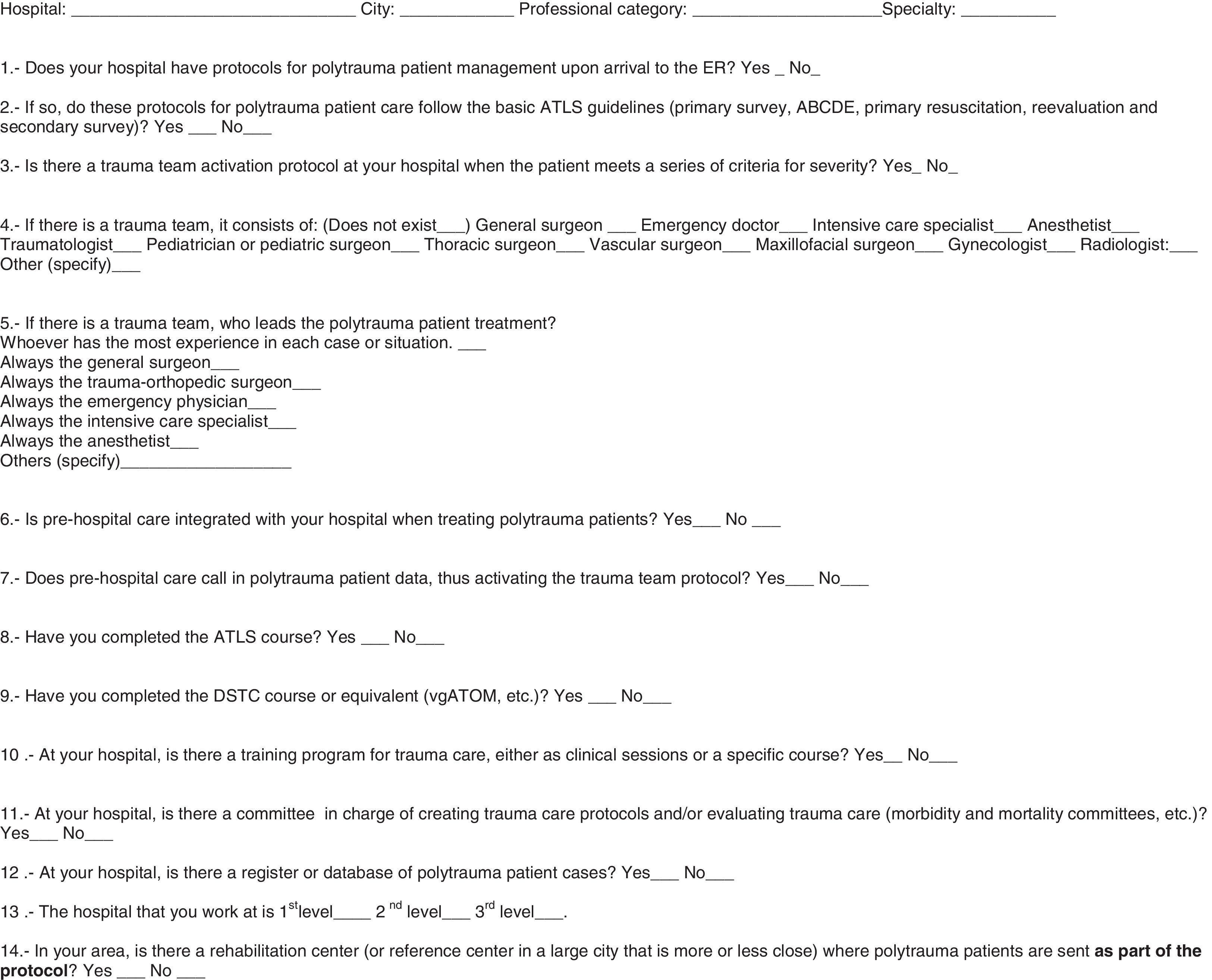
Material and MethodsA survey was created with 14 questions on the organization of trauma care and the training of doctors in specific aspects of polytrau ma patient treatment. The survey was posted in the news section of the Spanish Association of Surgeons website (http://www.aecirujanos.es/secciones/politraumatizados/encuesta_stae.php) for a period of nine months (July 2011 to March 2012). All members of the association were also invited to participate on 2 separate occasions during this period by e-mail. The survey questions referred to aspects about the organization of polytrauma patient treatment, all of which were close-ended (yes/no or similar) except for 2 (Fig. 1). The responses were collected in Access 97 and analyzed descriptively with the SPSS 9.0 statistical package.
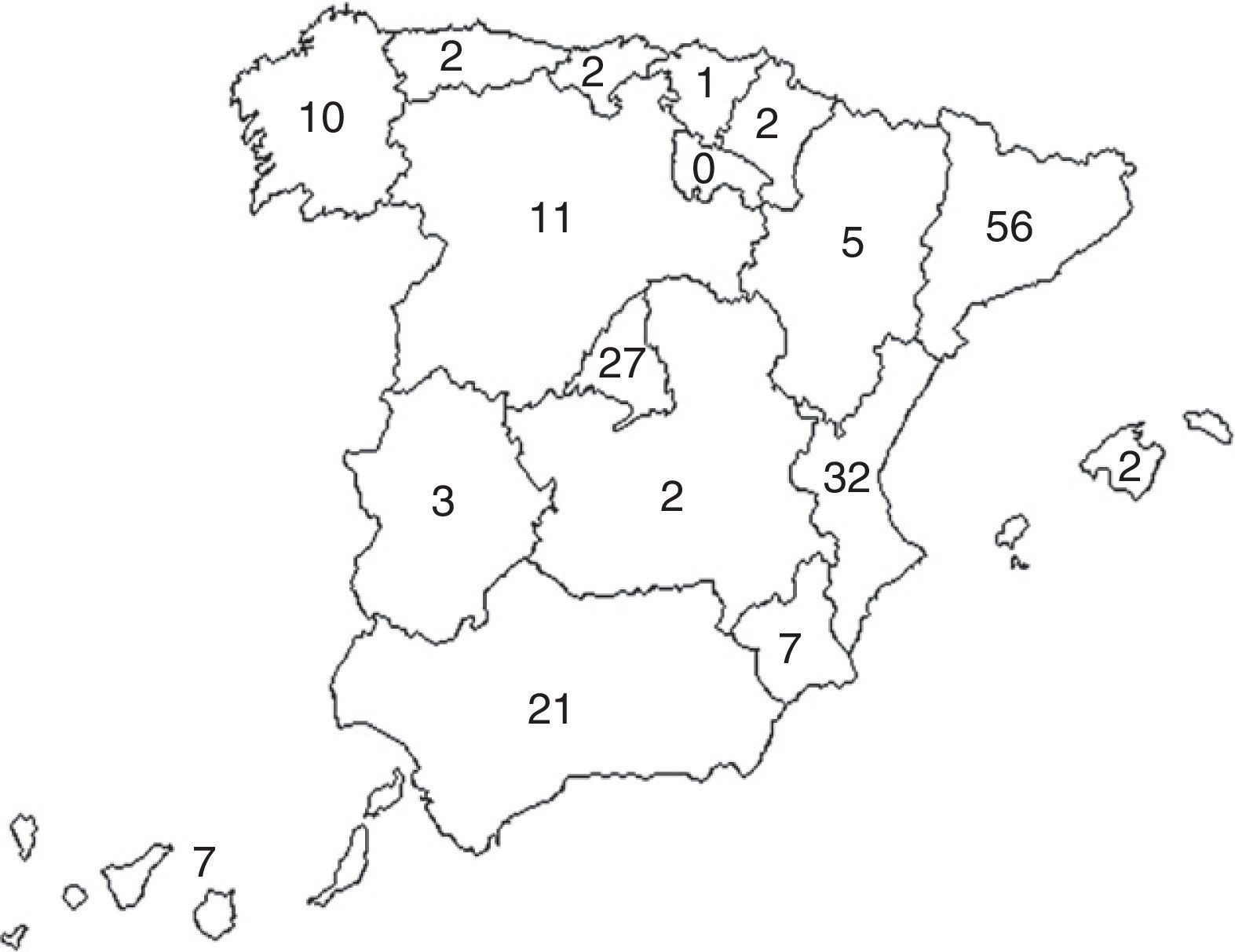
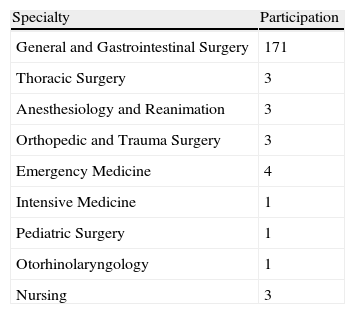
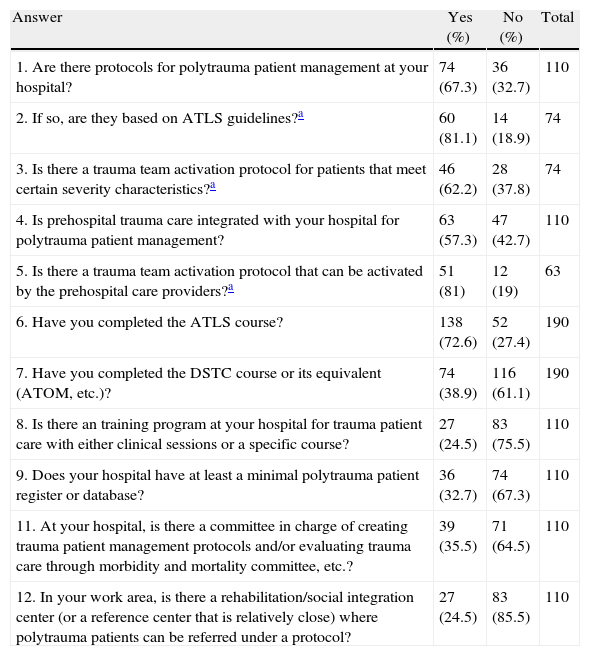
ResultsA total of 190 responses were received from 110 different hospitals. Fig. 2 shows the distribution of the participation by autonomous communities (Spanish provinces): participants from Catalonia turned in 56 surveys, from Valencia 32, Madrid 27 and Andalusia 21. The responses were sent by the following personnel at the different hospitals: 3 nurses, 14 directors of clinical services, 14 department heads, 21 residents and 138 attending physicians. Table 1 shows the specialties of these staff members. Table 2 compiles the results of the responses about polytrauma care organization and the training of the participating personnel. Of these, we should highlight that in 67.3% of the hospital centers (74) there were protocols in place for polytrauma care, 81.1% of which are based on the ATLS guidelines, and 53 centers (48%) have a multidisciplinary polytrauma team, with a corresponding protocol for activation in 46 of these. Furthermore, in the centers that have trauma teams, they are multidisciplinary and made up of doctors from at least 2 different specialties. The team leader is usually the anesthetist in 7 centers, the general surgeon in 5, the intensive care specialist in 15 and the ER physician in 7; in the remaining 19 centers, the team is usually led by the member of the trauma team that has the most experience in each situation. Thirty-nine centers (35%) have a Committee for Polytrauma Care that is in charge of generating the protocols and controlling the quality of care for these patients, as well as the correct application of the protocols. Twenty-seven centers (24%) have an intrinsic training system in polytrauma care for their personnel. 24.5% of the hospitals have a rehabilitation program or center for polytrauma patients. Out of the 190 people who responded to the survey, 138 had completed the ATLS course and 74 (38.9%) had completed the DSTC course.
Responses to the Questionnaire on the Organization of Trauma Systems in Spain.
| Answer | Yes (%) | No (%) | Total |
| 1. Are there protocols for polytrauma patient management at your hospital? | 74 (67.3) | 36 (32.7) | 110 |
| 2. If so, are they based on ATLS guidelines?a | 60 (81.1) | 14 (18.9) | 74 |
| 3. Is there a trauma team activation protocol for patients that meet certain severity characteristics?a | 46 (62.2) | 28 (37.8) | 74 |
| 4. Is prehospital trauma care integrated with your hospital for polytrauma patient management? | 63 (57.3) | 47 (42.7) | 110 |
| 5. Is there a trauma team activation protocol that can be activated by the prehospital care providers?a | 51 (81) | 12 (19) | 63 |
| 6. Have you completed the ATLS course? | 138 (72.6) | 52 (27.4) | 190 |
| 7. Have you completed the DSTC course or its equivalent (ATOM, etc.)? | 74 (38.9) | 116 (61.1) | 190 |
| 8. Is there an training program at your hospital for trauma patient care with either clinical sessions or a specific course? | 27 (24.5) | 83 (75.5) | 110 |
| 9. Does your hospital have at least a minimal polytrauma patient register or database? | 36 (32.7) | 74 (67.3) | 110 |
| 11. At your hospital, is there a committee in charge of creating trauma patient management protocols and/or evaluating trauma care through morbidity and mortality committee, etc.? | 39 (35.5) | 71 (64.5) | 110 |
| 12. In your work area, is there a rehabilitation/social integration center (or a reference center that is relatively close) where polytrauma patients can be referred under a protocol? | 27 (24.5) | 83 (85.5) | 110 |
Properly organized and protocolized trauma care has been demonstrated to be beneficial for patients. It reduces the time used in reanimation and reduces delays before surgical intervention if indicated, especially in penetrating trauma, which improves morbidity and mortality rates. Along these lines, Petrie et al. concluded that the severest patients (those with an ISS above 12) have clearly better results when treated in a trauma team activation system.23 In our survey, we have found that only 67.3% of the hospitals surveyed have a polytrauma treatment protocol, although 81.1% of these are based on ATLS guidelines. Only 62.2% of the centers with protocols declare having a trauma team activation plan,24,25 which would be the best case scenario according to the evidence.
On the other hand, 72.6% of those surveyed declare having completed the ATLS course, which is not a bad result when we considered that the course is not mandatory (not even as part of the residency program) for any other specialties represented. The ATLS method was initiated by James Styner and a training course was developed for the treatment of polytrauma patients, which was later adopted by the American College of Surgeons Committee on Trauma, and the ATLS course began in 1978.24,26 This method, which is now standardized and taught by the course in 50 countries, was established in Spain in the year 2000 through the Spanish Association of Surgeons27 with the aim to improve the knowledge and abilities of our professionals and, above all, to provide a common language.24 As has been mentioned, the ATLS course is not mandatory during training, although the effectiveness of the ATLS method has been demonstrated by several studies in different settings.28–31 For example, Ali et al.28 demonstrated that the ATLS program improved the results of polytrauma patients by reducing mortality from 68% to 34% after completing the course. With all this, it would seem that the ATLS course should be mandatory training for hospital personnel that are involved in one way or another with trauma patients. In many countries, it is required to have a valid ATLS certificate to be able to work in contact with trauma patients. Almost three-quarters of the survey participants declared having completed the course, which is not a bad result. We believe that, in time, this percentage will get closer to 100%, which would be ideal.
When faced with a polytrauma patient in a surgical setting, the concepts of damage control and operative management offered by the DSTC or ATOM courses are equally useful.32–34 The DSTC course (established by the IATSIC) is a more recent development in Spain and is specifically directed at surgeons, which is demonstrated by the lower percentage of staff that had completed the course (38.9%).
In trauma systems, the trauma center is the nucleus of the system. Depending on the functioning characteristics and the population area covered, this center should meet a series of characteristics. The ideal trauma center should include training for its personnel and ensure that the protocols are properly followed in morbidity and mortality sessions.21 It should also verify the level of knowledge and clinical effectiveness of the personnel treating these patients, and carry out a continuous audit of the care of these patients using a trauma register.11,24 Among the centers surveyed, 24.5% reported having a training system for their staff, 32.7% declared having a register or database of polytrauma patients and 35.5% declared having a committee in charge of evaluating the clinical efficiency of the management of these patients (Trauma Committee) or morbidity and mortality sessions of polytrauma patients. Likewise, one of the functions that a trauma system should perform is the rehabilitation of injured patients after having recovered from their acute problems.11,24,35 According to the result of the survey, in Spain this only happens in 24.5% of the centers surveyed. All these characteristics are essential conditions for a hospital to meet the requisites to be accredited as a trauma center in the US system of accreditation and verification, which, given its proven efficacy,1,8 should be considered the gold standard. Based on the results of the survey, very few Spanish centers would meet all the requisites to be accredited as a trauma center with the American criteria. It is true, however, that in some Spanish autonomous communities it is starting to become compulsory by law to meet minimum requirements, such as having an activation system for the trauma team and protocols for treating polytrauma patients.
In contrast, what is striking is the good general development that we have detected in the coordination of prehospital polytrauma care (57.3% stated having prehospital care integrated in the center, and 81% of the centers have a trauma care protocol and trauma team, with a trauma team activation protocol in 81% of the cases). Nonetheless, we should not be tempted to consider that an excess of polytrauma patient assistance is synonymous with improved quality.36 On many occasions, there continues to be a lack of early communication between the prehospital assistance provider and the receiving hospital. As many centers do not have a trauma register, it is not possible to get any feedback about the quality of care in either of the two trauma care settings.
The present paper has a very obvious bias: the participants who answered the survey either have a personal interest in trauma care, or at the hospital where they work relevance is given to the care of this type of patients. Meanwhile, those who did not answer the survey may possibly lack this interest. This bias would over-interpret the reality of trauma assistance. In spite of this, we believe that although the interest in trauma care may have grown in our country in recent years, it still has a long way to go to reach the level of other countries such as the United States, Australia, Israel, Germany or Austria.10 In this function of improving and implementing trauma care, the Polytrauma Section of the Spanish Association of Surgeons plays a very important role, as it has demonstrated up to the present time. But, it is also necessary to accompany this effort with large doses of enthusiasm and motivation from the professionals who, at each particular hospital, would promote this development. What is also needed is greater involvement of the local, regional and national government, providing greater specific funding and a legal framework that would promote more and better development of polytrauma patient treatment, concentrating cases of severe trauma in specially designed and accredited hospitals.37 The number of these centers would logically be proportional to the number of inhabitants in each province or public healthcare region, following well-known recommendations and studies. Necessary and essential conditions would be the initiation of a mandatory trauma register in each of these hospitals, the organization of integral care for these patients and the creation of the figure of hospital trauma coordinator, who would unite these organizational efforts.
Conflict of InterestThe authors have no conflict of interest to declare.
Please cite this article as: Costa Navarro D, Jiménez Fuertes M, Ceballos Esparragón J, Montón Condón S, Jover Navalón JM, Turégano Fuentes F, et al. Análisis de los resultados de una encuesta sobre los sistemas de trauma en España: la enfermedad abandonada de la sociedad moderna. Cir Esp. 2013;91:432–437.