To analyze the effectiveness and quality of ambulatory laparoscopic cholecystectomy (CLCMA) versus management of laparoscopic cholecystectomy with conventional hospital stay (CLEST).
Material and methodsA retrospective study was conducted on all patients ASA I-II, who had a laparoscopic cholecystectomy (LC) over a period of 6 years. The patients were divided into 2 groups: group CLCMA (n=141 patients) and group CLEST (n=286 patients).
The effectiveness was analyzed by evaluating morbidity, further surgery, re-admission and hospital stay. The quality analysis was performed using CLCMA group satisfaction surveys and subsequent assessment by indicators of satisfaction.
ResultsThere was no significant differences between groups (CLEST vs CLCMA) in morbidity (5.24 vs 4.26), further surgery (2.45 vs 1.42) or re-admissions (1.40 vs 3.55). There was no postoperative mortality. In the CLCMA group 82% of patients were discharged on the same day of surgery, with a mean stay of 1.16 days, while in the CLEST group the mean hospital stay was 2.94 days (P=.003). The overall satisfaction rate was 82%, and the level of satisfaction of care received was 81%, both above the previously set standard.
ConclusionsCLCMA is just as effective and safe as hospital based CLEST, with a good level of perceived quality.
Analizar la efectividad y calidad de la colecistectomía laparoscópica en régimen ambulatorio (CLCMA) frente al manejo convencional de la colecistectomía laparoscópica con estancia (CLEST).
Material y métodosEstudio retrospectivo donde se analizan todos los pacientes ASA I-II, durante 6 años, intervenidos mediante colecistectomía laparoscópica (CL). Se establecen 2 cohortes de pacientes: grupo CLCMA (n=141 pacientes) y grupo CLEST (n=286 pacientes).
La efectividad se analizó evaluando morbimortalidad, reintervenciones, reingresos y estancia. El análisis de calidad del grupo CLCMA se realizó mediante encuestas de satisfacción y posterior valoración mediante indicadores de satisfacción.
ResultadosNo existieron diferencias estadísticamente significativas entre ambos grupos (CLEST vs CLCMA) en morbilidad (5,24 vs 4,26), reintervenciones (2,45 vs 1,42) ni en reingresos (1,40 vs 3,55). No hubo mortalidad postoperatoria. El 82% de los pacientes del grupo CLCMA fueron alta el mismo día de la intervención, siendo la estancia media de este grupo 1,16 días, mientras que en el grupo CLEST fue de 2,94 días (p=0,003). El índice de satisfacción global fue de un 82% y el indicador de satisfacción de la asistencia recibida fue del 81%, ambos por encima del estándar previamente fijado.
ConclusionesLa CLCMA es tan efectiva y segura como la CLEST programada, con un buen nivel de calidad percibida.
Laparoscopic cholecystectomy (LC) in the major outpatient surgery (MOS) setting does not have a uniform distribution in the hospitals throughout our public healthcare system1 due to its connotations.
In 2010, we performed a study that analyzed the reliability of laparoscopic cholecystectomy as major outpatient surgery (LCMOS) in our center. In doing so, we analyzed an initial series of 110 cases, obtaining results that were comparable with national LC reports in Spain.2 Nonetheless, we feel that more studies are necessary to compare the effectiveness of LCMOS versus LC with hospitalization, both in terms of morbidity and mortality. Once its effectiveness is demonstrated, it will then only be necessary to assess the quality perceived by patients. With equal effectiveness, it is assumed that there will be greater efficiency when the patients are operated on in LCMOS.
We carried out a study whose main objective was to compare the effectiveness of LCMOS with early hospital discharge (6h) compared with LC with hospital stay (LCHS) within our clinical unit. The effectiveness was analyzed in terms of morbidity and mortality, rate of reinterventions and re-admittances. The secondary objectives were to analyze the reasons for hospitalization in the MOS patients, assess the quality perceived by the patients who completed the MOS regime and analyze the reasons that impede a greater use of ambulatory treatment.
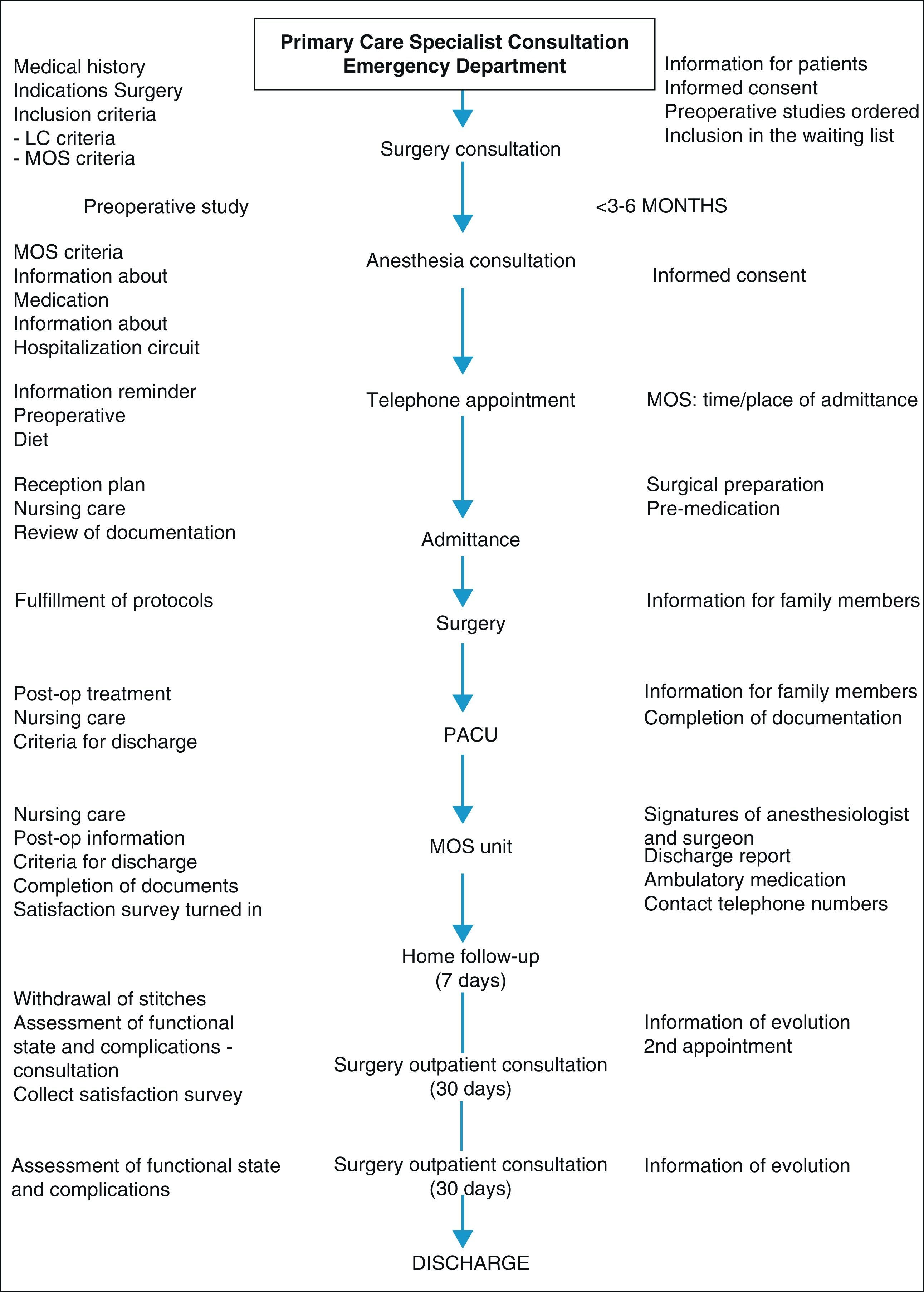
Patients and MethodsIn January 2005, after the first 10 LCMOS, it was decided to include in this regime all those patients with uncomplicated symptomatic cholelithiasis who met the established criteria: (a) local criteria: no admittances due to acute cholecystitis or acute pancreatitis in the previous 3 months, absence of lithiasis in the main bile duct and normal liver function tests; (b) general criteria: absence of prior supramesocolic abdominal surgery, no oral anticoagulants or antiplatelet agents and patients with American Society of Anesthesiologists (ASA) status grades I and II; (c) social criteria: distance to the hospital, family support, possibility of telephone contact and acceptance of this by the patient. If the social criteria for MOS were not met, the patients were put on the surgical waiting list for LCHS (Fig. 1).
A retrospective study was performed of the patients who had undergone LC due to symptomatic uncomplicated cholelithiasis in the MOS regime (LCMOS, n=141 patients) over a period of 6 years (January 2005–December 2010). At the same time, another series of patients was compiled from the same period who met the same MOS criteria and had undergone surgery with hospital stay because they did not meet the social criteria (LCHS, n=286 patients).
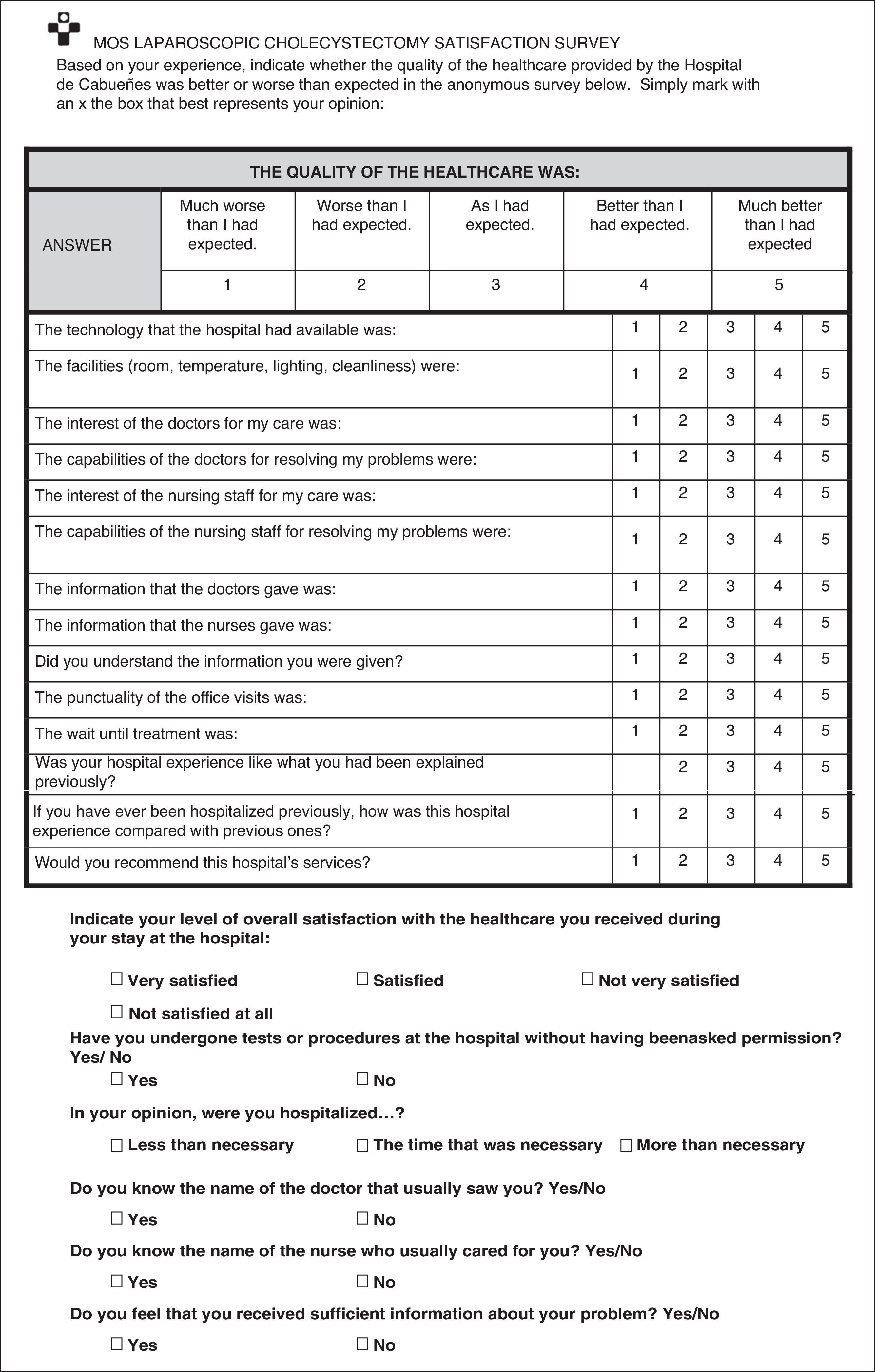
For the data collection, a database was used that had been designed to create a registry of the patients who had been operated on due to cholelithiasis without complications using LC. The database included aspects referring to the symptoms that were the cause for consultation, previous morbidity, ASA grade, previous abdominal surgery (supramesocolic or not), treatment regimen (hospitalization vs MOS), intraoperative complications, drainage, conversion to laparotomy and causes, postoperative complications (medical and surgical), reintervention and causes, as well as number of hospitalizations and re-admittances. Furthermore, for those patients who underwent MOS surgery, the reason for hospitalization on the surgical floor was included along with aspects referring to the satisfaction survey that they were given upon discharge, which was returned at the first postoperative office visit (Fig. 2).
LC was performed in 100% of the cases with 4 entry ports by a total of 4 surgeons with experience in biliary surgery (more than 50 procedures), 2 of them with special interest in MOS.
Both groups had the same medical-surgical resources available, both intra- and post-operatively. The criteria for discharge were: controlled vital signs, oral tolerance, mild post-surgical pain, adequate mobility/walking and absence of complications. In the case of the patients operated on in the MOS regime, the patients were contacted 6h after discharge. An office visit was likewise scheduled in both groups for 7–10 days after the intervention, at which time the satisfaction survey was collected.
For the statistical analysis, the SPSS version 14.0 program was used and a 5% level of significance was set. In the univariate analysis, the quantitative variables were expressed as means and standard deviation, and the qualitative variables were expressed as absolute values and percentages. In both types of variables, 95% confidence intervals were calculated. In the bivariate analysis, the comparison between qualitative variables was calculated with the χ2 and the Student's t tests for the comparison of means in the quantitative variables.
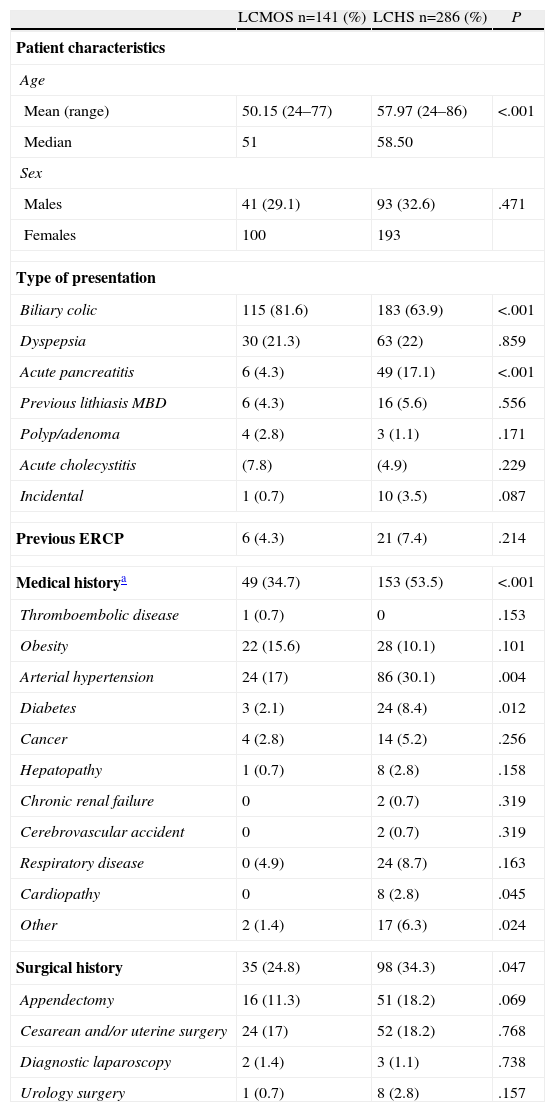
ResultsTable 1 shows the pre-surgical characteristics of the patients in both groups. Despite the patients being classified as ASA I–II, there were statistically significant differences, so that the patients of the LCHS group presented an older age and greater comorbidities. The presence of surgical history was higher in the LCHS group, with slightly significant differences.
Pre-surgical Characteristics of the Patients.
| LCMOS n=141 (%) | LCHS n=286 (%) | P | |
| Patient characteristics | |||
| Age | |||
| Mean (range) | 50.15 (24–77) | 57.97 (24–86) | <.001 |
| Median | 51 | 58.50 | |
| Sex | |||
| Males | 41 (29.1) | 93 (32.6) | .471 |
| Females | 100 | 193 | |
| Type of presentation | |||
| Biliary colic | 115 (81.6) | 183 (63.9) | <.001 |
| Dyspepsia | 30 (21.3) | 63 (22) | .859 |
| Acute pancreatitis | 6 (4.3) | 49 (17.1) | <.001 |
| Previous lithiasis MBD | 6 (4.3) | 16 (5.6) | .556 |
| Polyp/adenoma | 4 (2.8) | 3 (1.1) | .171 |
| Acute cholecystitis | (7.8) | (4.9) | .229 |
| Incidental | 1 (0.7) | 10 (3.5) | .087 |
| Previous ERCP | 6 (4.3) | 21 (7.4) | .214 |
| Medical historya | 49 (34.7) | 153 (53.5) | <.001 |
| Thromboembolic disease | 1 (0.7) | 0 | .153 |
| Obesity | 22 (15.6) | 28 (10.1) | .101 |
| Arterial hypertension | 24 (17) | 86 (30.1) | .004 |
| Diabetes | 3 (2.1) | 24 (8.4) | .012 |
| Cancer | 4 (2.8) | 14 (5.2) | .256 |
| Hepatopathy | 1 (0.7) | 8 (2.8) | .158 |
| Chronic renal failure | 0 | 2 (0.7) | .319 |
| Cerebrovascular accident | 0 | 2 (0.7) | .319 |
| Respiratory disease | 0 (4.9) | 24 (8.7) | .163 |
| Cardiopathy | 0 | 8 (2.8) | .045 |
| Other | 2 (1.4) | 17 (6.3) | .024 |
| Surgical history | 35 (24.8) | 98 (34.3) | .047 |
| Appendectomy | 16 (11.3) | 51 (18.2) | .069 |
| Cesarean and/or uterine surgery | 24 (17) | 52 (18.2) | .768 |
| Diagnostic laparoscopy | 2 (1.4) | 3 (1.1) | .738 |
| Urology surgery | 1 (0.7) | 8 (2.8) | .157 |
ERCP: endoscopic retrograde cholangiopancreatography; MBD: main bile duct.
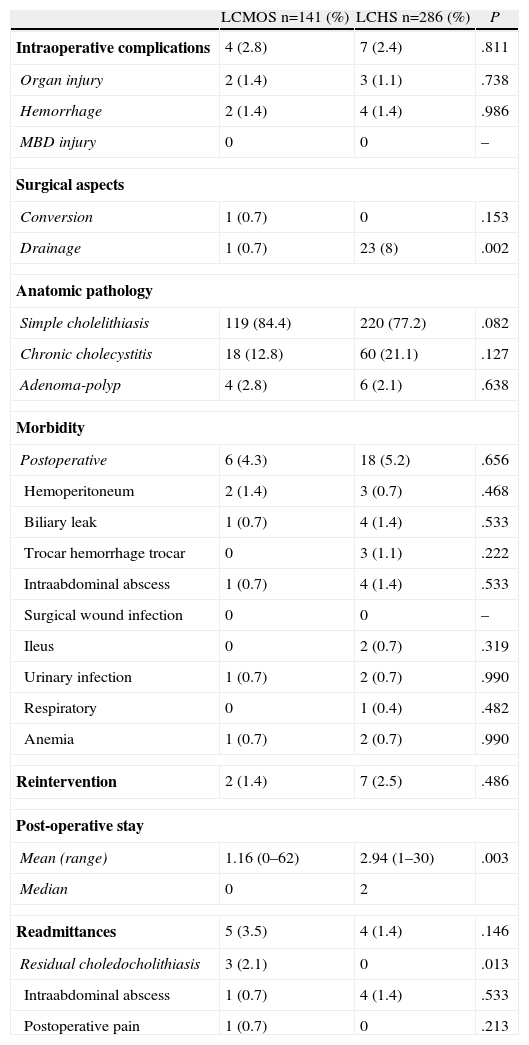
Table 2 demonstrates the post-surgical characteristics in both patient groups. Significant differences were only observed in the use of drains, which was significantly higher in the LCHS group.
Post-surgical Patient Characteristics.
| LCMOS n=141 (%) | LCHS n=286 (%) | P | |
| Intraoperative complications | 4 (2.8) | 7 (2.4) | .811 |
| Organ injury | 2 (1.4) | 3 (1.1) | .738 |
| Hemorrhage | 2 (1.4) | 4 (1.4) | .986 |
| MBD injury | 0 | 0 | – |
| Surgical aspects | |||
| Conversion | 1 (0.7) | 0 | .153 |
| Drainage | 1 (0.7) | 23 (8) | .002 |
| Anatomic pathology | |||
| Simple cholelithiasis | 119 (84.4) | 220 (77.2) | .082 |
| Chronic cholecystitis | 18 (12.8) | 60 (21.1) | .127 |
| Adenoma-polyp | 4 (2.8) | 6 (2.1) | .638 |
| Morbidity | |||
| Postoperative | 6 (4.3) | 18 (5.2) | .656 |
| Hemoperitoneum | 2 (1.4) | 3 (0.7) | .468 |
| Biliary leak | 1 (0.7) | 4 (1.4) | .533 |
| Trocar hemorrhage trocar | 0 | 3 (1.1) | .222 |
| Intraabdominal abscess | 1 (0.7) | 4 (1.4) | .533 |
| Surgical wound infection | 0 | 0 | – |
| Ileus | 0 | 2 (0.7) | .319 |
| Urinary infection | 1 (0.7) | 2 (0.7) | .990 |
| Respiratory | 0 | 1 (0.4) | .482 |
| Anemia | 1 (0.7) | 2 (0.7) | .990 |
| Reintervention | 2 (1.4) | 7 (2.5) | .486 |
| Post-operative stay | |||
| Mean (range) | 1.16 (0–62) | 2.94 (1–30) | .003 |
| Median | 0 | 2 | |
| Readmittances | 5 (3.5) | 4 (1.4) | .146 |
| Residual choledocholithiasis | 3 (2.1) | 0 | .013 |
| Intraabdominal abscess | 1 (0.7) | 4 (1.4) | .533 |
| Postoperative pain | 1 (0.7) | 0 | .213 |
MBD: main bile duct.
As for the rate of re-interventions, 2 patients (1.4%) in the LCMOS group were re-operated due to hemoperitoneum, while in the LCHS group 7 patients (2.5%) were re-operated on: 4 patients due to biliary peritonitis (biliary leak) and 3 patients due to hemoperitoneum. These differences were not statistically significant.
There was no post-operative mortality.
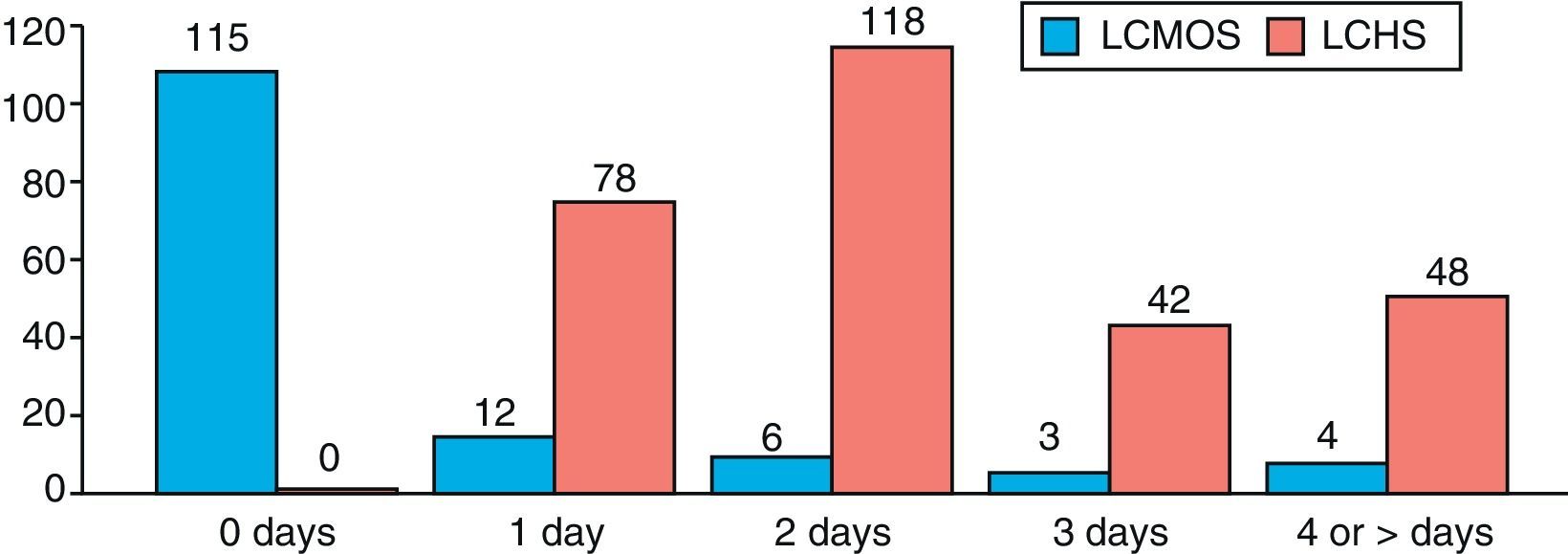
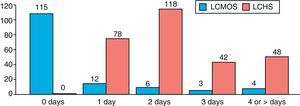
Regarding post-operative hospital stay, the patients of the LCMOS group presented a mean stay of 1.16 days, while in the LCHS group it was 2.94 days, with statistically significant differences (P=0.003) (Fig. 3). Within the patient group with LCMOS, a total of 115 patients (82%) were discharged 6h after the surgical intervention, thus complying with the MOS regime. The reasons for hospitalization of the 26 remaining patients were: poorly controlled pain (2 patients), high surgical difficulty (4 patients), presence of nausea/vomiting (5 patients), dizziness (2 patients), hemodynamic instability (3 patients), social reasons (6 patients), urinary retention (3 patients) and conversion to laparotomy (one patient).
There were no significant differences between the two groups with regard to rate of re-admittances. Within the LCMOS patient group, 5 patients (3.5%) required re-admittance: 3 patients for residual choledocholithiasis resolved with endoscopic retrograde cholangiopancreatography (ERCP), one patient for sustained pain with no evidence of disease and one patient for intraabdominal abscess treated with percutaneous drainage. Among the patients of the LCHS group, there was a total of 4 readmittances due to intraabdominal abscesses, which were resolved conservatively (3 using percutaneous drainage and one with antibiotic treatment).
Given that the group of LCHS patients presented a higher rate of previous comorbidity, we assessed whether this was related to a greater probability of presenting postoperative complications, higher rate of reinterventions or a higher rate of readmittances. There were no statistically significant differences observed (P=0.169; P=0.616 and P=0.862, respectively).
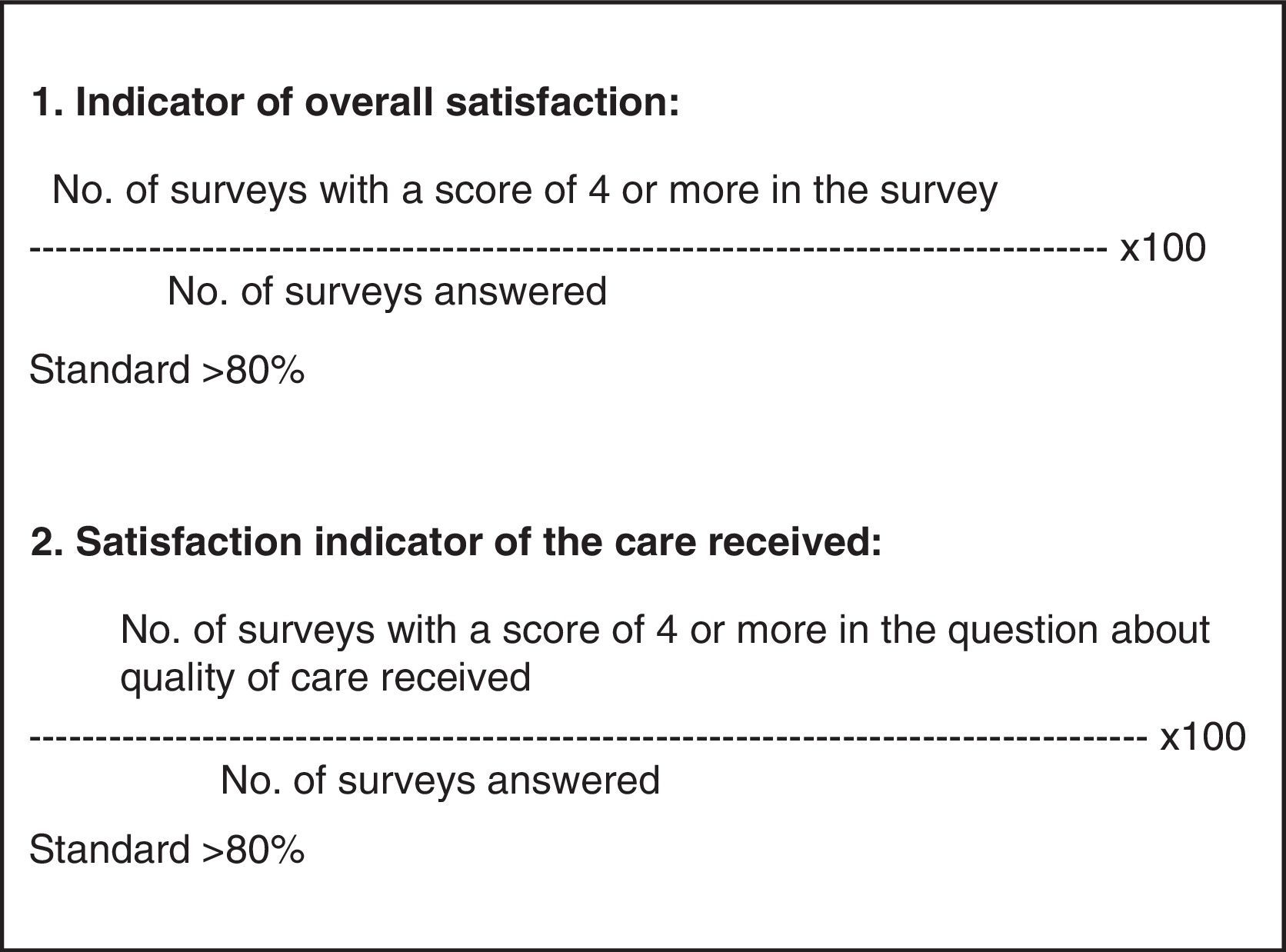
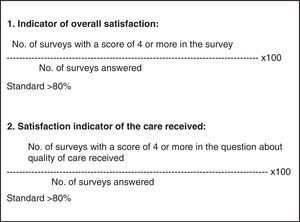
After excluding the patients who required hospitalization, a total of 80 patients (70%) answered and returned the satisfaction survey at the first scheduled office visit. For the assessment of this survey, we considered the indicators for overall satisfaction (82%) and perceived overall care satisfaction (81%). Both indicators were situated above the previously set standard (Fig. 4).
DiscussionLC is considered the gold standard technique in the treatment of symptomatic cholelithiasis.3–7 Nonetheless, LCMOS does not have a uniform presence in the hospitals of our public healthcare system since surgeons assume an “unnecessary risk” in the patients’ medical treatment.1
Several studies, however, have demonstrated that LCMOS is reliable and effective, as seen in the degree of satisfaction and quality perceived by the patients.5,6,8–14 It has been confirmed that the recovery of patients treated in the MOS regime, as well as their level of anxiety and quality of life, are similar to hospitalized patients.15 There are even studies that show evidence of better recovery among patients operated on in the LCMOS regime, as they present a lower degree of tiredness, which is attributable to a night of rest in their own homes.16
Studies are therefore necessary to compare the effectiveness of LCMOS versus LCHS, both in terms of morbidity and mortality. These studies would be more reliable if both variations were performed within the same hospital and the patients were all selected with the same criteria.
This present study attempts to analyze this situation, with special interest given to demonstrating that, initially, LCMOS is just as safe as LCHS.
In our study, our attention is called to the fact that out of the 427 patients who met MOS criteria, close to 50% did not meet the social criteria and, within this group, in most instances this was related with patient refusal. This is probably because patients perceive uncertainty shown by the surgeon when discussing the MOS program indication. Second, it is the more senior patients who usually refuse the ambulatory surgery regime and, logically, older age is associated with more comorbidity. This may be a reason why both study groups are not entirely homogeneous; these differences, however, were not associated with a higher rate of complications.
Furthermore, we observed that 30% of the patients in the MOS program migrated to LCHS as part of the waiting list reduction programs. This is due to the high prevalence of this disease and the limited possibility of performing this surgery on an outpatient basis (potentially only once a week). All these factors must be taken into account when promoting the outpatient treatment program.
We observed that our results are comparable to those reported in the literature: morbidity rate of 6%, 1.2%–5% conversions, 1% reoperations and 2%–4% readmissions.5,7–9 There were no significant differences between the two groups when comparing postoperative morbidity, reintervention or readmission rates.
Coinciding with the data reported in the literature, postoperative morbidity mainly consisted of the presence of hemoperitoneum due to bleeding at the surgical site, bile leak or intraabdominal abscess. The presence of bleeding at the surgical site was detected in the early postoperative period because of hemodynamic instability, while the 4 reoperations for biliary leak were performed more than 24h afterwards. It has been observed that major complications are usually diagnosed either during the surgery itself or more than 48h afterwards; they would therefore also go unnoticed in the LCHS regime.1,8,17
During the surgical procedure, the surgeon detects the higher probability of complications and implements the necessary mechanisms to be prepared for this possible outcome. Such was the case of the 4 patients from the LCMOS group who were admitted for fear of postoperative LCMOS complications, or misuse of drains in the LCHS series where, since the patient is hospitalized, the surgeon tends to make more use of them. Therefore, given the results obtained, we are able to say that the LCMOS is as safe as LCHS.
In our study, only 30% of the LCHS group patients were discharged the following day, which could be related to the surgeon's passivity. The percentage of hospitalizations in the LCMOS group was 18%, similar to reports (8%–40%) in recent studies.1,5,6,8,12–14 We infer, therefore, that performing LCMOS gives the surgeon a greater degree of commitment to the hospital institution which, together with patient information, are the keys to success of this surgical modality.
Among the reasons for hospitalization of the 26 patients in the LCMOS group, only 6 patients were admitted due to social causes. Reasons for admission such as nausea/vomiting, urinary retention or poorly controlled pain could be improved with the administration of recently approved drugs and improvements in anesthesia techniques.14,18 However, nearly 50% of the patients who were admitted to the surgical ward from the MOS unit were discharged the following day.
In the present study, the LCMOS group patients had a mean stay of 1.16 days, versus the mean postoperative stay of 2.94 days in the LCHS group. It is further noted that, in our experience, if the patient is not discharged within the first 6h, he/she is admitted to the hospital ward.
Several studies have demonstrated that both the degree of satisfaction and quality perceived by patients treated in LCMOS programs have been good.6,8–11 In the present series, 81% of the patients were satisfied with the care received, while 82% expressed overall satisfaction.
Proper patient selection, personal interview and surgeon-patient interaction are necessary to ensure the success of care management. Improvements in the legal framework would make surgeons feel protected when providing this type of treatment.
Having established the fact that LCMOS is not inferior to LCHS in terms of effectiveness, safety or quality, what remains is to assess whether the commitment acquired from professionals and patients would lead to savings in actual medical expenses. For this purpose, a study should be undertaken to analyze the difference in cost between the outpatient and hospitalization variations.
ConclusionsLCMOS in ASA I-II patients is as safe and effective as scheduled LCHS, with a good level of quality perceived by patients.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Lezana Pérez MÁ, Carreño Villarreal G, Lora Cumplido P, Álvarez Obregón R. Colecistectomía laparoscópica ambulatoria versus con ingreso: estudio de efectividad y calidad. Cir Esp. 2013;91:424–431.