There is controversy in the literature about the choice of expectant medical treatment vs surgical treatment of hiatal hernias, depending on the presence or absence of symptoms. This study presents the results obtained by our group, considering disease duration and postoperative results.
Patients and methodA total of 121 patients were included and divided by age, disease duration, type of hiatal hernia and postoperative outcome.
ResultsIn 32% of the patients younger than 70 years, symptom duration was longer than 11 years and 68% of those aged more than 71 years had long-term symptoms (P<.05). Type iv hernias (complex) and those with diameters measuring more than 16cm were observed in the group with longer symptom duration. Complications were more frequent in the older age group, in those with longer symptom duration and in those with type IV complex hernias. There was no postoperative mortality and only one patient (0.8%) with a type III hernia and severe oesophagitis required reoperation.
ConclusionWe recommend that patients with hiatal hernia undergo surgery at diagnosis to avoid complications and risks. Older patients should not be excluded from surgical indication but should undergo a complete multidisciplinary evaluation to avoid complications and postoperative mortality.
En la literatura se evidencia la controversia existente entre el tratamiento médico expectante versus el tratamiento quirúrgico sistemático de las hernias hiatales y respecto a cuál es la opción más adecuada dependiendo de la presencia o no de síntomas. En este estudio se presentan los resultados obtenidos por nuestro grupo, considerando el tiempo de evolución de la enfermedad y los resultados postoperatorios.
Pacientes y métodoSe incluye a 121 pacientes dignosticados de herni de hiato divididos por edad, tiempo de evolución y tipo de la hernia hiatal y se evalúan los resultados postoperatorios.
ResultadosEl 32% de los pacientes menores de 70 años tenían más de 11 años de evolución de los síntomas; en cambio, en el grupo de pacientes mayores de 71 años el 68% tenían síntomas de ambiar larga data por mayor tiempo de evolución, (p < 0,05). Las hernias tipo IV (complejas) y de tamaño mayor de 16cm de diámetro se observaron en el grupo con mayor tiempo de evolución de los síntomas. Las complicaciones se observaron más frecuentemente en el grupo de mayor edad, de mayor tiempo de evolución de los síntomas o en pacientes con hernias tipo IV complejas. No hubo mortalidad postoperatoria y solo un paciente (0,8%) con hernia tipo III y esofagitis severa debió ser reoperado.
ConclusiónPensamos que los pacientes con hernia hiatal deben operarse en el momento de su diagnóstico para evitar riesgos de complicaciones y los pacientes añosos no se deben excluir de la indicación quirúrgica pero deben ser evaluados en forma completa multidisciplinaria para evitar complicaciones y mortalidad postoperatoria.
Articles found in the literature show the controversy between wait-and-see medical treatment vs surgical treatment of hiatal hernias, and which option is best depending on the presence or absence of symptoms. Some authors favor conservative medical management, claiming that most patients with hiatal hernias are asymptomatic or have minor symptoms. In contrast, others prefer to indicate surgery at the time when hiatal hernia is diagnosed, regardless of symptoms, to prevent any possible progression or complications.1–6 Currently, there is considerable literature about the successful results obtained by laparoscopic surgery in the short- and long-term, even in elderly patients.7–13 This study presents the results of our group, including surgical indications, preoperative symptoms, duration of the disease and postoperative results of the surgical treatment of hiatal hernia.
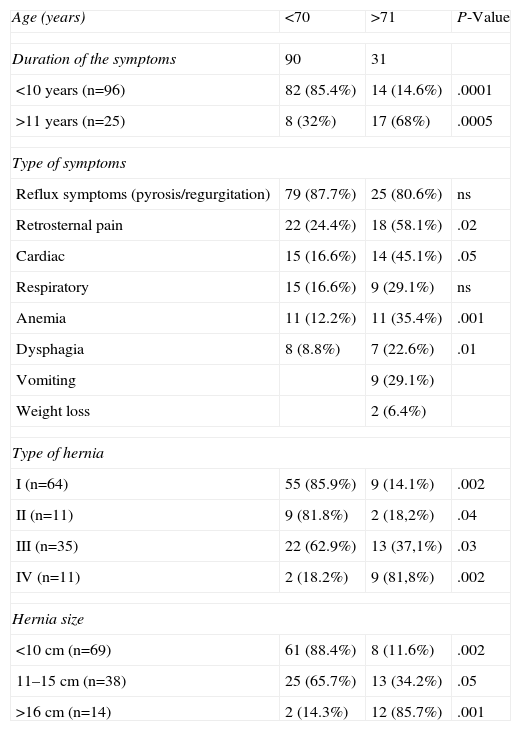
Patients and MethodsThis prospective study included 121 patients (43 men and 78 women) with a mean age of 66.5 years (range 37–88 years), divided into 2 groups: group I, 90 patients aged 70 and under; and group II, 31 patients aged 71 and over. All patients underwent laparoscopic surgery between January 1995 and December 2011. The hiatal hernias were classified in accordance with an international classification3; Table 1 describes the demographic and clinical characteristics of the patients. The patients had a preoperative diagnostic evaluation with endoscopy and barium sulfate swallow radiology, manometry and 24-h pH monitoring. Both immediate and long-term postoperative results were analyzed.
Demographic and Clinical Characteristics of the Patients; n=121.
| Age (years) | <70 | >71 | P-Value |
| Duration of the symptoms | 90 | 31 | |
| <10 years (n=96) | 82 (85.4%) | 14 (14.6%) | .0001 |
| >11 years (n=25) | 8 (32%) | 17 (68%) | .0005 |
| Type of symptoms | |||
| Reflux symptoms (pyrosis/regurgitation) | 79 (87.7%) | 25 (80.6%) | ns |
| Retrosternal pain | 22 (24.4%) | 18 (58.1%) | .02 |
| Cardiac | 15 (16.6%) | 14 (45.1%) | .05 |
| Respiratory | 15 (16.6%) | 9 (29.1%) | ns |
| Anemia | 11 (12.2%) | 11 (35.4%) | .001 |
| Dysphagia | 8 (8.8%) | 7 (22.6%) | .01 |
| Vomiting | 9 (29.1%) | ||
| Weight loss | 2 (6.4%) | ||
| Type of hernia | |||
| I (n=64) | 55 (85.9%) | 9 (14.1%) | .002 |
| II (n=11) | 9 (81.8%) | 2 (18,2%) | .04 |
| III (n=35) | 22 (62.9%) | 13 (37,1%) | .03 |
| IV (n=11) | 2 (18.2%) | 9 (81,8%) | .002 |
| Hernia size | |||
| <10cm (n=69) | 61 (88.4%) | 8 (11.6%) | .002 |
| 11–15cm (n=38) | 25 (65.7%) | 13 (34.2%) | .05 |
| >16cm (n=14) | 2 (14.3%) | 12 (85.7%) | .001 |
Using the laparoscopic approach, a hiatal hernioplasty was performed with fundoplication following previously published techniques.9 The key steps in the surgical technique are: (a) dissection of the hernial sac; (b) reduction of the hernia and removal of adhesions and lipomas, with partial or total resection of the hernial sac; (c) hiatoplasty (with/without mesh, depending on the size of the hernia); (d) fundoplication; and (e) posterior gastropexy.
Statistical AnalysisStatistical analyses were performed in Stata 11.0 using the Student's t test for normally distributed continuous variables, nonparametric Mann–Whitney test for ordinal and continuous variables with non-normal distribution and the chi-squared test to compare proportions. A P<.05 was considered significant (two-tailed).
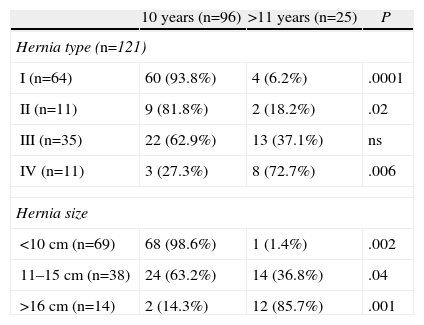
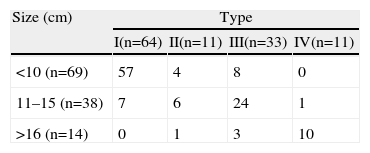
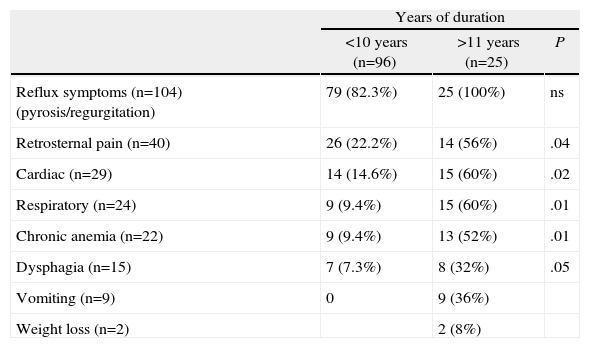
ResultsRegarding the epidemiological characteristics of the patients studied, 85.4% of patients aged 70 and under had symptoms for less than 10 years. On the other hand, in the group of patients aged 71 and older, 68% had more than 11 years of symptom duration, and some had even presented symptoms for 30 years before surgery (Table 1). Symptoms resulting from gastroesophageal reflux were very common, with no statistically significant differences in either patient group (P=ns). However, extraesophageal symptoms were more common in older patients with over 11 years of symptoms and large hiatal hernias. In the group of older patients with longer duration times, we observed complex type iv hernias that were larger in size (Tables 2 and 3). Related symptoms, such as retro-sternal pain and cardiac and respiratory symptoms, were recorded significantly more often in patients with longer symptom duration. Dysphagia and vomiting were also observed in patients with more than 11 years of duration (Table 4).
Symptom Duration and Hernia Characteristics.
| 10 years (n=96) | >11 years (n=25) | P | |
| Hernia type (n=121) | |||
| I (n=64) | 60 (93.8%) | 4 (6.2%) | .0001 |
| II (n=11) | 9 (81.8%) | 2 (18.2%) | .02 |
| III (n=35) | 22 (62.9%) | 13 (37.1%) | ns |
| IV (n=11) | 3 (27.3%) | 8 (72.7%) | .006 |
| Hernia size | |||
| <10cm (n=69) | 68 (98.6%) | 1 (1.4%) | .002 |
| 11–15cm (n=38) | 24 (63.2%) | 14 (36.8%) | .04 |
| >16cm (n=14) | 2 (14.3%) | 12 (85.7%) | .001 |
Type of Symptoms and Years of Symptom Duration.
| Years of duration | |||
| <10 years (n=96) | >11 years (n=25) | P | |
| Reflux symptoms (n=104) (pyrosis/regurgitation) | 79 (82.3%) | 25 (100%) | ns |
| Retrosternal pain (n=40) | 26 (22.2%) | 14 (56%) | .04 |
| Cardiac (n=29) | 14 (14.6%) | 15 (60%) | .02 |
| Respiratory (n=24) | 9 (9.4%) | 15 (60%) | .01 |
| Chronic anemia (n=22) | 9 (9.4%) | 13 (52%) | .01 |
| Dysphagia (n=15) | 7 (7.3%) | 8 (32%) | .05 |
| Vomiting (n=9) | 0 | 9 (36%) | |
| Weight loss (n=2) | 2 (8%) | ||
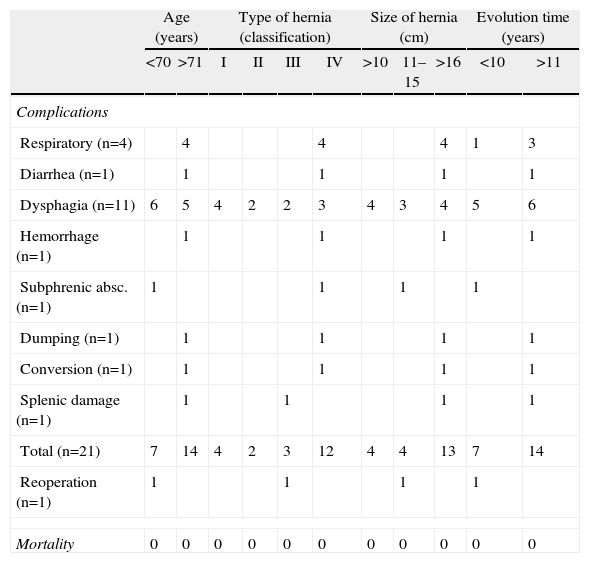
While it is true that the more elderly patients with symptoms over a longer course of time and more complex hernias present a higher risk of complications and postoperative mortality, in our series complications were observed more frequently in the older age group with longer duration of symptoms or in patients with complex type IV hernias. There was no postoperative mortality and only one patient (0.8%) with type III hernia and severe esophagitis needed a reoperation (Table 5). The symptoms observed in patients with hernia recurrence occurred regardless of age, were primarily derived from gastroesophageal reflux and affected 14 patients (11.6%): 4 patients with type I hiatal hernias, one patient treated surgically for type II hernia, 4 patients with type III hiatal hernias and 5 type IV hernias. Thirteen had small type I hernias smaller than 5cm, and their management was medical. Asymptomatic hernias smaller than 3cm (as described during endoscopy or with radiology tests) were not considered recurrences.
Complications and Mortality According to Age and Hiatal Hernia Characteristics.
| Age (years) | Type of hernia (classification) | Size of hernia (cm) | Evolution time (years) | ||||||||
| <70 | >71 | I | II | III | IV | >10 | 11–15 | >16 | <10 | >11 | |
| Complications | |||||||||||
| Respiratory (n=4) | 4 | 4 | 4 | 1 | 3 | ||||||
| Diarrhea (n=1) | 1 | 1 | 1 | 1 | |||||||
| Dysphagia (n=11) | 6 | 5 | 4 | 2 | 2 | 3 | 4 | 3 | 4 | 5 | 6 |
| Hemorrhage (n=1) | 1 | 1 | 1 | 1 | |||||||
| Subphrenic absc. (n=1) | 1 | 1 | 1 | 1 | |||||||
| Dumping (n=1) | 1 | 1 | 1 | 1 | |||||||
| Conversion (n=1) | 1 | 1 | 1 | 1 | |||||||
| Splenic damage (n=1) | 1 | 1 | 1 | 1 | |||||||
| Total (n=21) | 7 | 14 | 4 | 2 | 3 | 12 | 4 | 4 | 13 | 7 | 14 |
| Reoperation (n=1) | 1 | 1 | 1 | 1 | |||||||
| Mortality | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
We should comment on some important points from the analysis of our results and the available literature.
First of all, many authors have suggested that a large number of patients with hiatal hernia are asymptomatic, which is an opinion that we do not share. The most frequently observed symptoms are secondary to gastroesophageal reflux. In older patients with a long duration of the disease, there may be cardiovascular and respiratory symptoms or dysphagia related with the development of large hiatal hernia. This situation carries a risk for severe complications such as gastric volvulus, strangulation, stenosis, gastric ulcers, chronic anemia, gastric retention syndrome, gastric necrosis or acute respiratory pneumonia.14 In their paper, Gongopadhyay et al.5 stated that only 8% of their patients were asymptomatic. It has been reported that the risk of severe symptoms and complications increases annually, and that more than 50% of these patients required emergency surgery.15–23
Another controversial aspect is disease progression. Recent literature has reported the progression of the disease and its complications; therefore, the indication should be done in a timely manner, avoiding emergency surgery in order to reduce postoperative complications and mortality.5,22,24–29 The annual probability of developing acute symptoms is estimated at 1.6% per year, with a risk for presenting acute symptoms of the disease of 18% in patients over the age of 65; after emergency surgery, the risk of mortality is 5.4%. Hill30 reported a 30% risk of complications in patients with hiatal hernia diagnosed 20 years before surgery.
The management of hiatal hernia also creates controversy: conservative treatment or elective surgery? There are several previous studies that reported a 30% higher probability of developing complications in the group of patients who were managed with observation and treatment of symptoms. The conclusion of these studies was to recommend surgery at the time when the hiatal hernia is diagnosed.6,31 If we compare the results reported with elective surgery vs emergency surgery, postoperative mortality after elective surgery is 1.3% (0%–5.2%) while postoperative mortality for emergency surgery ranges between 17% and 54%.32 Based on statistical simulation studies,20 some authors do not support elective surgery in asymptomatic patients; these studies, however, have limitations and have therefore been questioned. In the recent study by Polomsky et al.,6,7 the results demonstrate that patients admitted to the Emergency Department have higher mortality than patients admitted electively (2.7% vs 1.2%, P<.0001) and those who had emergency surgery had 5 times higher postoperative mortality than those who underwent elective surgery (5.1% vs 1.1%, P<.0001). Thus, these results support our position to indicate elective surgery at an early stage. Allen and Jamieson,18,24 who initially suggested conservative management, reported 11% and 20% postoperative mortality after emergency surgery, which is a very high rate compared to elective surgery. This is therefore another argument that supports the indication for early surgery. Silhvo et al. recently reported a mortality rate of 16.4% in symptomatic patients managed with medication and they estimated that 30% of these deaths could have been prevented with early elective surgery.29,33–35
Systematic indication for surgery would prevent postoperative complications. Emergency surgery should be avoided because the mortality estimated in an American study including 1000 hospitals in 22 states was 5.4%. This rate is much higher than postoperative mortality after elective surgery performed in older patients, which does not surpass 0.5%.32
We should also comment on the good current results with laparoscopic elective surgery in high-risk senior patients. This approach is the preferred method of treatment in many institutions. Large series of patients who have been operated on with this technique (including ours) have demonstrated its effectiveness with an acceptable rate of complications and minimal mortality.5,11,16,24,35–38 Postoperative complications ranged from 8% to 28%, but operative mortality is very uncommon (less than 1%) even in elderly patients with high surgical risk. A recent study5 reported 8.5% major complications in patients younger than 65, and 8.5% in those over the age of 75 (P=ns) with an overall mortality of 0.6%. In ASA I–II patients under the age of 65, between 7.5% and 10% presented major complications; in ASA III patients, this level rises to 16%–24% in patients older than 75 (P=.0001).
As for the appearance of ex novo symptoms, dysphagia has been observed in 18% and anatomical failure in 26.1% of patients under age 65 and 27.8% in those older than 75 years, use of proton pump inhibitors in 10%, and a re-operation rate of 3%.8,10,11 Some studies have reported radiological recurrence in up to 66%, but these are hernias measuring less than 5cm, with no clinical repercussions, that are interpreted as hernias and often correspond with a dilated phrenic ampulla and not a true hernia.39
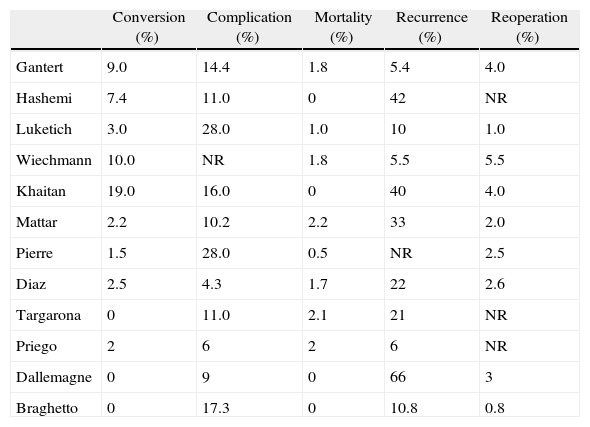
Lastly, the results obtained by our group are comparable to international results (Table 6).
Postoperative Outcome of Patients With Hiatal Hernia Repair: Review of Major Series in the Literature.
| Conversion (%) | Complication (%) | Mortality (%) | Recurrence (%) | Reoperation (%) | |
| Gantert | 9.0 | 14.4 | 1.8 | 5.4 | 4.0 |
| Hashemi | 7.4 | 11.0 | 0 | 42 | NR |
| Luketich | 3.0 | 28.0 | 1.0 | 10 | 1.0 |
| Wiechmann | 10.0 | NR | 1.8 | 5.5 | 5.5 |
| Khaitan | 19.0 | 16.0 | 0 | 40 | 4.0 |
| Mattar | 2.2 | 10.2 | 2.2 | 33 | 2.0 |
| Pierre | 1.5 | 28.0 | 0.5 | NR | 2.5 |
| Diaz | 2.5 | 4.3 | 1.7 | 22 | 2.6 |
| Targarona | 0 | 11.0 | 2.1 | 21 | NR |
| Priego | 2 | 6 | 2 | 6 | NR |
| Dallemagne | 0 | 9 | 0 | 66 | 3 |
| Braghetto | 0 | 17.3 | 0 | 10.8 | 0.8 |
The authors have no conflict of interests to declare.
Please cite this article as: Braghetto I, Csendes A, Korn O, Musleh M, Lanzarini E, Saure A, et al. Hernias hiatales: ¿cuándo y por qué deben ser operadas? Cir Esp. 2013;91:438–443.