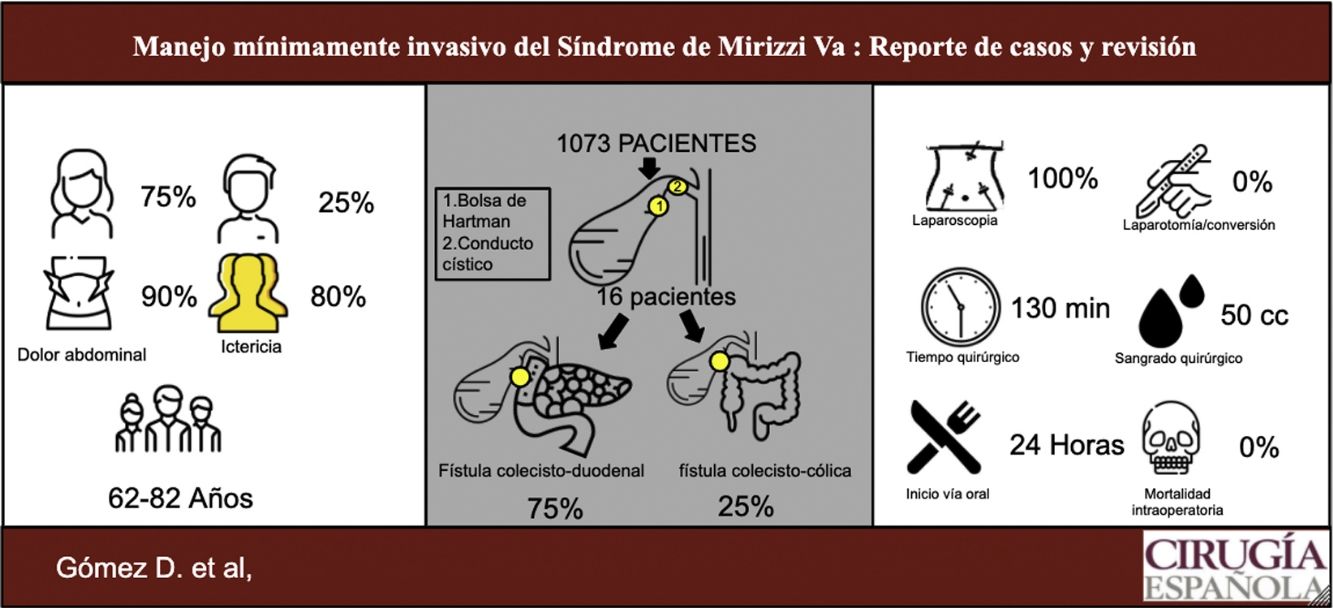
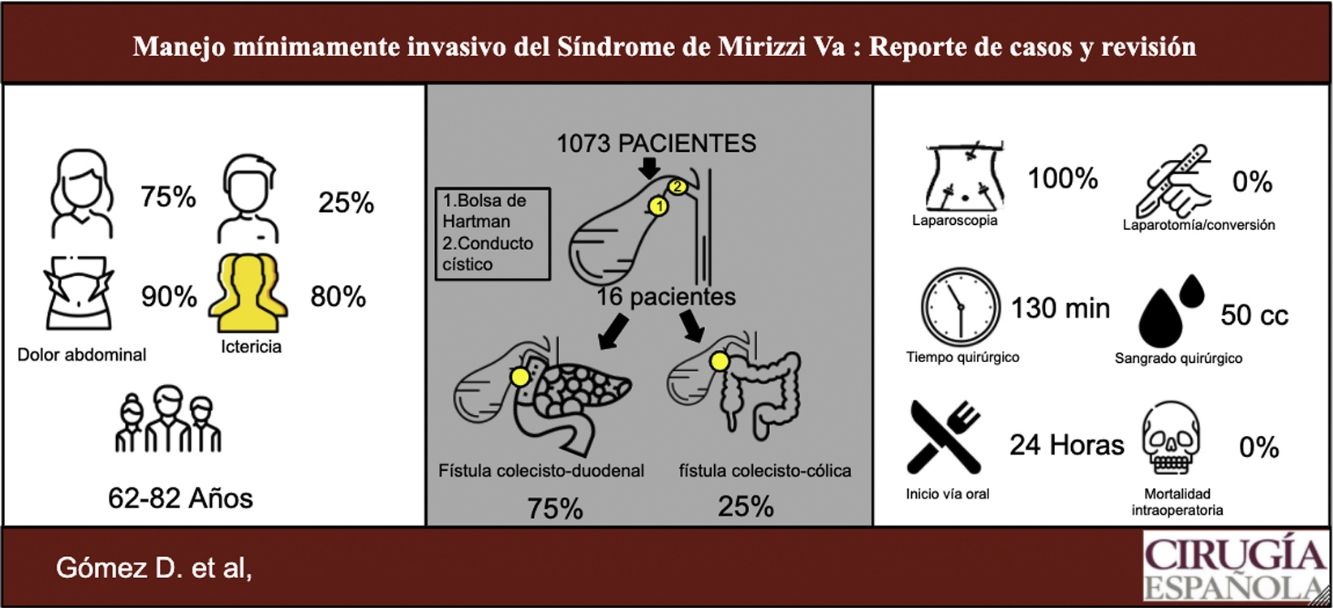
Mirizzi’s Syndrome (MS) is a rare pathology, known to be a challenge for the surgeon. In the surgical management, open approach vs laparoscopic is a topic of discussion due to anatomic variations. The aim of this study is to analyze our experience in the laparoscopic management of this condition in Type Va.
MethodsWe made a descriptive retrospective study of patients diagnosed with MS type Va and treated by laparoscopic approach from 2014 to 2019, in two high volume centers of Bogotá, Colombia.
Results1073 patients who presented complications from gallstones were evaluated, of which 16 were diagnosed with MS type Va. 75% were females and 25% males; 80% presented jaundice and 90% abdominal pain; 12 patients showed cholecystoduodenal fistula and 4 cholecystocolic fistula. All patients underwent laparoscopic management, total cholecystectomy and fistula resection with primary closure was possible on a 100% of the patients. Conversion rate was 0%. The follow up was 18 months.
ConclusionLaparoscopic management of MS is feasible and safe; the experience of the surgery group and selection of the patients is the key to a successful outcome.
El síndrome de Mirizzi (SM) es una patología infrecuente que es un reto para el cirujano. En el manejo quirúrgico, el abordaje abierto o el laparoscópico es un punto de discusión debido a la distorsión anatómica que se presenta. El objetivo de este estudio es analizar nuestra experiencia en el manejo laparoscópico de esta condición en el tipo Va.
MaterialesRealizamos un estudio descriptivo retrospectivo de pacientes con diagnóstico de SM tipo Va y tratados por abordaje laparoscópico, entre el 2014 y 2019, en dos centros de alto volumen de Bogotá, Colombia.
ResultadosSe evaluaron 1.073 pacientes que presentaron complicaciones por cálculos biliares, de los cuales 16 fueron diagnosticados con SM tipo Va. El 75% eran femeninos y el 25% masculino; el 80 % presentó ictericia y el 90% dolor abdominal. Doce pacientes presentaron fístula colecistoduodenal y cuatro fístula colecistocólica. Todos se manejaron de manera laparoscópica, en el 100% se logró realizar colecistectomía total y resección de fístula con cierre primario. La tasa de conversión fue del 0%, no hubo reingresos ni reintervención. El periodo de seguimiento fue de 18 meses.
ConclusiónEl manejo laparoscópico en el SM es posible y seguro, teniendo en cuenta la experiencia del grupo quirúrgico y realizando una adecuada selección de los pacientes.
Mirizzi’s syndrome (SM) is a rare complication of cholecystitis, characterised by the presence of one or more stones, which are impacted in Hartmann’s pouch or in the cystic duct, causing compression of the extrahepatic bile duct1,2. The pathophysiology is that this impaction associated with recurrent inflammatory processes leads to the formation of a fistula between the gallbladder and the bile duct or neighbouring organs, such as the duodenum, colon or stomach1,3.
This condition is rare, with an incidence in developing countries of 4.7%–5.7%, while in developed countries it is lower than 1%2. It usually occurs in people aged 40–70 years and may be an incidental finding in 0.06–5.7% of patients undergoing cholecystectomy1,4.
This manifestation in the bile duct is a challenge for surgeons because of the difficulty it presents in diagnosis and treatment1,5–7. Over the years, it has been classified in different ways, depending on the involvement of the common bile duct (CBD) and the presence of fistula. Currently, the Csendes classification modified by Beltran is the most widely used8. Surgical management of this pathology varies according to this classification, with the open and/or minimally invasive approach being a point of discussion5,6,9,10. We therefore conducted a retrospective study on the minimally invasive approach to type Va MS, in addition to a comprehensive review of the literature.
Materials and methodsThis is a retrospective descriptive study of patients with a diagnostic finding of type Va MS, who were referred for laparoscopic management, in two referral and high-volume centres in Bogotá, Colombia, between the periods of January 2014 and January 2019 (five years). The research protocol was presented at both institutions and approved by each ethics committee. All patients and relatives were informed of the approach, benefits, possible complications and, in the case of intraoperative findings, the need for conversion to open surgery. The following variables were evaluated: age, sex, diagnosis, surgery time, bleeding, biliary leakage, fistulas, conversion rates, tolerance to oral feeding, intensive care unit (ICU) stay, hospitalisation time, need for reoperation, incidence of stenosis, mortality, and incidence of cholangiocarcinoma with a postoperative follow-up of at least one year.
All patients had a pre-anaesthetic and multidisciplinary assessment, performed by the anaesthesiology, internal medicine and surgical department of each institution. All authors were informed and followed the guidelines of the Declaration of Helsinki and good clinical practice guidelines.
In addition, a review of the literature was carried out, taking into account studies published in scientific journals indexed in the PubMed database over the last 10 years, with which a comparative analysis was made with the variables obtained in our study. We included patients over 18 years of age, with a diagnosis of type Va MS who were taken for laparoscopic management, excluding patients with Child-Pugh B or greater liver cirrhosis, suspected malignancies such as extrinsic compressions. In this study we analysed comorbidities, epidemiological data of the population, intervention performed on patients, procedure undergone, morbidity and mortality and postoperative outcome.
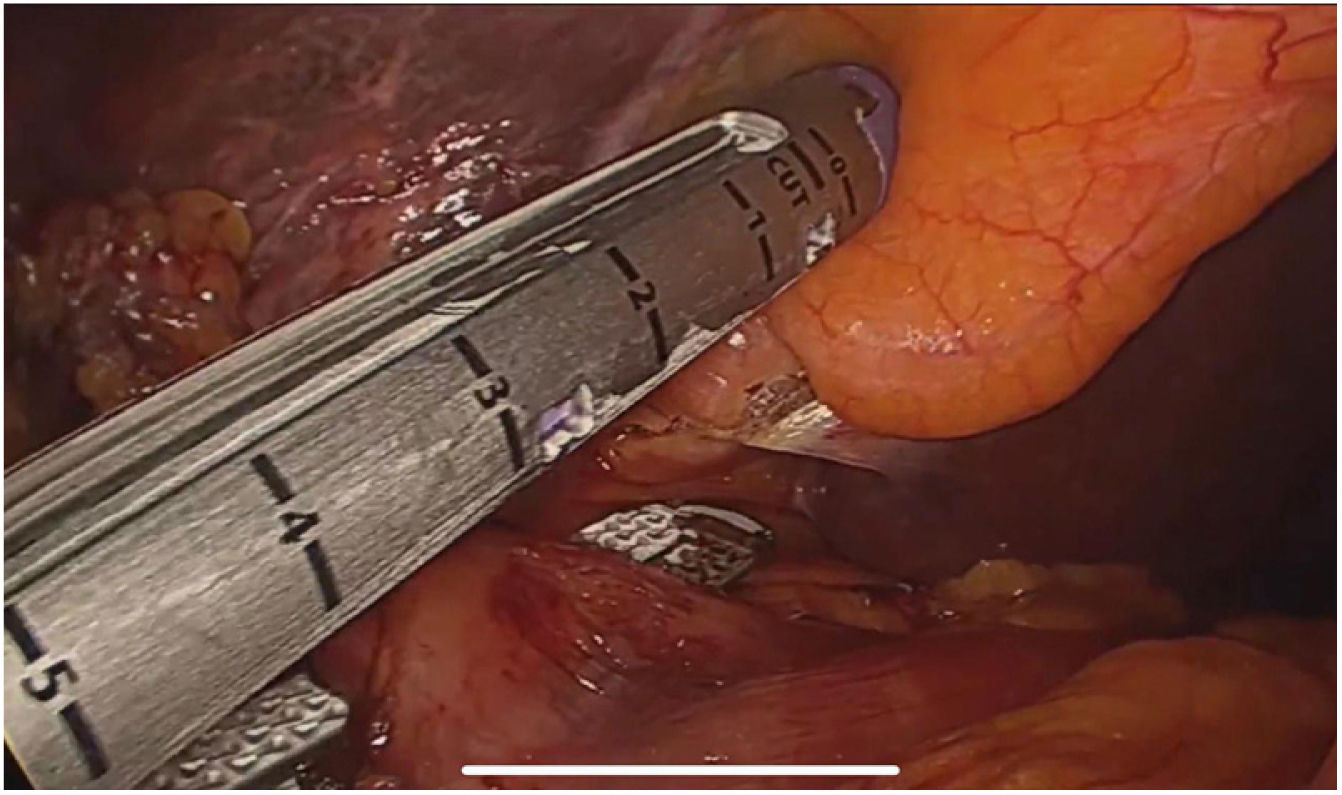
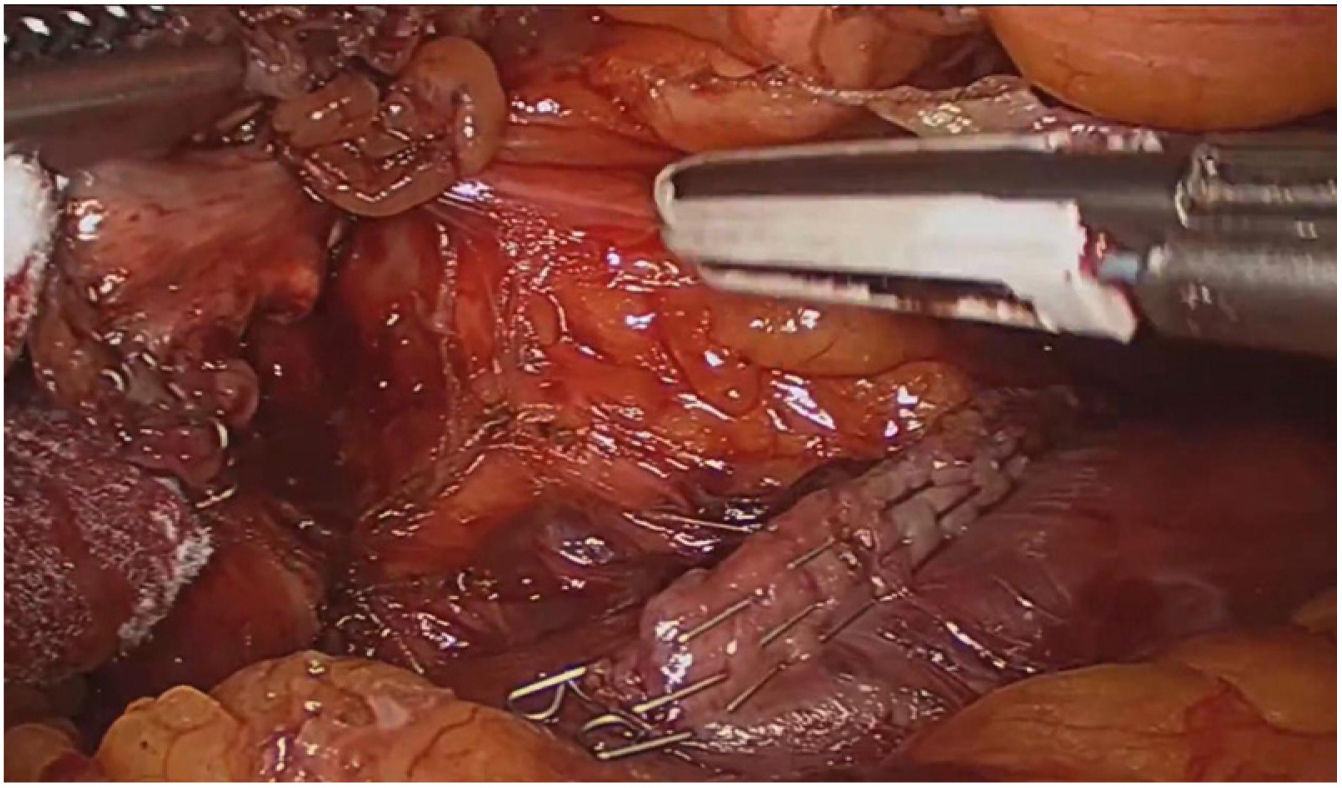
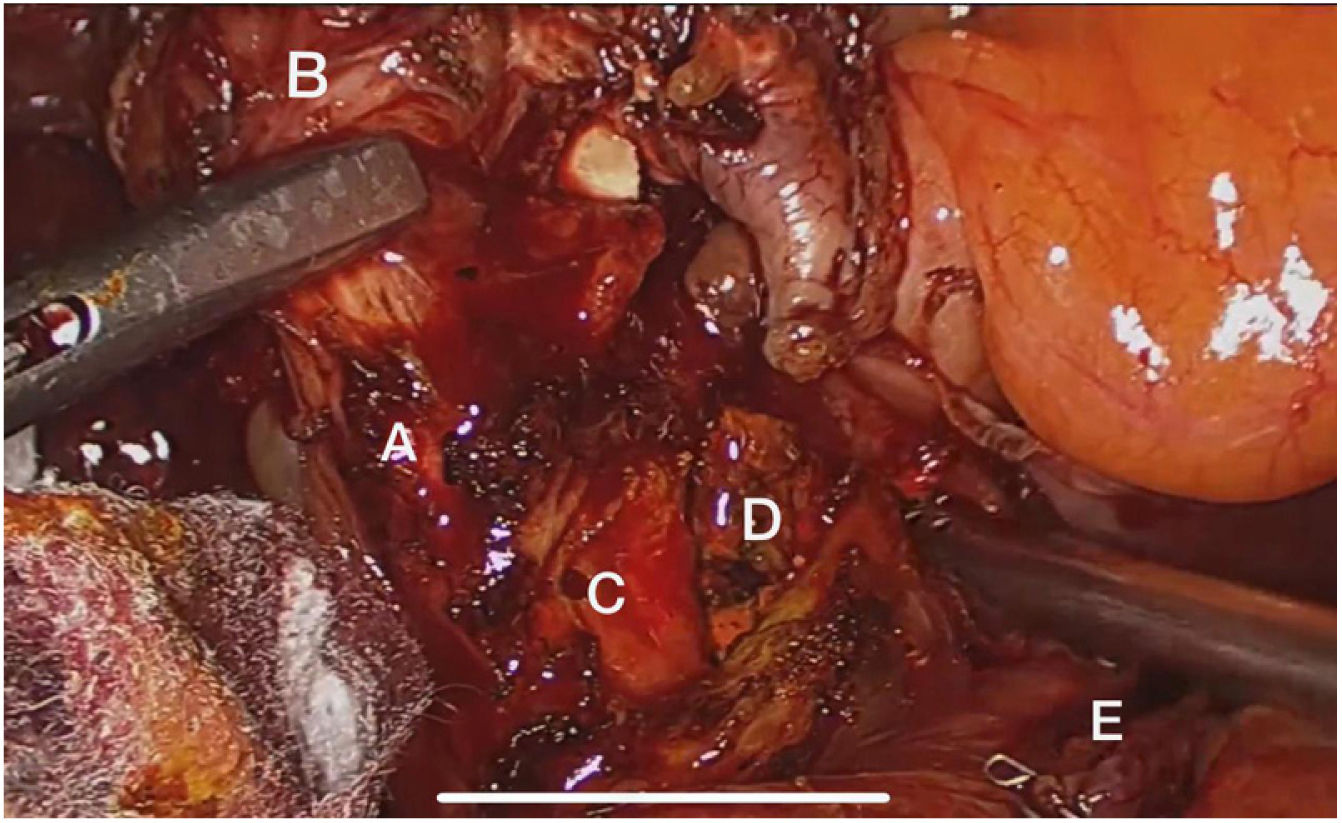
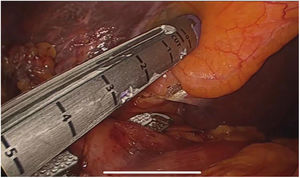
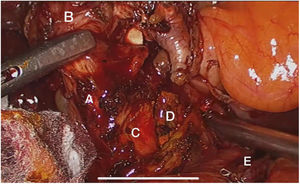
Surgical techniqueThe approach was performed by inserting the initial trocar through the open Hasson umbilical technique, the trocars were arranged as follows: 12 mm umbilical trocar, 12 mm trocar in the epigastrium, one to two 5 mm trocars in the right hypochondrium, according to need, blunt dissection was performed with a surface sealing electroscalpel (Ligasure Blunt Tip 5 mm), complete dissection of the fistula, resection and closure of its duodenal or colonic border with a single shot of Endo Gia 60 mm purple; Once closure of the cholecystoenteric fistula was achieved, dissection of the hepatocystic triangle was performed until the critical safety view was obtained and total cholecystectomy was performed. The specimens were extracted by endobag (saline bag) and a subhepatic drain was used in all cases and removed prior to discharge.
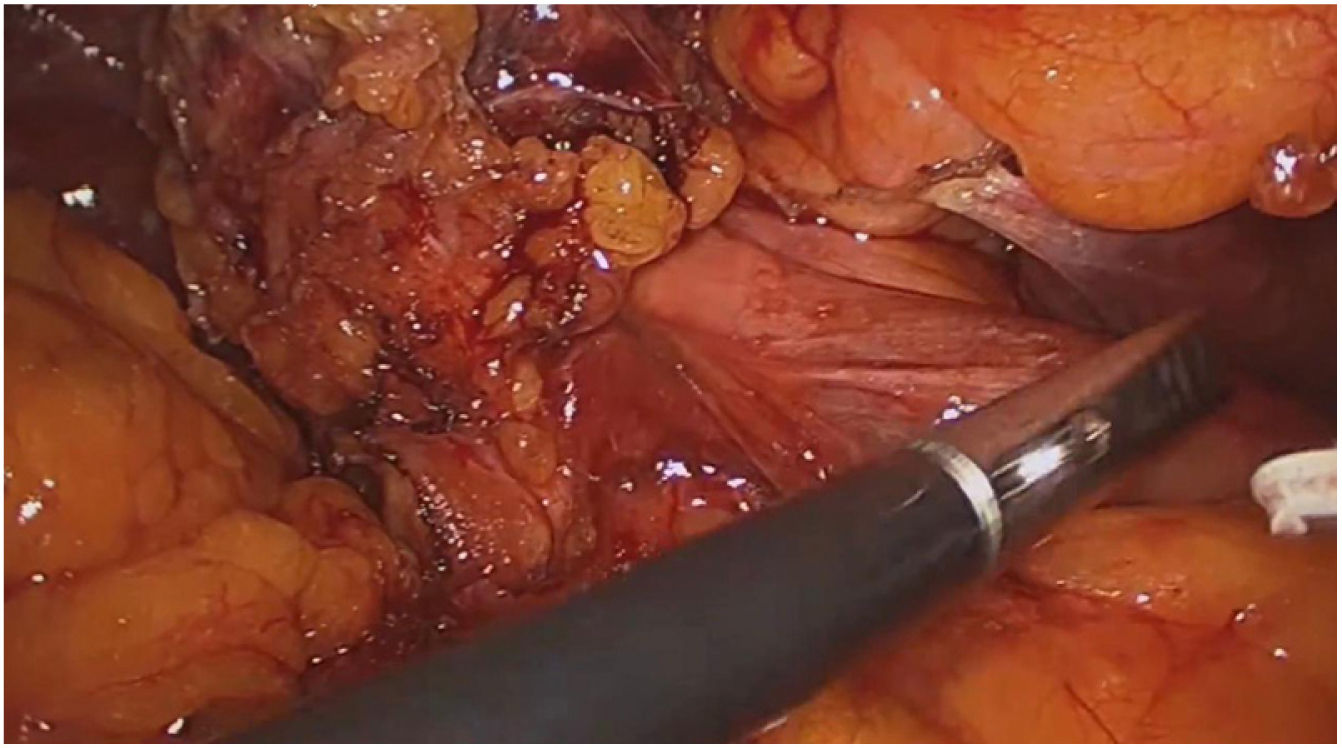
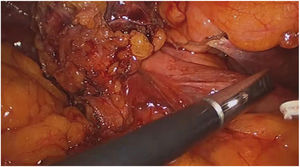
ResultsA total of 1,073 patients presented with gallstone complications, 16 were diagnosed with Va MS, 12 patients (75%) had cholecystoduodenal fistula (Fig. 1) and four (25%) cholecystocolonic fistula, all cases were managed by laparoscopic approach. Twelve (75%) patients were female and four (25%) were male in a F/M ratio of 3:1. The mean age was 72.3 years (range 62–82), the sociodemographic variables of the patients are summarised in Table 1. Seventy per cent of patients had total bilirubin above 4 mg/dL, alkaline phosphatase levels in the range 300 to 984 IU/L.
Sociodemographic patient variables.
| Variable | Percentage (n) |
|---|---|
| Gender | |
| Male | 25% (4) |
| Female | 75% (12) |
| Age | 72.3 years (62–82) |
| Initial clinical presentation | |
| Abdominal pain | 80% |
| Jaundice | 90% |
| Fever | 30% |
| Comorbidities | |
| High blood pressure | 80% |
| Hypothyroidism | 20% |
| Diabetes mellitus | 70% |
| Heart failure | 10% |
| Laboratory | |
| Total bilirubin | |
| >4 mg/dL | 70% (11) |
| <4 mg/dL | 30% (5) |
| Alkaline phosphatase | 300–984 UI/L |
The diagnosis was suspected by ultrasound in five patients (31.25%), of which all were confirmed by other imaging modalities; in three patients it was confirmed by computed tomography (CT), in the remaining two by magnetic resonance cholangiopancreatography (MRCP). Of the 16 patients, another two patients (12.5%) were diagnosed by endoscopic retrograde cholangiopancreatography (ERCP) and finally, the majority of cases, nine patients (56.25%) were incidental findings during surgery.
The laparoscopic approach was performed in 100% of cases with total cholecystectomy and correction of the fistula by resection and closure (Figs. 2–4). The average operative time was 130 min (90–150) and an average bleeding of 50 cc (20–100). There was no need for conversion to open surgery.
Onset and tolerance to the oral route in all patients was 24 h after the surgical procedure. Three patients required ICU admission for comorbidities. No complications related to the intervention were evidenced and no presence of gallbladder cancer was evidenced in the pathological examination in our population. The average length of hospital stay was four days (range 3–9), no patient required reoperation, and no readmission associated with the procedure was recorded in the following 30 days. Additional complications such as surgical site infections, residual choledocholithiasis or biliary leakage did not occur. Follow-up time averaged 18 months (12–25 months), during which two mortalities at six months associated with comorbidities (pneumonia and heart failure) were evident. In the follow-up of the remaining 14 patients, no additional complications occurred, the outcomes are described in Table 2.
Postoperative outcomes and complications.
| Laparoscopic approach | 16 (100%) |
| Conversion | 0 (0%) |
| Time in surgery | 130 min (90–130) |
| Bleeding | 50 cc (20–100) |
| Onset and tolerance of oral route | 24 h |
| Hospital stay | 4 days (range 3–9) |
| Readmissions | 0 |
| Reinterventions | 0 |
| Surgical site infection | 0 |
| Biliary leakage | 0 |
| Surgical procedure-associated mortality | 0 |
| Non surgical procedure-associated mortality | 2 (12.5%) |
The first to mention this pathology were Ruge and Kehr in 1900, but it was not until 1948 that it was given this name by the Argentinean surgeon Pablo Mirizzi2,6. This condition is more frequent in women10,11, and an anatomical predisposing factor is when the cystic duct is longer and with a low insertion8.
This syndrome develops when there is an impaction of a stone in the infundibulum that predisposes patients to repeated cholecystitis. Over time, an inflammatory process develops, leading to atrophy of the gallbladder walls5. These are formed when the impacted stone completely obliterates the cystic duct and, due to the pressure exerted, forms an ulcer that eventually comes into contact with the bile duct, which subsequently erodes, creating a communication between the two spaces8. Depending on the location of the calculus and the compression it generates on the adjacent structures, ulcers will form which will eventually end in fistulas in the different anatomical portions, and this is how cholecystoenteric fistulas are produced8. The most common (75%) is cholecystoduodenal, followed by cholecystocolonic (10–20%), as shown in our cases, and the other 15% in other less frequent locations, such as the stomach12.
MS is characterised by chronic inflammation of the gallbladder and its classification depends on the presence or absence of a fistula2. Although there are multiple classifications, the most widely used was the one described by Csendes and modified by Beltrán, which classifies this syndrome into five types8. Type I refers to an external compression of the common bile duct, without the presence of a fistula; type II is the presence of a cholecystobiliary fistula with involvement of less than one third of the circumference of the CBD, while type III is a fistula that covers up to two thirds of the circumference8. Type IV is a fistula with total obliteration, forming a fusion between the gallbladder wall and the CBD8. Finally, type V is the presence of a cholecystoenteric fistula and is subdivided into Va (without biliary ileus), like the population in our study, and Vb (with biliary ileus)2,5,8. According to the literature, the most frequent type is type I, with a reported frequency of 10.5%–51%, while the least common are types IV and V, with a range of 1%–4%; the remaining types account for 29% of cases6.
The symptoms reported by these patients are not specific and may vary from case to case2. Manifestations may include vomiting, fever, constipation, nausea, jaundice and pain in the right hypochondrium, as well as laboratory alterations, such as elevated transaminases, leukocytes, bilirubin and alkaline phosphatase1,2,5, as seen in 70% of our patients. All this makes diagnosis difficult and still remains a clinical challenge5.
Preoperative diagnosis varies widely due to the infrequent occurrence of MS and the non-specific clinical presentation and this is reported with great variability in the literature between 8% and 63%10 It is also reported that it can be found incidentally between .06% and 5.7% during cholecystectomies and in 1.07% during ERCP1. However, if this pathology is suspected, it can be detected by imaging studies2, thus allowing a surgical strategy to be planned to reduce the risk of complications, such as bile duct injury, which has been described in up to 17%10. Abdominal ultrasound has a sensitivity of 8.2%–27% and an accuracy of 29%1,4; if this is suggestive of disease, an additional study should be performed to confirm the pathology5. Another method is the use of computed tomography, which has a sensitivity of 42%–50%2,9 and although the findings are not specific for MS, it helps to differentiate between neoplasia and fistula1,10. ERCP is considered the gold standard1, as it has a sensitivity of 77.8%–100% and a specificity of 93.5%1. It has the advantage of identifying the point of obstruction or fistulae, if present, and can be therapeutic in resolving CBD obstruction, but it must be borne in mind that this procedure is invasive, and may lead to additional complications1,10. Magnetic resonance cholangiopancreatography4, which has a sensitivity of 77%–100%2 and a specificity of 93%, is one of the best non-invasive studies to identify the anatomy of the bile duct and rule out other causes of CBD obstruction. In 31.5% of our patients, the ultrasound showed alterations suggestive of MS and the complementary studies described were performed to confirm the diagnosis; however, as reported in other series, most of the cases were incidental findings10.
The treatment of MS remains a challenge for surgeons1,8, due, as previously explained, to the infrequent nature of the pathology and the fact that most of the time the condition is not known until surgery. Surgical management depends on the type of MS, and includes the open approach, or the minimally invasive approach including laparoscopy or robotic-assisted laparoscopy1.
The open approach by laparotomy is considered the management of choice because it has a broader view of the anatomy, and allows the surgeon to feel the anatomical structures and identify and remove the embedded stone before performing the cholecystectomy, but it is an invasive procedure and has been associated with increased morbidity1.
In the past, the use of the laparoscopic approach was considered a contraindication due to possible complications, including damage to the bile duct and a high conversion rate of 31%–100%. However, thanks to all the advances in surgery, the increased experience and surgical skill, it no longer poses a restriction to treat this pathology laparoscopically, including the more complex types of MS2,7.
In the literature review, laparoscopy is only recommended in type I and some type II cases1,9,11,13. Due to the diversity of anatomy in laparoscopic cases, it is suggested that cholangiography be performed prior to gallbladder removal12 and a T-tube be placed in the MS, greater or equal to type II at the level of the bile duct to allow decompression and thus avoid bile leaks and stenosis1,9,11. Subtotal cholecystectomy, because the gallbladder is usually fibrous and attached to the CBD, is an option for some authors in the management of mainly type I and II MS, thus leaving a gallbladder remnant to avoid complications associated with risky dissection of the hepatocystic triangle13,14. Recently, Nag and Nekarakanti conducted a comparative study of the open and laparoscopic approaches, showing that the laparoscopic approach could reduce the rate of complications, intraoperative blood loss and hospital stay15.
In type Va MS, as one of the rarest types, management is not standardised, and evidence has only been obtained from case reports and retrospective case series2,9,16. In the case reports of this type of laparoscopic management, such as those by Shirah et al., Lledó et al. and Nag and Nekarakanti, patients with type Va MS were not included, or the management used in this group was not described9,13,15.
In our review of laparoscopic management, Yetişir et al. are the only group to report their successful experience with the approach to a case of type Va MS, with a cholecystocolonic fistula using trilinear mechanical suture and performing a subtotal cholecystectomy, without showing any complications in a follow-up of eight months12. Hence, the importance of our cases in the management of this pathology. Our study shows that the minimally invasive approach in patients with type Va MS is not inferior compared to the conventional open approach reported; carefully performing closure of the enteric fistula without stenosing the lumen of the gastrointestinal tract and performing careful dissection of the hepatocystic triangle until the critical safety view is obtained to avoid performing subtotal cholecystectomy and reducing the risk of subsequent episodes of pancreatitis12. But to obtain these results, like many authors, we must emphasise proper patient selection9,13,15.
This study is limited by its retrospective design and number of patients, but given our results and this being the series with the largest number of cases of type Va MS, we propose that total cholecystectomy, resection and primary fistula closure by laparoscopy is a possible option for management in this group of patients, without complications at one and a half years of follow-up. We consider that the expertise of the surgical team is a very important factor to be taken into account, since, in our case, we are a reference centre with a high volume of biliary pathology, so we have experience in the management of challenging dissections in this type of anatomical complexity, even performing, when necessary, minimally invasive bilioenteric reconstructions, as we have described in other studies.
To conclude, we can say that Mirizzi syndrome is a rare pathology, which occurs as a complication of cholecystitis, so its infrequency and non-specific clinical presentation makes it difficult to diagnose. It is important, therefore, given clinical suspicion, to use the necessary tools for a preoperative diagnosis and make an adequate planning of management. However, most cases will be detected during surgery, so the surgeon must have adequate knowledge of the different techniques for correction, according to each type. Currently, the most accepted approach is the open approach for type III and above, but laparoscopic management is increasing as surgeons gain more experience, thus demonstrating that minimally invasive management is safe and has advantages over the traditional approach, as demonstrated in our 16 cases of type Va MS, in which all patients underwent laparoscopic surgery, without any conversion to open surgery, and with no in-hospital complications or complications during follow-up.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Gómez D, Pedraza M, Cabrera LF, Mendoza Zuchini A, Arrieta G M, Aparicio BS, et al. Manejo mínimamente invasivo del síndrome de Mirizzi Va: Reporte de casos y revisión narrativa de la literatura. Cir Esp. 2022;100:404–409.