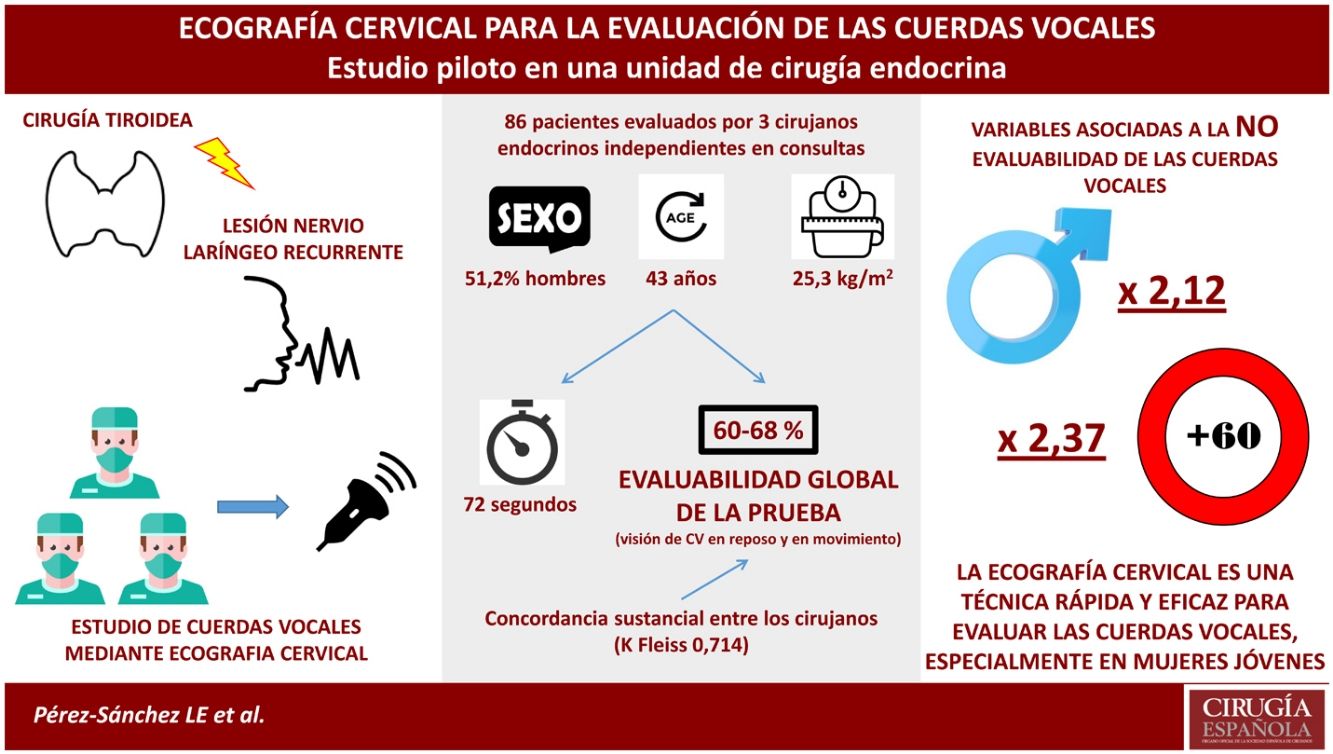
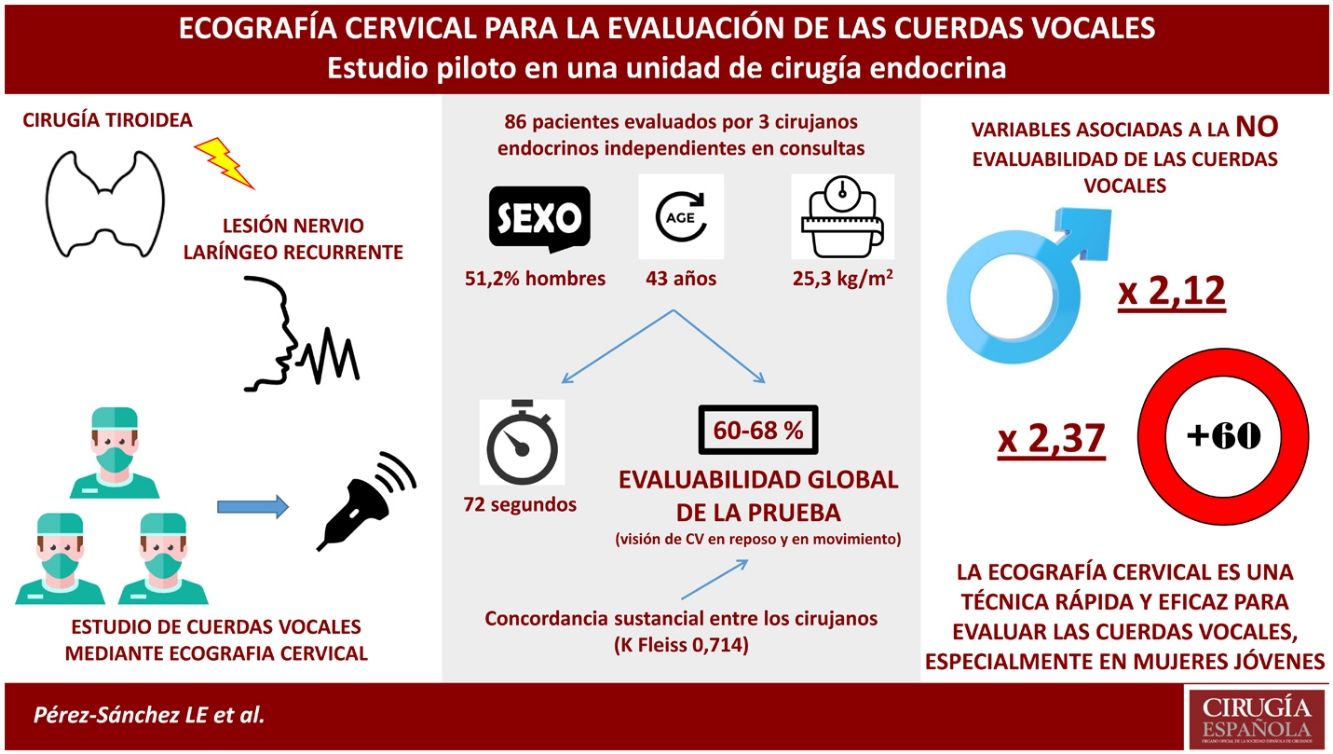
Cervical ultrasound (CE) has emerged as a promising tool in recent years for vocal cord (VC) assessment in patients undergoing thyroid surgery. Our aim is to assess the reliability of CE once implemented in an endocrine surgery unit and performed by the surgeons themselves.
Material and method86 participants with no history of laryngeal pathology or cervical surgery underwent CE by three independent endocrine surgeons. Laryngeal structures and specifically the VCs were analysed. To consider the examination as diagnostic, the VCs had to be visualised statically and during phonation. The time taken to perform the technique and the interobserver variability were also analysed.
ResultsOf the 86 participants, 51.2% were male with a mean age of 43 years. The range of diagnostic examinations between surgeons was 60–68%, with substantial agreement between the 3 explorers (Fleiss’s K-value = .714). Male sex and advanced age were factors associated with non-assessability of the technique. The mean procedure time was 72 s.
ConclusionsCE is a fast, non-invasive, feasible bedside tool useful for the assessment of VCs prior to thyroid surgery, mainly in young women.
La ecografía cervical (EC) ha surgido como una herramienta prometedora en los últimos años para la evaluación de las cuerdas vocales (CV) en pacientes sometidos a cirugía de tiroides. Nuestro objetivo es valorar la fiabilidad de la EC una vez implementada en una unidad de cirugía endocrina y realizada por los propios cirujanos.
Material y métodoSe incluyeron 86 participantes sin antecedentes de patología laríngea ni cirugía cervical a los que se les realizó una EC por parte de 3 cirujanos endocrinos independientes. Se analizaron las estructuras laríngeas y específicamente las CV. Para considerar la exploración como diagnóstica, debían visualizarse las CV de manera estática y durante la fonación. También se analizó el tiempo de realización de la técnica y la variabilidad interobservador.
ResultadosDe los 86 participantes, el 51,2% fueron varones y una edad media de 43 años. El rango de exploraciones diagnósticas entre los cirujanos fue de 60–68%, con una concordancia sustancial entre los 3 exploradores (valor K de Fleiss’s = 0.714). El sexo masculino y la edad avanzada fueron factores asociados a la no evaluabilidad de la técnica. El tiempo medio del procedimiento fue de 72 segundos.
ConclusiónLa EC es una herramienta rápida, no invasiva, viable a pie de cama y útil para la evaluar las CV antes de la cirugía tiroidea, principalmente en mujeres jóvenes.
Thyroidectomy is one of the most commonly performed procedures in general surgery. Injury to the recurrent laryngeal nerve (RLN) is a very serious complication during thyroid surgery. Bilateral RLN palsy is considered a rare but life-threatening event. However, unilateral vocal cord (VC) paralysis occurs more frequently and does not usually have a clinical impact on the voice. In fact, asymptomatic unilateral RLN lesions have been shown to account for 67% of all cases of RLN palsy.1
Such complications are of concern not only for patients, who may subsequently develop multiple types of physical and psychosocial sequelae,2 but also for surgeons, as they are a common cause of medico-legal claims.3
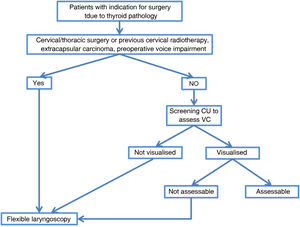
Therefore, assessment of VC function is nowadays necessary in patients in whom a total thyroidectomy is planned, in those with previous cervical operations or with previous voice impairment.4 Flexible laryngoscopy (FL) is currently considered the gold-standard for the assessment of VC function.5 Although widely available, FL is an invasive procedure and, at least in our setting, requires evaluation by an ENT specialist.
In recent years, cervical ultrasound (CU) has proven to be a promising tool in the assessment of VC function and has been used in some high-volume thyroid surgery centres with good results.6,7 Unlike FL, CU is a non-invasive procedure performed in the same pre-surgical consultation that can be routinely performed by endocrine surgeons. Although CU appears to be a promising technique in this field, little has been studied on its implementation and use by thyroid surgeons.
The aim of our study is to assess the reliability of CU once implemented in an endocrine surgery unit and performed by endocrine surgeons themselves.
MethodsWe conducted a prospective study between 1 January and 28 February 2021, to assess the ability of 3 independent endocrine surgeons to assess laryngeal structures using CU with special emphasis on VC mobility.
Eighty-six subjects were included in the study consecutively and blinded to the surgeons who were to perform the ultrasound. All participants were selected during surgical consultations not related to thyroid or cervical diseases. Patients with previous cervical procedures (surgery or radiotherapy), known laryngeal conditions or any previously known voice disturbance were excluded. Demographic variables such as height, weight, age and sex were recorded. Informed consent was obtained from all participants.
Three independent endocrine surgeons, with no previous ultrasound experience, were trained by a CU specialist for 6 months. Each surgeon performed more than 100 supervised procedures before starting the study.
The examination was performed in an isolated room where only one surgeon and one participant could be present. The latter remained in the room until the 3 independent assessments were performed. Each subject was not allowed to speak prior to the scan to avoid providing any additional information to the operator. Each surgeon had a maximum of 180 s to perform the assessment, but in case the scan ended earlier, the surgeon had to remain in the room until the time was up. Each participant was placed in a supine position on a stretcher with the neck in hyperextension and arms at the sides of the body. A portable ultrasound system (SonoSite M-Turbo Portable UltrasoundSystem, Fujifilm, USA) with a 5−10 MHz linear transducer was used and placed transversely over the anterior surface of the neck. The ultrasound technique used consisted of a systematic scan from the floor of the mouth to the second tracheal cartilage. During the procedure, the laryngeal structures at rest were initially assessed: thyroid cartilage, free edge of the VCs, VC muscles and arytenoid cartilage. Once all laryngeal structures were identified, the mobility of the VCs was analysed by asking the subject to pronounce an /i:/ sound continuously in a soft voice and monitoring the vibration of the VCs in adduction. The ultrasound patterns described by Singh et al. in 20098 were followed.
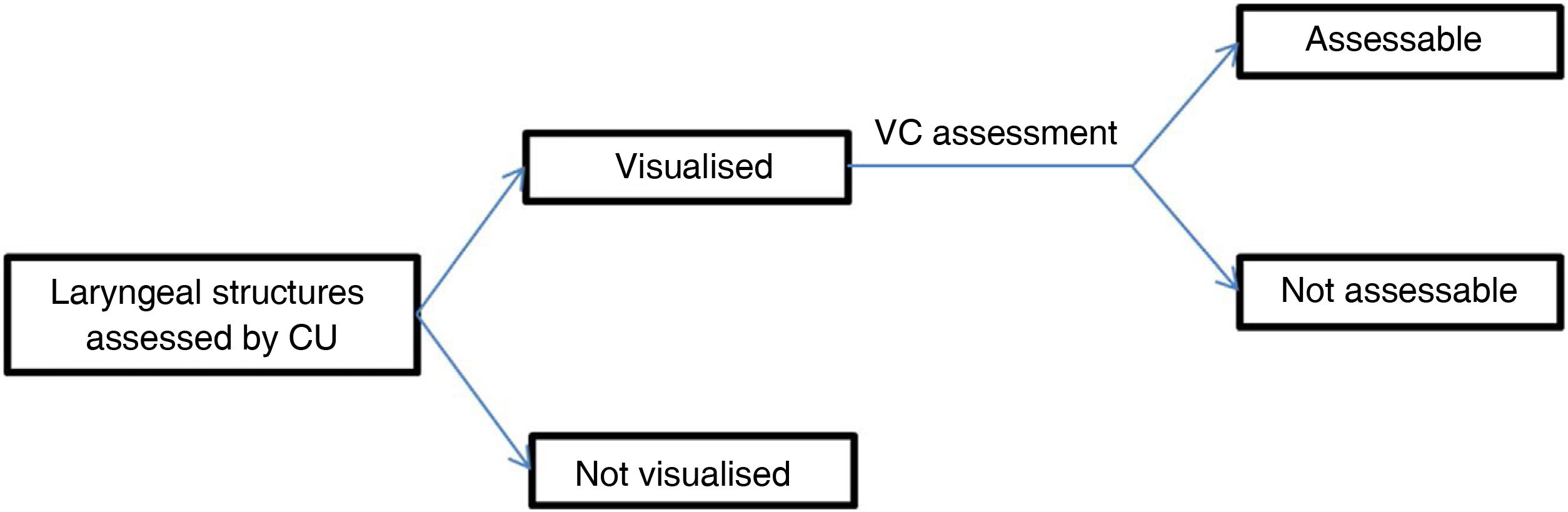
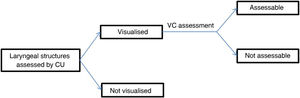
After evaluation of the laryngeal structures our findings were classified as visualisable, when we were able to distinguish these structures bilaterally using CU, and non-visualisable otherwise. Specifically, in the case of the evaluation of the VCs these were categorised as evaluable when in addition to being visualised (free edge of the VCs) we were able to determine their mobility; those where movement could not be seen were classified as not evaluable (Fig. 1). After the procedure each surgeon fills in a checklist per subject describing the laryngeal structures with the described details.
Statistical analysis was performed using R 4.0 (A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org). Continuous variables were expressed as median and interquartile range, while qualitative variables were expressed as frequency and percentage. To assess inter-operator agreement, Fleiss’ kappa analysis was performed, calculated using the SPI function of the REL package (RiccardoLoMartire [2020]. rel: Reliability coefficients. R package version 1.4.2. https://CRAN.R-project.org/package=rel). Cochran's Q test was used to test for equality between several related samples on a dichotomous variable. The Poisson regression model was used to determine the rate of any variable associated with the non-assessability of the technique. The Kaplan–Meier and log-rank test was used to analyse the relationship between procedure time and assessability. A p-value of less than .05 was considered statistically significant.
ResultsOur study included a sample of 86 consecutively selected participants in the general surgery practice. Their ages ranged from 18 to 75 years, with a mean age of 43 years. The sex ratio showed an equal distribution and, in terms of BMI, our sample showed a prevalence of normal weight (18.5−24.9 kg/m2) and overweight (25−29.9 kg/m2) subjects (48% and 36%, respectively) (Table 1).
Baseline characteristics of the subjects studied.
| N = 86 | |
|---|---|
| Age (years), median (IQR) | 43 (28−58) |
| Male sex, n (%) | 44 (51.2) |
| Height (m), median (IQR) | 1.68 (1.62−1.77) |
| Weight (kg), median (IQR) | 72 (65−81) |
| BMI (kg/m2), median (IQR) | 25.28 (23−28.19) |
| Normal weight (BMI 18.5−24.9), n (%) | 41 (48) |
| Overweight (BMI 25−29.9), n (%) | 31 (36) |
| Obesity grade i (BMI 30−34.9), n (%) | 8 (9) |
| Obesity grade ii (BMI 35−39.9), n (%) | 4 (5) |
| Obesity grade iii (BMI 40−49.9), n (%) | 2 (2) |
BMI: body mass index; IQR: interquartile range.
After assessment of the cervical region using CU, the thyroid cartilage and VC muscle were the best visualised anatomical structures (overall rate 98% and 90%, respectively). All 3 surgeons described a similar ratio. The overall mean procedure time was 72 s, with a maximum difference between operators of 6 s on average (Table 2).
Results of the cervical assessment using cervical ultrasound.
| Operator A | Operator B | Operator C | |
|---|---|---|---|
| Technique time, (sc), median (IQR) | 61.5 (49.2−86.8) | 76 (56.2−94.8) | 67.5 (51.2−88) |
| Thyroid cartilage, % | 96.5 | 97.7 | 98.8 |
| VC muscle, % | 91.9 | 87.2 | 88.4 |
| VC free margin, % | 75.6 | 73.3 | 69.8 |
| Arytenoid cartilage, % | 67.4 | 61.6 | 62.8 |
| Assessable VC, % | 68.6 | 62.8 | 60.5 |
IQR: interquartile range; VC: vocal cord.
Although in this study CU was not compared to a gold-standard technique, the concordance of assessability between the 3 operators was substantial, with a Fleiss K-value of .714. Table 3 shows the degree of agreement between each pair of operators. Likewise, no statistically significant differences were found in the assessability index between the 3 surgeons (p = .10) after performing a Cochran’s Q test.
After applying the Poisson regression model, gender and age were identified as independent variables associated with the non-assessability of the technique. The incidence rate in men was 2.12 (p < .001) and in patients older than 60 years was 2.37 (p < .001). BMI was not identified as a variable associated with the non-assessability of the technique.
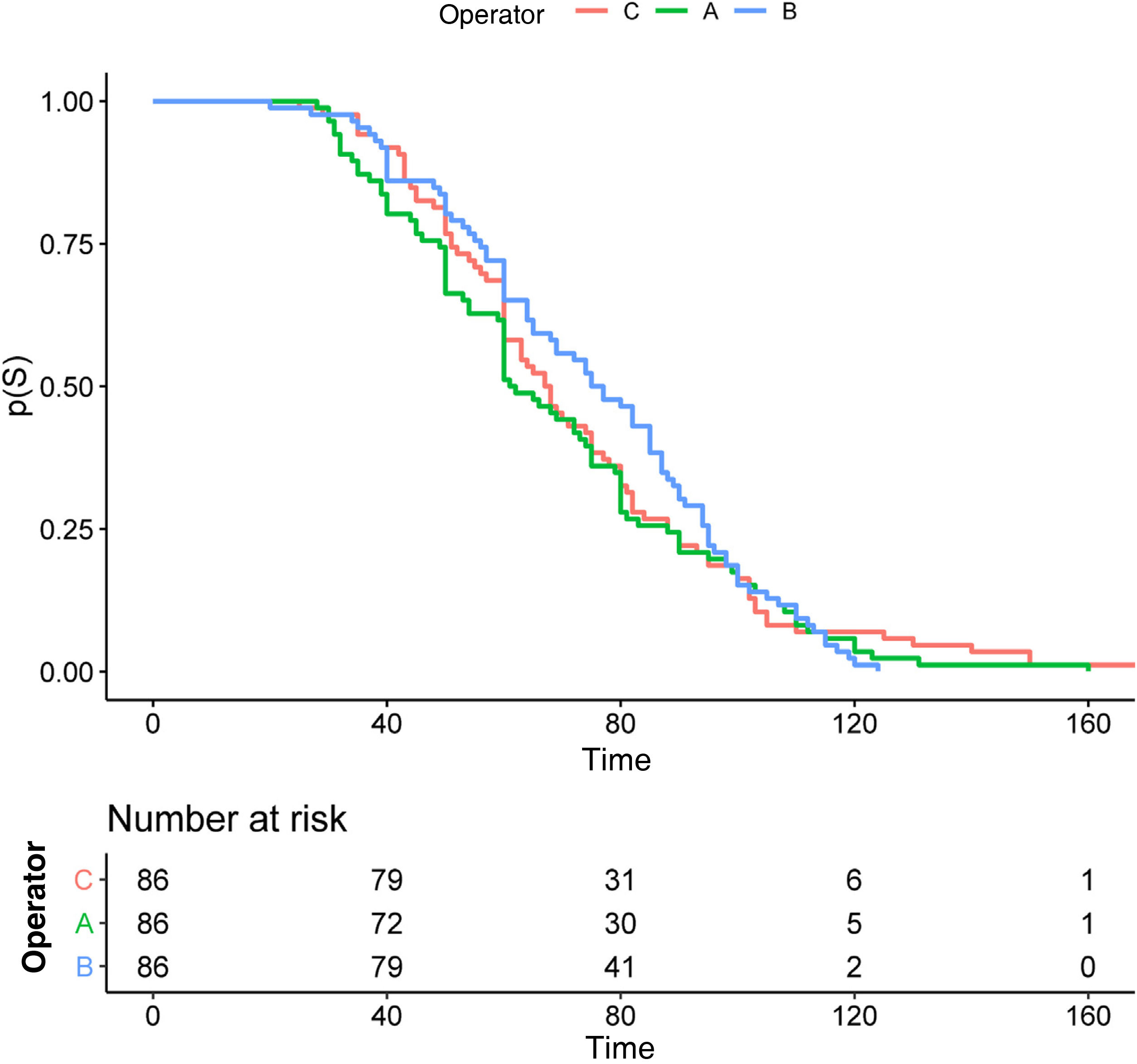
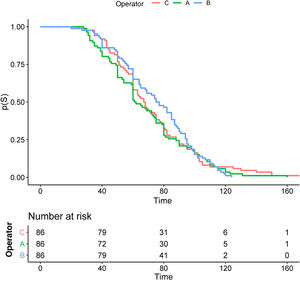
Fig. 2 shows the Kaplan Meier analysis illustrating the relationship between procedure time and the assessability of each patient, between the 3 operators. There is no difference in decision time according to the observer (p = .60). The mean procedure time is around 70 s with no major differences between surgeons.
DiscussionPreoperative assessment of VCs is an essential requirement for good planning of thyroid surgery. CU is an increasingly developed procedure and can be performed by surgeons as a bedside technique.
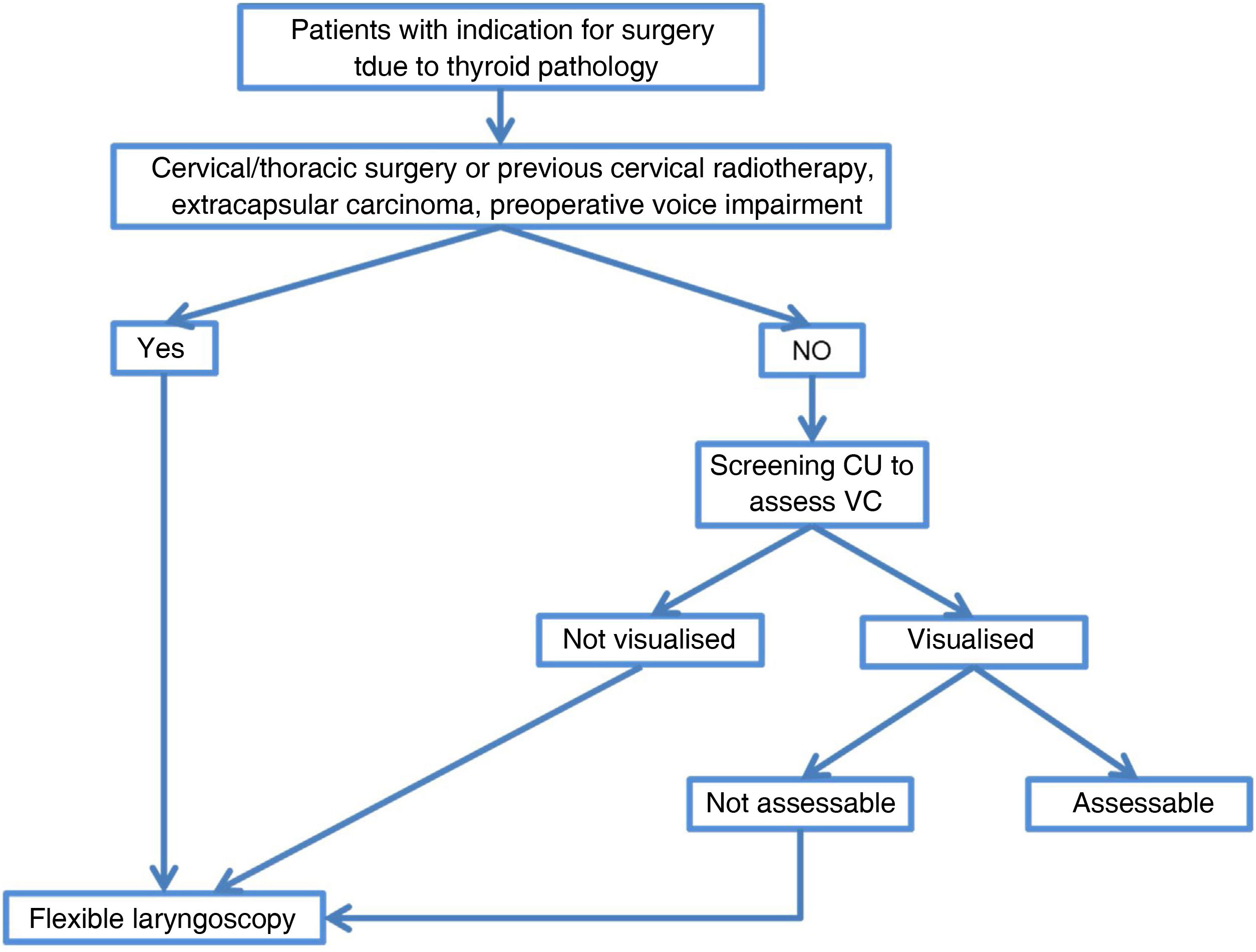
VC paralysis, although a relatively rare complication,5 is associated with increased morbidity affecting patients' quality of life (voice, swallowing and airway). This, in turn, has serious medico-legal implications and high costs for healthcare systems.9 Therefore, preoperative VC assessment is necessary, especially in certain scenarios such as patients with voice abnormalities, history of thoracic or cervical surgery, known thyroid cancer or suspected/confirmed lesion of the RLN or vagus nerve.10,11 Although FL is currently the gold-standard technique in the evaluation of these structures, especially indicated in these scenarios, CU has been developed as a preoperative screening method that can be implemented in all other cases, being a less invasive technique and fundamentally more accessible to the endocrine surgeon in our environment. For this reason, authors such as Wong6 have defended this technique with good results.
The appropriate study of VCs by CU is determined by certain intrinsic characteristics of the patients. Gender and age must be considered, as they are variables of particular relevance in the population in question, since thyroid disease is more prevalent among younger women.12,13 The presence of a more protruding thyroid cartilage in males hinders the assessment of VCs.14,15 In fact, a more obtuse angulation of the anterior ala of the thyroid was associated with a better quality of laryngeal examination.16 This was also evident in our study, where males were associated with a higher probability of non-assessment (incidence ratio of 2.12). In terms of age, the increased ossification of the thyroid cartilage with age hinders the passage of the ultrasound beam and, therefore, the images are poorer.15,17 It has also been observed in our analysis that older individuals have a poorer assessment compared to younger subjects. In this regard, patients over 60 years of age have a high risk of non-assessment in our study (incidence ratio of 2.37).
Excess body weight is a controversial feature due to its negative impact on ultrasound imaging. While Kandil et al.18 oppose ultrasound as a substitute for FL, especially in populations with higher BMI, others such as Carneiro-Pla et al.7 support its use regardless of weight/height ratio. In our study, 52% of the individuals examined were overweight or obese, despite which BMI was not associated with an increased risk of non-assessment, as previously reported in other published series. 13,14 Although we did not measure neck diameter or the distance between the skin and the thyroid cartilage in our study, these factors should be taken into account in future studies.
The duration of the technique is another relevant factor when implementing this technique. Considering that it is a procedure that can be performed at the bedside, and also considering the high number of patients seen in our healthcare system, CU should not cause delays in the surgical consultation. According to Wong19 the average time required for an experienced operator to perform the technique is 30 s. On the other hand, Masood et al.16 have shown that the mean time for CU in expert hands is 1.8 min. In our study 70 s was the mean time between the 3 operators, with no difference between them (p = .60). Furthermore, most of the examinations were completed in less than 2 min, as shown in Fig. 2. In our opinion the timing of the procedure was relevant, as a prolonged test time was associated with greater hesitancy in the assessment of VCs, and thus a higher degree of non-assessable scans.
Preoperative ultrasound analysis of VCs has recently been investigated by many authors. The high rate of VC assessment by CU would avoid invasive procedures and serves as a screening procedure prior to a more aggressive technique. FL, although the gold standard in laryngeal assessment, could be reserved for selected cases in which CU cannot assess VC status (e.g., males or elderly population), remaining as a second-level examination, or in cases at high risk of VC paralysis (extracapsular thyroid carcinoma, large thyroid goitre, patients with voice changes and previous cervical surgery),20 as reflected in the algorithm in Fig. 3. Therefore, preoperative assessment of VCs with a screening technique such as CU, coupled with the routine use of intraoperative neuromonitoring, would decrease the risk of overlooking VC palsy.
Our work has several limitations. Firstly, it is a non-comparative study. The lack of a control group using FL, the reference technique in the evaluation of VCs, is the main limitation. Moreover, the operators are not experts in CU, despite having been trained with at least 100 cases of cervical ultrasound. Even so, the learning curve described in other articles, as well as the peculiarities of the technique itself (operator dependent) contribute to a certain degree of heterogeneity in the results.7,19 Finally, the selection of patients with no known previous VC palsy is another limitation, even if this information was withheld from the evaluators. Studies of “normal” anatomy usually exclude patients undergoing radiotherapy or with previous cervical surgery, so the results cannot be fully extrapolated to the main population at hand.
In conclusion, CU is an easy technique to implement in an endocrine surgery unit when performed by the surgeons themselves, allowing the evaluation of VCs, especially in young women. The possibility of being an examination performed by endocrine surgeons at the bedside, without relying on techniques performed by external services, and the fact that it is a non-invasive procedure, makes CU a good tool for VC screening in the preoperative evaluation of patients who are candidates for thyroid surgery and in the planning of the surgical intervention.
AuthorshipL. E. Pérez-Sánchez, E. Caballero-Rodríguez, J.C. Jordán-Balanza: planning, study design and data collection.
L. E. Pérez-Sánchez y R. Orti-Rodríguez: writing of the manuscript.
A. Soto-Sánchez y M.A. García-Bello: analysis and interpretatio of results. All authors: critical review, reading and final approval of the manuscript.
Conflict of interestsThe authors have no conflict of interests to declare.