Radiofrequency ablation of liver metastases is an alternative to surgical resection when the use of this technique is not possible. It is generally a safe technique that provides good results in the treatment of lesions smaller than 3cm.1 One of its limitations is its reduced effectiveness when these lesions are close to blood vessels due to the cooling effect that it causes in blood circulation. For this reason, when it is applied intraoperatively, hilar clamping is recommended to reduce this effect. In the case we present, radiofrequency ablation of a central metastasis with hilar clamping led to complete ischemic necrosis of a liver segment.
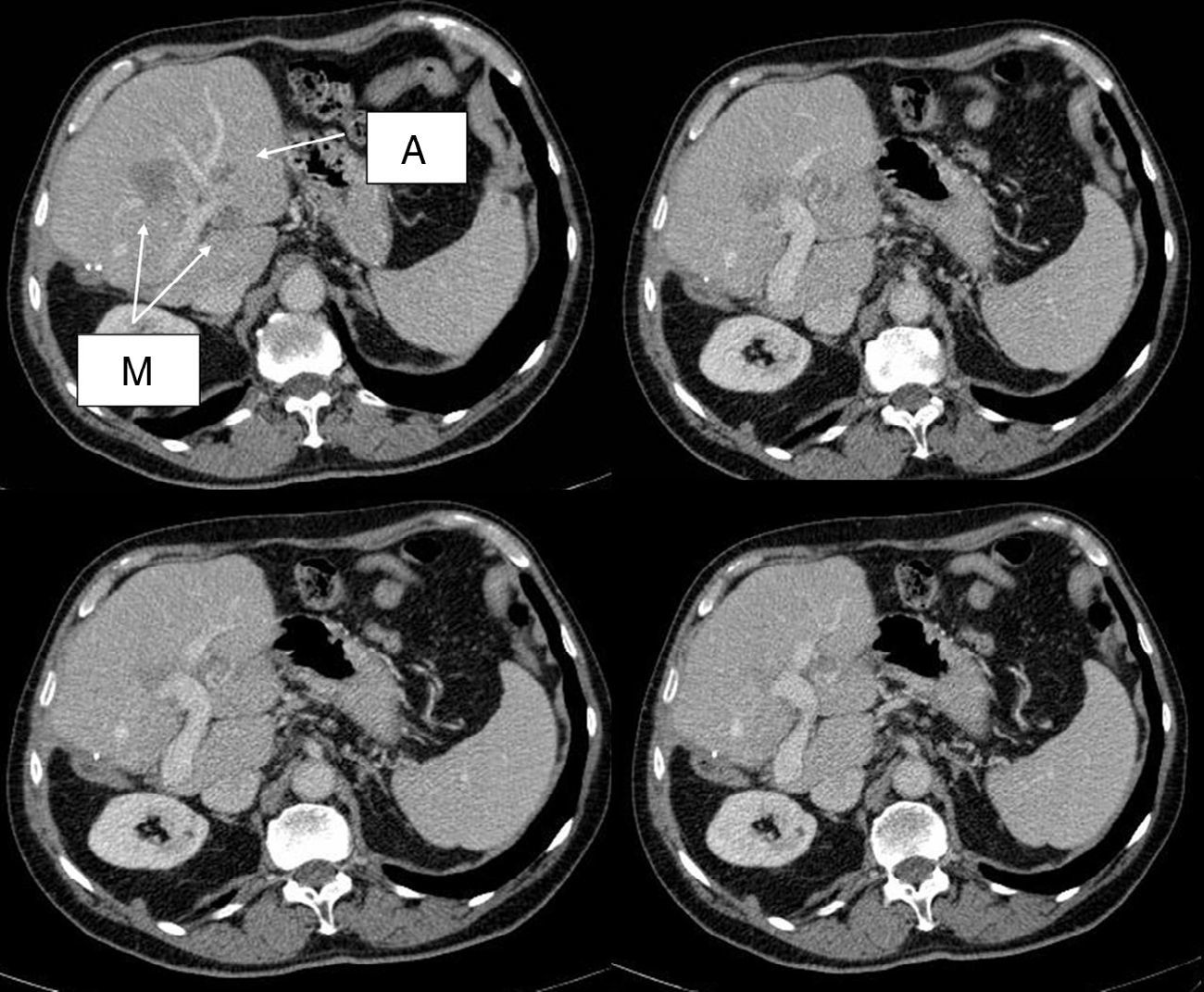
The patient is a 72-year-old male with a history of colon cancer and synchronous liver metastases that had been resected by means of right hepatectomy 14 months earlier. During follow-up, 3 new metastases were detected: 2 superficial lesions in segment II, and 1 deep lesion measuring 2cm in segment IV, which was in contact with the left portal vein and encompassed branches of this segment (Fig. 1). The location made surgical resection impossible. We considered the possibility of R0 treatment using combined surgery and radiofrequency ablation. In a multidisciplinary clinical session, treatment with 4 cycles of neoadjuvant FOLFIRI-cetuximab was decided. Re-evaluation with CT and MRI showed a partial response with no extrahepatic metastases.
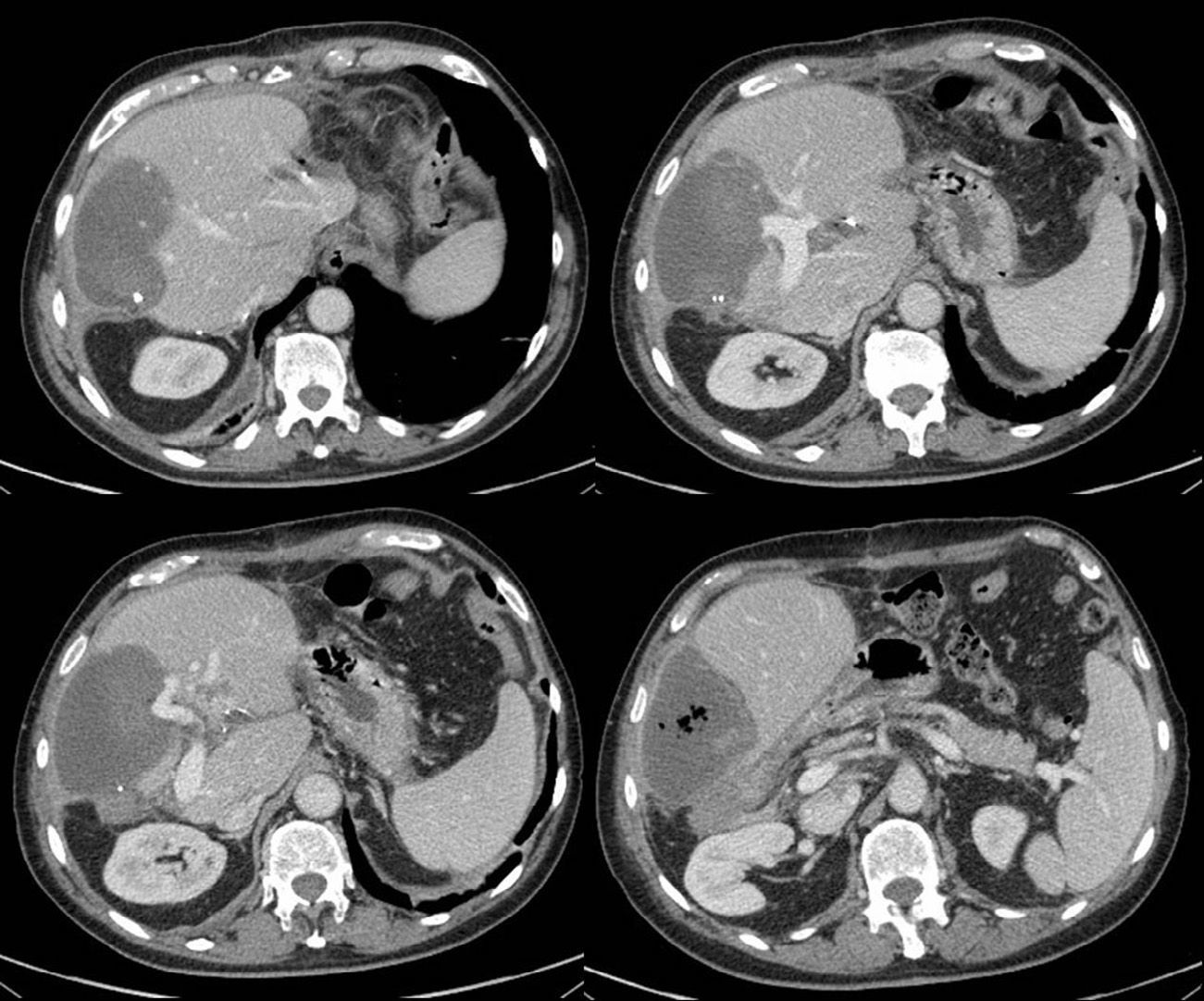
The patient underwent surgery, involving individual non-anatomical resections of the metastases in segment II and radiofrequency ablation of the metastasis in segment IV. We used the Cool-tip™ RF Ablation System by Covidien with a needle whose radius of action was 3cm, and radiofrequency was applied with hilar clamping for 11min. The postoperative period was uneventful; transaminase levels were initially elevated (GOT/GPT=1505/1373IU/L; GGT/FA=241/128IU/L), then progressively descended, and liver function was normal. The patient was asymptomatic and discharged on the 7th day post-op. On the 12th day post-op, the patient was readmitted with fever. Lab workup showed normal liver function (GOT/GPT=59/161IU/L and GGT/FA=1213/726IU/L) and normal bilirubin. CT detected a collection that occupied the entire segment IV, with dense content and air bubbles and no arterial or venous contrast material (Fig. 2). Needle aspiration obtained a small amount of serosanguineous fluid that was sent for culture, which ruled out the presence of biliary content. Both this culture and the blood cultures were negative. The clinical-radiological diagnosis was complete ischemic necrosis of segment IV. The patient was treated with empirical antibiotics and antipyretics, after which he presented good clinical progress. The patient was discharged after 6 days with oral antibiotic therapy (the patient's residence was in another province, which made early discharge difficult). In spite of the complication described, the treatment was effective and there was no evidence of disease 6 months afterwards.
Although radiofrequency ablation of liver metastases is a rather safe procedure, it does have its complications. These are more frequent when the procedure is percutaneous than when the application is intraoperative due to the greater control of the pathway of the needle and the neighboring organs in this latter situation. For this reason, we prefer its intraoperative application, which also enables hilar clamping in order to improve its efficacy. Reported complications of radiofrequency include abscesses, bilomas, biliary fistulas, sepsis, portal thrombosis, etc.2 We have not found any published cases with ischemic necrosis of an entire segment. Portal thrombosis is more frequent in cirrhotic patients and it has been associated with procedures with vascular occlusion and a distance of less than 5mm to the vessel.3,4 The cause of the thrombosis is the heat-generated endothelial damage.2 Nonetheless, in a recent study, hilar clamping was not associated with a greater incidence of major complications,5 and its application in metastases close to hepatic veins with hilar and corresponding hepatic vein clamping was also safe.6 In cases with portal thrombosis, although it may cause liver failure, it does not lead to ischemic necrosis of the parenchyma as it is substituted by the corresponding hepatic artery.7
In our case, in addition to portal thrombosis, there must have been arterial thrombosis of the branch from segment IV that led to complete ischemic necrosis of the segment. In our patient, the liver parenchyma of segments I, II, and III was sufficient to maintain normal liver function. Nevertheless, the consequences could have been severe, so this complication, although uncommon, should be considered in similar cases and other ablative techniques should be contemplated.
Please cite this article as: Alonso Casado Ó, González Moreno S, Encinas García S, Rubio González E, Ortega Pérez G. Necrosis isquémica completa del segmento IV tras ablación con radiofrecuencia con clampaje hiliar. Cir Esp. 2015;93:467–469.