Eosinophilic cholecystitis (EC) was described for the first time in 1949 by Albot.1 Its etiology is not always well defined, and can be due to allergies, parasitosis, hypereosinophilic syndrome, eosinophilic gastroenteritis, eosinophilia-myalgia syndrome and drugs.2,3 Peripheral eosinophilia is not present in the majority of cases and the diagnosis is established by the presence of infiltrate in the gallbladder wall with more than 90% eosinophils,4 because clinically it presents with the classic symptoms of acute cholecystitis. Treatment is cholecystectomy and the diagnosis is confirmed by the pathology study.
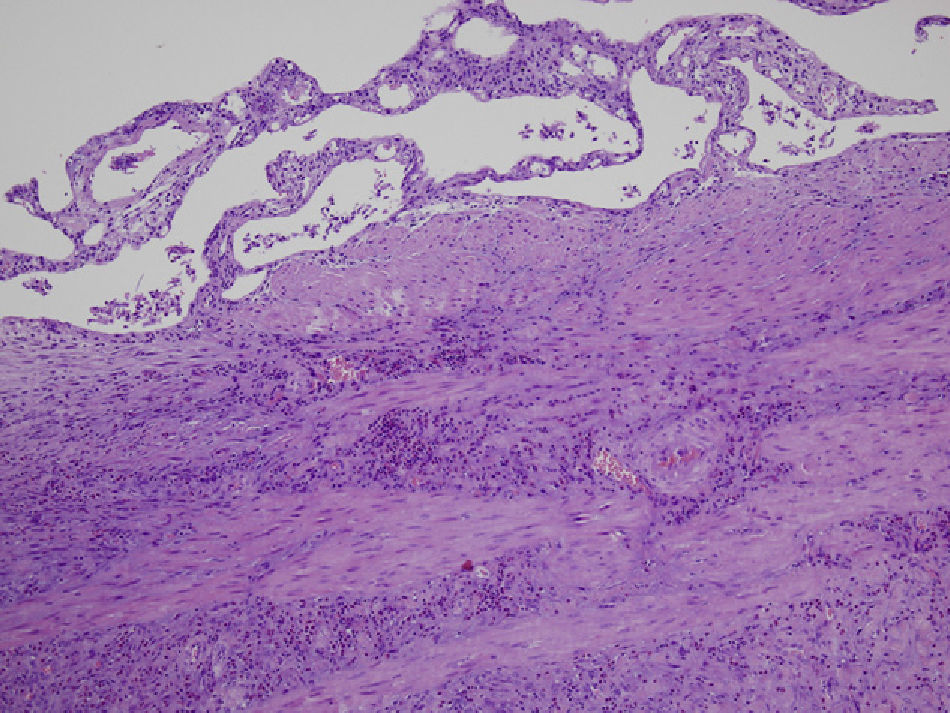
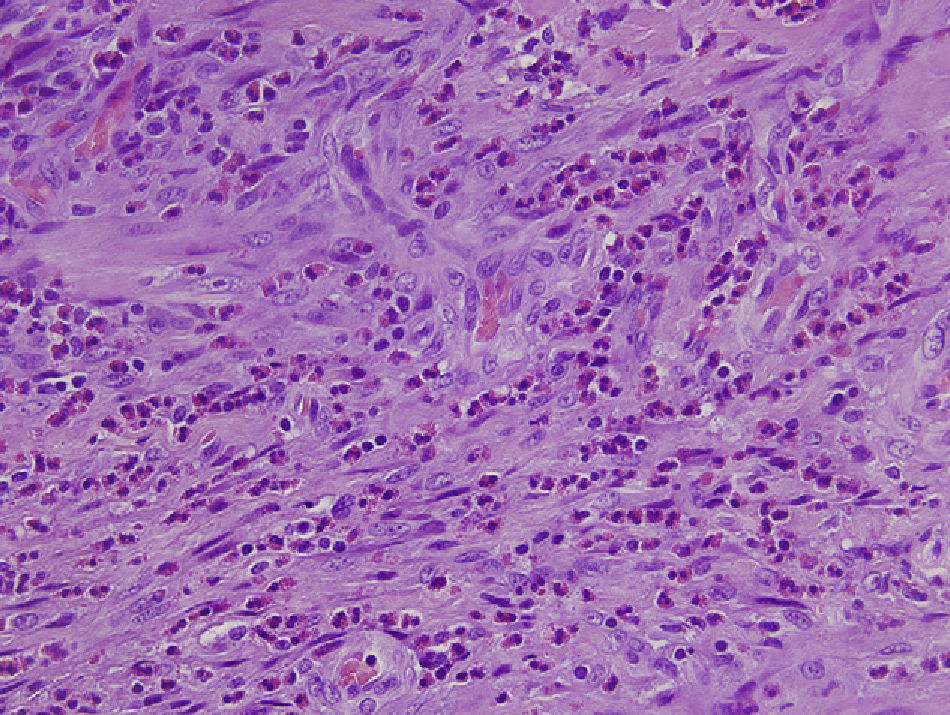
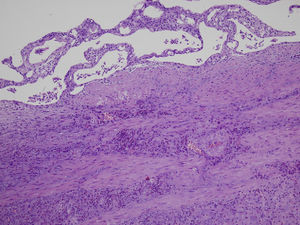
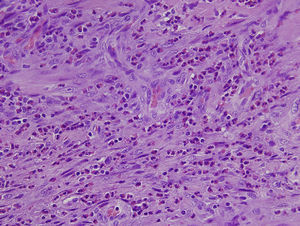
We present a case of EC that was treated with laparoscopic cholecystectomy. The patient is a 65-year-old male with a history of type 2 diabetes mellitus in treatment with oral antidiabetes medication, nephrolithiasis and lumbar arthrodesis, with no history of allergy to any medication. He came to our Emergency Room complaining of epigastric abdominal and right upper quadrant pain during the previous 48h, with no other symptoms. On examination, palpation was painful in the right upper quadrant, with a positive Murphy's sign. Blood tests showed a leukocyte count of 10,500 leukocytes/mm,3 70.5% segmented and 3.6% eosinophils (normal reference values, 0%–5%). Total serum bilirubin was 1.3mg/dl; liver enzymes were moderately elevated (AST: 503U/l, ALT: 239U/l, GGT: 818U/l, AP: 402U/l). Abdominal ultrasound showed findings compatible with acute cholecystitis and a normal main bile duct, and emergency cholecystectomy was decided upon. This was performed laparoscopically with no complications. The pathology study revealed diffuse inflammation of the gallbladder wall with tissue eosinophilia >90% and absence of calculi (Figs. 1 and 2). The patient had a favorable postoperative course and was discharged from the hospital 48h after surgery.
EC is a rare entity described by Albot in 1949,1 and there are only 30 cases published in the scientific literature2–4; it generally presents in the absence of gallbladder lithiasis.5 When it presents as acute cholecystitis, it is difficult to suspect the diagnosis before the histologic study of the specimen, unless there is peripheral eosinophilia. CE can present in patients with hypersensitivity or allergy to medication (such as penicillin or erythromycin3), eosinophilia-myalgia syndrome, immunosuppression, parasitosis by Echinococcus, Clonorchis sinensis or Ascaris lumbricoides,4 gastrointestinal eosinophilic infiltration (eosinophilic gastroenteritis, eosinophilic granulomatous hepatitis or eosinophilic ascites),5 infections due to cytomegalovirus or cryptosporidium, Crohn's disease, sarcoidosis, lupus erythematosus, polyarteritis nodosa, Sjögren's syndrome6–9 or the ingestion of medicinal herbs.10
Without any of these precipitating causes, idiopathic EC should be considered, as in the case that we report. The clinical presentation is equal to acute cholecystitis and the diagnosis is based on the presence of an eosinophilic infiltrate >90% in the histologic study of the gallbladder.6,8 In most patients, the clinical evolution is benign and the symptoms resolve with cholecystectomy, which can generally be laparoscopic. In cases with associated symptoms of eosinophilic gastroenteritis or eosinophilic cholangitis, corticosteroids may be necessary to complete the treatment.2,3
In summary, EC is a pathology that should be kept in mind because, when it is associated with peripheral eosinophilia, there is a large number of clinical situations in which there may be eosinophilic infiltration of other organs. In addition, we should rule out these causes in order to be able to define idiopathic EC, as in the case that we report.
Please cite this article as: Fernández Santiago R, Fontanillas Garmilla N, Gutiérrez Fernández G, Fernández Fernández F, Gómez Fleitas M. Colecistitis eosinofílica. Cir Esp. 2013;91:465–466.