Budd–Chiari syndrome (BCS) is a heterogeneous group of diseases characterized by obstruction of the hepatic venous outflow at the suprahepatic veins (SHV) or the inferior vena cava (IVC). This obstruction results in increased hepatic sinusoidal pressure and portal hypertension, which can lead to cirrhosis of the liver if left untreated.1 The most frequent causes of BCS in our setting are hematological alterations,2 and complete membranous obstruction of the IVC is rare.3,4 The relationship between BCS and increased risk of hepatocellular carcinoma (HCC) has not been well established.2
We report the case of a 34-year-old female patient who was diagnosed with chronic liver disease at another hospital in 2008 following the intraoperative finding of ascites during a cesarean section. Since 2009, the patient has been followed-up at our hospital and diagnosed with chronic BCS due to idiopathic thrombosis of the SHV, after having ruled out hematological causes.
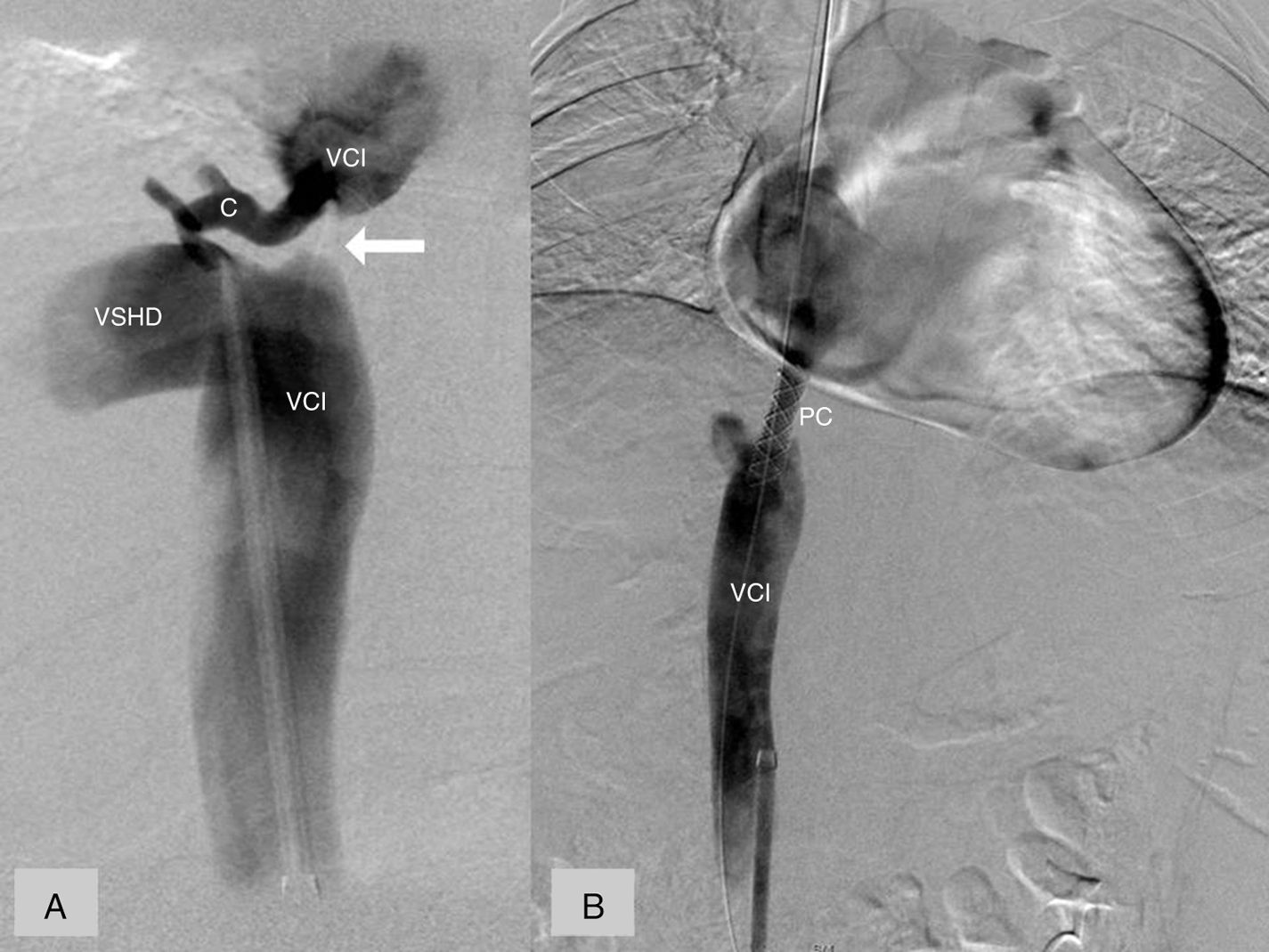
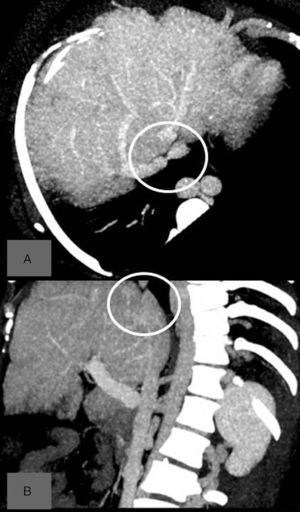
A follow-up abdominal ultrasound in 2015 demonstrated an image compatible with HCC in liver segment VI measuring 2.7cm, which was confirmed by abdominal CT (Fig. 1A). In this situation of a patient with HCC and signs of portal hypertension (thrombocytopenia and history of ascites), liver transplantation was proposed.5 However, abdominal CT scan revealed that the right and left SHV were permeable, the median vein was occluded, and there was stenosis of the upper part of the IVC with formation of collateral circulation at the level of the azygos and lumbar veins (Fig. 1B). As the cause was therefore potentially treatable, we decided to perform a cavography with therapeutic intent. The cavography reported an obstruction of the IVC above the outlet of a dilated right suprahepatic vein, with a collateral vein near the occlusion point that connected with the IVC above the stenosis (Fig. 2). As it was impossible to move the guidewire through the occlusion, we decided to connect the segments above and below the stenosis by means of direct puncture and placement of a coated stent (Wallgraft® 8mm in diameter and 30mm in length). The confirmation cavography showed correct contrast passage through the prosthesis with a significant reduction of the collateral circulation to the azygos system (Fig. 2B). During the postoperative follow-up, the patient had no ascites and her platelet count normalized. At this time, as we were faced with a patient with chronic liver disease, who, if she had developed cirrhosis, would be classified as Child–Pugh A, with no signs of portal hypertension, we considered that liver resection was indicated.
The patient underwent surgery in January 2016, including limited resection of the lesion in segment VI. The postoperative period was free of incidents. The pathology study reported the presence of a 2.8cm HCC with free resection margins, no factors for a poor prognosis and hepatic parenchyma with cirrhosis.
BCS secondary to complete membranous obstruction of the IVC is a common disease in Africa and Asia, and several authors have proposed distinguishing it from classic BCS because of its differences in pathophysiology and progression.6,7 This entity usually presents a chronic course with few symptoms, so the diagnosis is generally made in advanced stages of the disease,3,4,6 with an incidence of liver cirrhosis in up to 70%.6 Percutaneous revascularization is the treatment of choice8 and is based on cavography, direct puncture of the membrane to circumvent the IVC stenosis, and stent placement.7,9 Surgery with placement of a graft between the pre-stenosis IVC and the right atrium3 has also been described for cases that cannot be resolved percutaneously. The results of stent placement in IVC obstruction are excellent; Zhang et al.10 report initial success of the treatment in 94% of patients, with clinical improvement in all of them, and in 96.7% the stents remained permeable at the end of follow-up.
A recent review by Ren et al.4 reports a prevalence of HCC in patients with BCS of 17.6% and up to 26.5% in patients with IVC obstruction. The increased risk for developing HCC in patients with obstruction of the IVC has been attributed to the fact that these individuals present a long-term process with few symptoms, which enables fibrosis to slowly develop in the liver, finally leading to cirrhosis.6,7 In contrast, in Western countries, where the majority of Budd–Chiari cases are secondary to hematological alterations and the progression of the disease tends to be acute or sub-acute, the association between BCS and cirrhosis of the liver or HCC is rare.2
In conclusion, membranous obstruction of the IVC is a disease with a low prevalence in Western countries which, given its chronic nature, is a frequent cause of cirrhosis. The case we describe demonstrates the possible treatment of the occlusion, which can modify the clinical situation and influence the treatment of any possible HCC.
Please cite this article as: Mils K, Lladó L, Ramos E, Domínguez J, Baliellas C. Carcinoma hepatocelular en paciente con síndrome de Budd-Chiari por membrana en la vena cava inferior. Posibilidad de resección tras tratamiento angio-radiológico del síndrome de Budd-Chiari. Cir Esp. 2017;95:47–49.