Recently a score (LARS) has been internationally validated that quantifies the anterior resection syndrome (ARS). The objective of this study is to know the incidence and severity of the ARS using LARS and its correlation with selected variables or risk factors.
MethodsAll operated patients with anterior resection for rectal cancer between October 2007 and February 2014, with curative intention and at least one year of functionality, were sent a LARS questionnaire. The variables studied were age sex, time elapsed since surgery, type of surgical approach, type of anastomosis, derivative ileostomy, postoperative pelvic complication, and radiotherapy regimen.
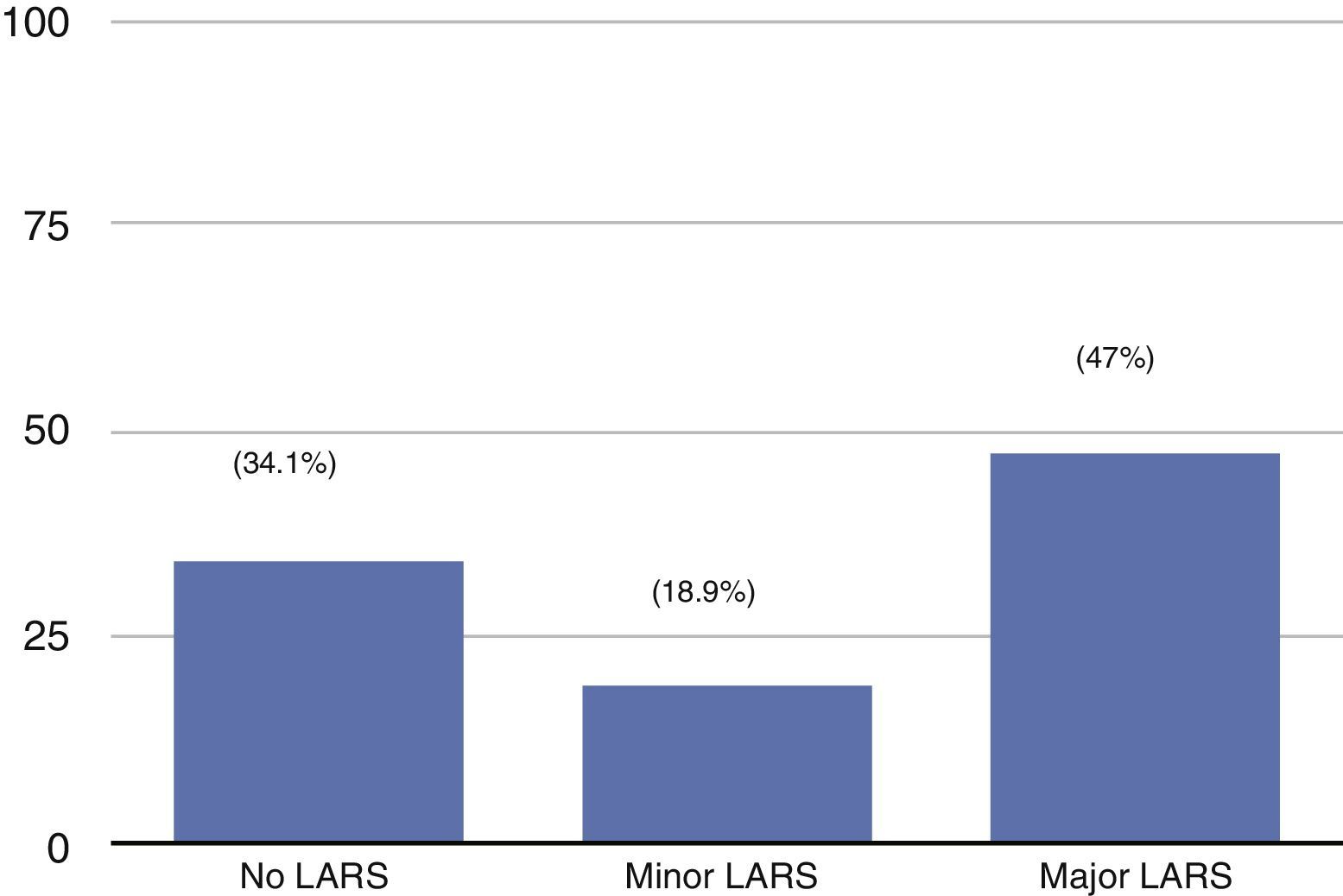
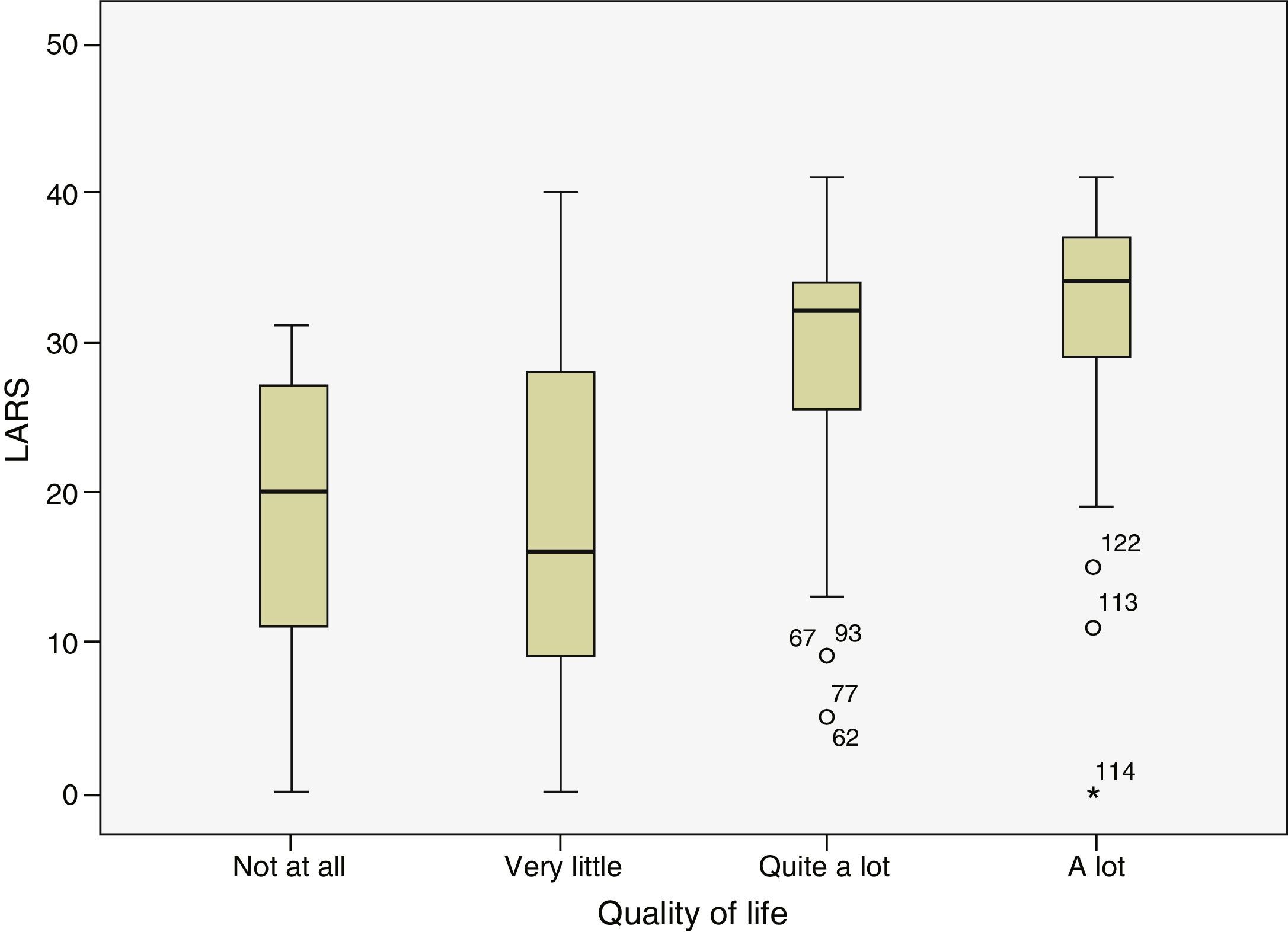
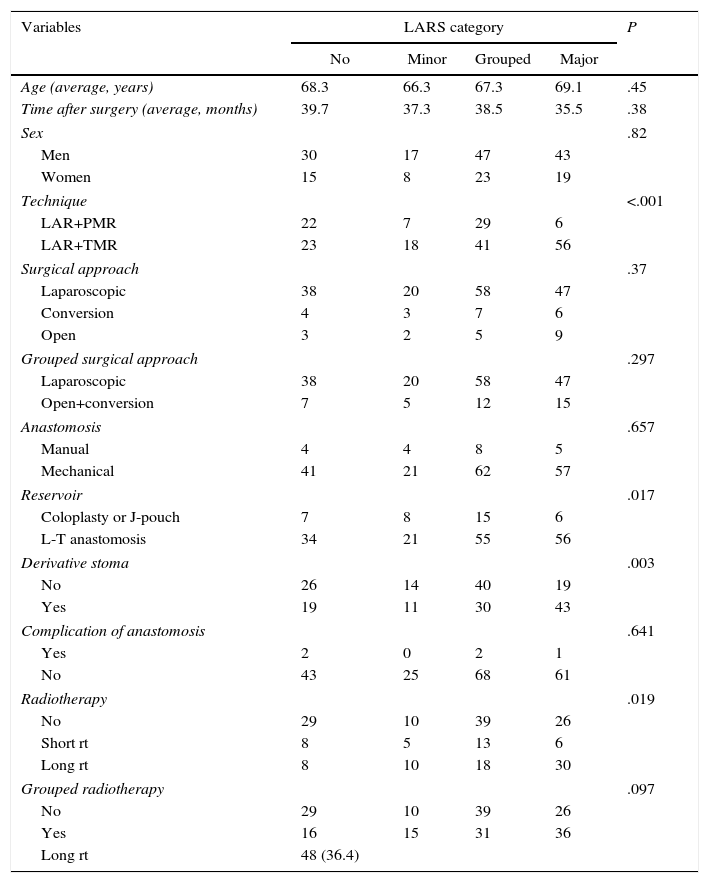
ResultsOut of 195 patients, 136 (70%) responded, and 132 responded properly. A total of 47% of the patients presented “severe” LARS and 34% did not develop quantifiable ARS. Quality of life was worse in the highest LARS scores (P=.002). In the univariate analysis, total mesorectal excision, long radiotherapy regimen and derivative stoma were associated to “severe” LARS and the use of a reservoir was associated with minor LARS. In multivariate analysis only the type of resection (P<.001) and the use of a reservoir (P=.002) were individual factors related to LARS.
ConclusionsHalf of the operated patients presented high LARS score and only a third did not provide a quantifiable ARS. The overall perception of quality of life was significantly worse in patients with more severe LARS. The absence of the rectum (total mesorectal excision) and the type of anastomosis were the main factors associated with the LARS score.
Recientemente se ha validado una escala internacional de puntuación (LARS) que cuantifica el síndrome de resección anterior (SRA). El objetivo de este estudio es conocer la incidencia y gravedad del SRA utilizando el LARS y su relación con variables seleccionadas.
MétodosA todos los pacientes con resección anterior por cáncer de recto operados entre octubre de 2007 y febrero de 2014, con intención curativa y con más de un año de funcionalidad, se les envió el cuestionario LARS. Las variables estudiadas fueron: edad, sexo, tiempo transcurrido desde la cirugía, tipo de resección, vía quirúrgica, tipo de anastomosis, realización de estoma derivativo, complicación postoperatoria y régimen de radioterapia.
ResultadosDe 195 pacientes, 136 (70%) respondieron (132 adecuadamente). El 47% de los pacientes presentaba un LARS mayor y el 34% no desarrolló SRA cuantificable. Se relacionó un LARS mayor con peor calidad de vida (p=0,002). En el análisis univariante, la escisión mesorrectal total (ETM), la radioterapia larga y el estoma derivativo se asociaron a un LARS mayor, y la utilización de un reservorio, a uno menor. En el análisis multivariante solo el tipo de resección (p<0,001) y la utilización de reservorio (p=0,002) fueron factores individuales relacionados con el LARS.
ConclusionesLa mitad de los pacientes operados presentaron un LARS mayor y solo un tercio no presentó un SRA cuantificable. La percepción global de la calidad de vida fue significativamente peor en los pacientes con LARS mayor. La ausencia de recto (ETM) y la forma de reconstrucción anastomótica fueron los principales factores asociados a la puntuación LARS.
In the last 3 decades advances in rectal cancer treatment have achieved a reduction in the locoregional recurrence rate. Additionally, they have made it possible to centre the therapeutic objective on the preservation of the sphincter function (and even the organ itself) while maintaining overall survival and disease-free rates. These largely and finally depend on the current or future existence of systemic disease. Anterior resection of the rectum while preserving intestinal continuity using various types of colorectal or colo-anal anastomosis, with or without combined radiochemotherapy, is today the most frequent treatment for cancer of the rectum.
Most of the patients operated with preservation of the sphincter will develop an alteration of intestinal and defecatory functions. The dysfunction varies in its symptoms and severity, and it manifests as urgency, incontinence and fragmented defecation, with bowel movements that are repeated, incomplete or difficult. The set of these symptoms constitutes what is known as the anterior resection syndrome (ARS), which may have a negative effect on the lives of operated patients. It is at present one of the main topics for clinical research.1
Due to the heterogeneous nature of the physiopathological, clinical and therapeutic aspects in connection with ARS, evaluation of the same has been predominantly descriptive and not quantitative, using unvalidated questionnaires. This has prevented comparative analyses of the functional results of different therapeutic approaches.2 Recently an international scoring system, the “LARS scale”, has been prepared, translated and validated in several languages. This makes it possible to quantify the severity of intestinal and defecatory dysfunction in a simple way, facilitating comparison and meta-analysis of different aspects of treatment.3 This scoring system has also been correlated with quality of life in an international study by applying the EORTC QLQ-C30 questionnaire for patients operated for cancer, and a relationship between quality of life and patients’ LARS has been observed.4
The objective of this study is to study the incidence, distribution and severity of ARS among our rectal cancer patients treated by anterior resection using the LARS score. It aims to confirm its quantitative correlation with the risk factors (clinical, therapeutic or pathological) which are known to be connected with ARS.
MethodsAll of the patients treated in our hospital for rectal cancer with a curative purpose by anterior resection of the rectum from October 2007 to February 2014 were included in this study. Patient data recorded in the hospital rectal cancer record were used prospectively and consecutively. In turn these were included (and are available) in the national record of Proyecto Vikingo.5
Patients with intersphincteric or associated multivisceral resection were excluded, as were those who had not had a reconstructed transit for at least one year. One year was taken to mean one year after the operation if they did not have a derivative stoma, or one year after the closure of the stoma. No age restrictions were applied.
All of the patients were sent a letter by ordinary mail which contained, together with the request to take part in the study, an informative note describing its aim and a declaration of its confidentiality. It also contained the LARS scale questionnaire in Spanish and a question that had been used in previous LARS validation studies about their opinion of how their intestinal and defecatory symptoms affected their overall quality of daily life. The patients who failed to answer the questionnaire appropriately were excluded.
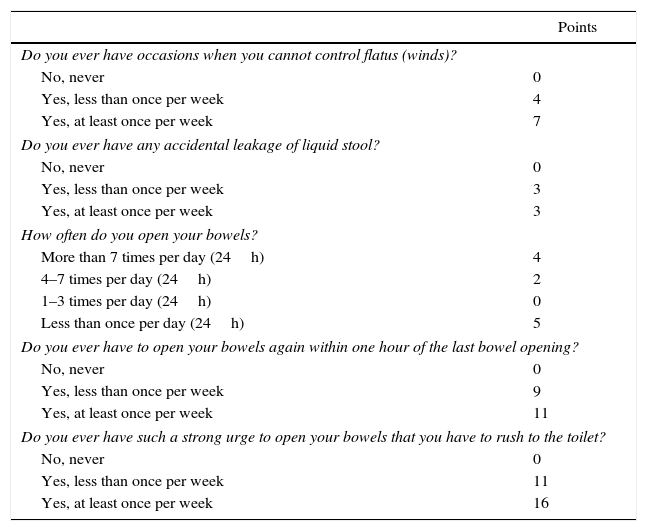
Table 1 shows the LARS questionnaire, which is composed of 5 questions that centre on the symptoms experienced by patients; the sum of all the items varies from 0 to 42 points, for classification into 3 groups: non-LARS (0–20 points), minor LARS (21–29 points) and major LARS (30–42 points). The question about quality of life was “In general, how much does the functioning of your intestines affect your quality of life?” There were 4 possible options: “not at all”, “very little” “quite a lot” or “a lot”. The variables selected to study possible risk factors for ARS and its correlation with the LARS were age, sex, length of time after surgery (or after closure of the protective stoma), the type of resection performed (high or low), the extent of the mesorectal resection (total or partial), the surgical approach used (open, laparoscopic or converted), type of anastomosis (colorectal or colo-anal; manual or mechanical), the use of a colonic reservoir or transverse coloplasty or not (lateroterminal or terminoterminal anastomosis), the creation of a derivative stoma (yes or no), postoperative complication of the anastomosis (dehiscence or abscess, yes or no) and the radiotherapy regime (no radiotherapy, short or long).
LARS Questionnaire in Spanish.
| Points | |
|---|---|
| Do you ever have occasions when you cannot control flatus (winds)? | |
| No, never | 0 |
| Yes, less than once per week | 4 |
| Yes, at least once per week | 7 |
| Do you ever have any accidental leakage of liquid stool? | |
| No, never | 0 |
| Yes, less than once per week | 3 |
| Yes, at least once per week | 3 |
| How often do you open your bowels? | |
| More than 7 times per day (24h) | 4 |
| 4–7 times per day (24h) | 2 |
| 1–3 times per day (24h) | 0 |
| Less than once per day (24h) | 5 |
| Do you ever have to open your bowels again within one hour of the last bowel opening? | |
| No, never | 0 |
| Yes, less than once per week | 9 |
| Yes, at least once per week | 11 |
| Do you ever have such a strong urge to open your bowels that you have to rush to the toilet? | |
| No, never | 0 |
| Yes, less than once per week | 11 |
| Yes, at least once per week | 16 |
0–20: no LARS; 21–29: Minor LARS; 30–42: Major LARS.
All of the patients had been evaluated by the Multidisciplinary Colorectal Cancer Committee. High resolution NMR was used to stage the cancer before operating and to evaluate mesorectal involvement and the height, length and lower edge of the tumour. In general, total mesorectal resection was used for cancer of the mid to low rectum, while partial mesorectal resection was used for upper rectal cancer. When this was considered to be indicated, and following discussion in the Multidisciplinary Committee, 2 neoadjuvant treatment regimes were used. These consisted of long chemoradiotherapy (54Gy in 5 weeks with chemotherapy at the start and end of radiotherapy) or short radiotherapy (25Gy over 5 days). The anastomosis was only examined using imaging techniques if there was the clinical suspicion of a complication.
Statistical AnalysisThe results were analysed in the Clinical Epidemiological Department of the hospital using the STATA program (StataCorp. 2013. StataStatistical Software: Release 13. College Station, TX: StataCorp LP).
Data are described in terms of absolute and relative frequencies in percentages and averages with standard deviation for continual variables, or the median and interquartile range if the data distribution made this advisable.
Firstly possible risk factors with the LARS category were analysed in univariate analysis. This had the purpose of identifying statistically significant variables using the Student t-test (Mann–Whitney U test) or Pearson's χ2 (Fisher's test). Multivariate logistical regression test analysis was then used to identify significant risk factors (P<.05) independently associated with a major LARS.
The Student t-test (and the Mann–Whitney U test) were used to study the correlation between the LARS and quality of life, after grouping the categories “not at all” and “very little” on the one hand, and “quite a lot” and “a lot” on the other, to increase the power of the study.
Results402 patients were operated on for cancer of the rectum from October 2007 to February 2014 in our hospital. Of these, 260 (65%) had an anterior resection of the rectum. 65 patients were excluded because they still had an unclosed ileostomy or because less than one year had passed since their surgery at the time of carrying out the survey. 195 patients were contacted by ordinary mail. A total of 136 patients (70%) answered the questionnaire, 132 of whom did so appropriately. 4 questionnaires were invalidated due to formal defects, as several answers had been selected simultaneously. The study sample was therefore composed of these 132 patients.
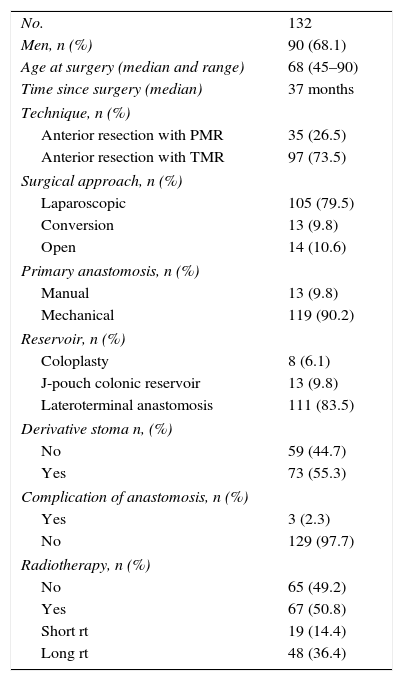
The median patient age was 68 years old, with a range from 45 to 90 years old. The median time which had passed from surgery to the survey was 37 months. Table 2 shows the demographic, clinical and therapeutic characteristics of the patients studied.
The Demographic, Clinical and Therapeutic Characteristics of the Patients.
| No. | 132 |
| Men, n (%) | 90 (68.1) |
| Age at surgery (median and range) | 68 (45–90) |
| Time since surgery (median) | 37 months |
| Technique, n (%) | |
| Anterior resection with PMR | 35 (26.5) |
| Anterior resection with TMR | 97 (73.5) |
| Surgical approach, n (%) | |
| Laparoscopic | 105 (79.5) |
| Conversion | 13 (9.8) |
| Open | 14 (10.6) |
| Primary anastomosis, n (%) | |
| Manual | 13 (9.8) |
| Mechanical | 119 (90.2) |
| Reservoir, n (%) | |
| Coloplasty | 8 (6.1) |
| J-pouch colonic reservoir | 13 (9.8) |
| Lateroterminal anastomosis | 111 (83.5) |
| Derivative stoma n, (%) | |
| No | 59 (44.7) |
| Yes | 73 (55.3) |
| Complication of anastomosis, n (%) | |
| Yes | 3 (2.3) |
| No | 129 (97.7) |
| Radiotherapy, n (%) | |
| No | 65 (49.2) |
| Yes | 67 (50.8) |
| Short rt | 19 (14.4) |
| Long rt | 48 (36.4) |
PMR: partial mesorectal resection; TMR: total mesorectal resection; rt: radiotherapy.
Fig. 1 shows the distribution of the patients in the different LARS categories. As may be seen, 62 patients (47%) presented a major LARS.
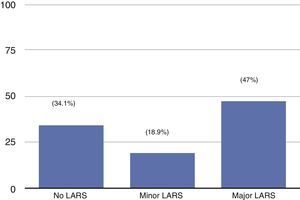
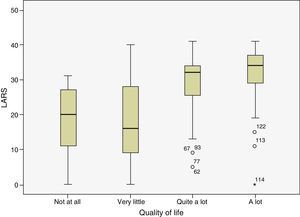
Fig. 2 shows the correlation between the LARS and the answer to the question on the effect of intestinal and defecatory symptoms on quality of life. A good correlation can be seen between a high LARS and greater effect on quality of life. Nevertheless, only when we group the categories “not at all” and “very little” on the one hand, and “quite a lot” and “a lot” on the other do we find significant differences between the 2 groups respecting LARS. No differences were found when the “not at all” and “very little” groups were compared, or when “quite a lot” was compared with “a lot”.
To study the correlation between the LARS and the selected variables, some of the latter were grouped as they lacked a sufficient number of patients. The following variables were grouped: the surgical approach (laparoscopy vs open plus converted), the construction of a reservoir (a colonic J-pouch plus coloplasty vs L-T anastomosis) and the administration of radiotherapy (yes vs no). Univariate analysis (Table 3) showed statistically significant differences for technique type and the mesorectal exeresis used (P<.001), the use of a reservoir or coloplasty (P=.017), the creation of a derivative stoma (P=.003) and the use of a long preoperative period of radiotherapy (P=.019).
Univariate Analysis. LARS vs Study Variables.
| Variables | LARS category | P | |||
|---|---|---|---|---|---|
| No | Minor | Grouped | Major | ||
| Age (average, years) | 68.3 | 66.3 | 67.3 | 69.1 | .45 |
| Time after surgery (average, months) | 39.7 | 37.3 | 38.5 | 35.5 | .38 |
| Sex | .82 | ||||
| Men | 30 | 17 | 47 | 43 | |
| Women | 15 | 8 | 23 | 19 | |
| Technique | <.001 | ||||
| LAR+PMR | 22 | 7 | 29 | 6 | |
| LAR+TMR | 23 | 18 | 41 | 56 | |
| Surgical approach | .37 | ||||
| Laparoscopic | 38 | 20 | 58 | 47 | |
| Conversion | 4 | 3 | 7 | 6 | |
| Open | 3 | 2 | 5 | 9 | |
| Grouped surgical approach | .297 | ||||
| Laparoscopic | 38 | 20 | 58 | 47 | |
| Open+conversion | 7 | 5 | 12 | 15 | |
| Anastomosis | .657 | ||||
| Manual | 4 | 4 | 8 | 5 | |
| Mechanical | 41 | 21 | 62 | 57 | |
| Reservoir | .017 | ||||
| Coloplasty or J-pouch | 7 | 8 | 15 | 6 | |
| L-T anastomosis | 34 | 21 | 55 | 56 | |
| Derivative stoma | .003 | ||||
| No | 26 | 14 | 40 | 19 | |
| Yes | 19 | 11 | 30 | 43 | |
| Complication of anastomosis | .641 | ||||
| Yes | 2 | 0 | 2 | 1 | |
| No | 43 | 25 | 68 | 61 | |
| Radiotherapy | .019 | ||||
| No | 29 | 10 | 39 | 26 | |
| Short rt | 8 | 5 | 13 | 6 | |
| Long rt | 8 | 10 | 18 | 30 | |
| Grouped radiotherapy | .097 | ||||
| No | 29 | 10 | 39 | 26 | |
| Yes | 16 | 15 | 31 | 36 | |
| Long rt | 48 (36.4) | ||||
PMR: partial mesorectal resection; TMR: total mesorectal resection; LAR: low anterior resection; rt: radiotherapy.
The significant variables for univariate analysis were included in the logistic regression model of the multivariate analysis. Only the type of technique and mesorectal exeresis used (P<.001), and the use of a reservoir or coloplasty (P=.002) are independently statistically significant for LARS.
DiscussionIn this study, half of the patients operated on for cancer of the rectum using low resection presented a major LARS, and only one-third had no quantifiable ARS. The overall perception of quality of life was significantly worse in patients with a major LARS. Total mesorectal resection and the form of reconstruction of the colorectal anastomosis were the main factors associated with the LARS.
These data agree with and reproduce those already published to validate the LARS scale in international studies.3 The response rate in this study was 70%, and although it would be desirable to have a higher rate of valid responses, this datum together with the previous one suggests that the causes studied are representative of the population of patients treated using anterior resection of the rectum. Moreover, as other studies have pointed out,1 the non-responders are often those whose functional results are the most extreme, thereby improving the balance.
The correlation found between the ARS quantification and the question of impact on quality of life reflects the importance of intestinal/defecatory dysfunction. Although quality of life is determined by many factors (physical, emotional, social and cognitive, etc.) and while the LARS does not ask about other aspects such as sexual or urinary dysfunction, a recent study demonstrated the importance of the ARS, quantified by LARS, in how patients perceive their quality of life as measured by the EORTC QLQ-C30.4
Although the functional alterations of the ARS are more intense and apparent in the first 12 months after surgery, after which the symptoms stabilise, the long-term results indicate that the ARS is a permanent alteration with a multifactor physiopathology.
The ARS has a wide range of symptoms; however, they can be divided into 2 types: those connected with continence (2 LARS questions) and defecatory alterations (3 LARS questions). It is interesting to observe that the surgeons and patients assess these symptoms differently: while surgeons tend to overestimate the aspects in connection with continence and to underestimate those relating to defecatory dysfunction, the patients attribute contrasting degrees of importance to these factors.6
In connection with the alteration of continence, it has been said that the reduction of sphincter tone that is often observed after an anterior resection, is due more to injury to the intra- and extramural nervous plexus than because of the complete mobilisation of the rectum, that it is to structural damage to the sphincter.1
On the other hand, defecatory dysfunction (fragmentation and frequency) is connected to the reduction in volume and compliance of the colon compared to the rectum, with the loss of anorectal coordination and sensitivity, and with the alteration in colonic motility.1 The latter has chiefly been observed following rectal resection, although less intensely; it may also occur following a sigmoidectomy.7
As could be expected, the LARS score was higher in cases of low anterior resection with total mesorectal excision than it was in cases of partial or subtotal excision. This aspect in turn reflects the height of the rectal tumour and the need to perform a total or subtotal proctectomy, together with the functional implication of the absence of all or part of the rectum.
Other aspects that may affect the severity of the ARS are the way the colorectal anastomosis is reconstructed, the absence of complications and the administration of pelvic radiation. We found a correlation between the creation of some type of colonic reservoir and the LARS. This coincides with known aspects relating to the functional superiority of reservoirs over terminoterminal anastomosis, while also highlighting the capacity of the LARS to discriminate these results.
Unlike the LARS scale validation studies, we found no clear indication of the role of radiotherapy in the quantification of the ARS using the LARS. The limited number of cases in our study for this factor is clearly a restriction here. Additionally, the tendency towards a minor LARS in patients treated with short radiotherapy may be due to the fact that this is used more in upper rectal tumours.
Many authors have pointed out the pernicious effects of radiotherapy on intestinal functioning after anterior resection. Nevertheless, if radiotherapy had a relevant role in the development of the ARS, the intestinal dysfunction could be expected to increase over time rather than stabilising. Other authors have stated that the impact of radiotherapy on quality of life and urogenital functioning is less than expected, although the studies in question followed abdominoperineal resection.8 In any case, current radiotherapy techniques and regimes are able to restrict harm in comparison with older therapies.9
To conclude, almost half of the patients operated for cancer of the rectumby anterior resection present an ARS quantified as “major” on the LARS scale, which affects their quality of life. Complete proctectomy with total mesorectal excision is the most important independent risk factor for a major LARS. The LARS scale, validated in Spanish, is a simple and quick means of quantifying the ARS and comparing the functional results of different therapeutic or reconstructive strategies following rectal resection. It may also be useful in evaluating the duration of the efficacy of different treatments which have the aim of relieving or improving the ARS.
Authorship/CollaboratorsStudy conception and design: Alberto Carrillo.
Critical revision of the manuscript and contribution to its contents: José María Enriquez-Navascués.
Data gathering and processing: Araceli Rodríguez, Ander Timoteo and Nerea Borda.
Statistical analysis and interpretation: Carlos Placer and José Andrés Múgica.
Draft manuscript: Alberto Carrillo and Yolanda Saralegui.
Revision and approval of the manuscript: all of the authors.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Carrillo A, Enríquez-Navascués JM, Rodríguez A, Placer C, Múgica JA, Saralegui Y, et al. Incidencia y caracterización del síndrome de resección anterior de recto mediante la utilización de la escala LARS (low anterior resection score). Cir Esp. 2016;94:137–143.