Like other primary hepatic tumours such as cholangiocarcinoma, colorectal liver metastases (CLM) can infiltrate the biliary ducts and adopt a pattern of intrabiliary growth.
We describe the case of a 64-year-old male patient who had been in treatment since October 2009 for rectal adenocarcinoma (pT3N0M1) at another hospital and who presented synchronous liver metastasis in segment V. As the rectal resection was radical, and given that the volume of liver disease was small, direct liver surgery was indicated.
In December 2009, limited resection of segment V was performed with segmentectomy of segment VI due to another metastasis that was discovered intraoperatively. The definitive pathology report confirmed that the resection margins were not affected by the tumour. Afterwards, the patient received 6 cycles of chemotherapy (CTx).
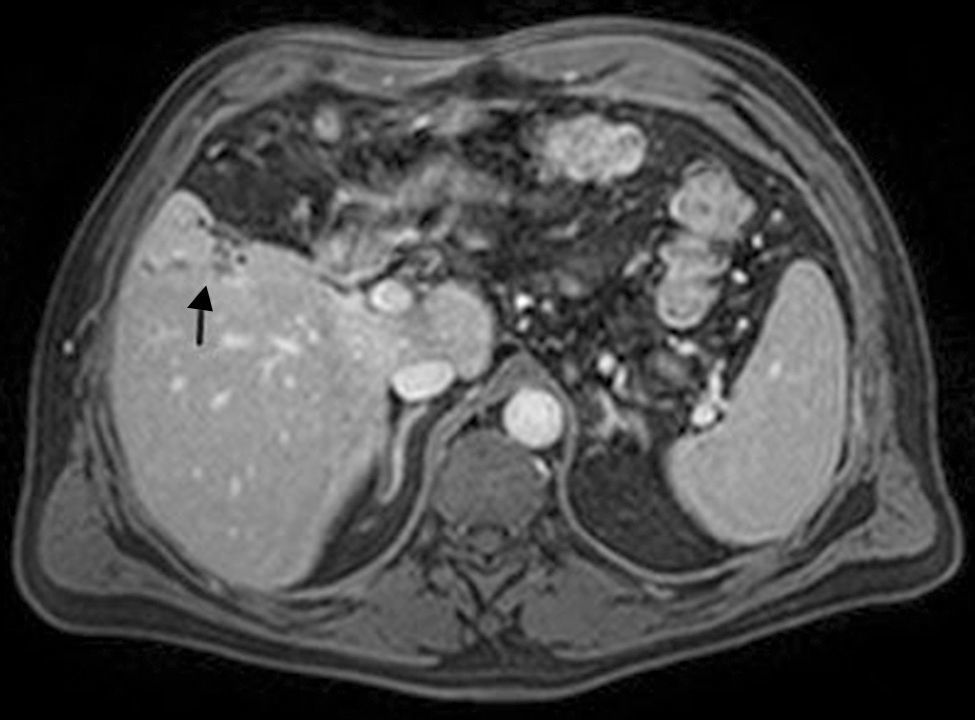
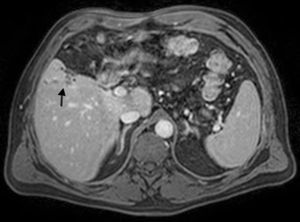
In July 2011, the patient was diagnosed with a hepatic recurrence in segment V that was not in contact with the previous resection margin, and it was therefore considered a new metastasis. Complementary tests (Fig. 1) detected an image suggestive of a dilated bile duct corresponding with segment V. Said image had not been observed in previous follow-up tests.
The patient was treated surgically once again in October 2011, at which time segmentectomy V was done after an extra-Glissonian approach of the pedicle. The definitive pathology report confirmed the presence of a metastatic lesion with intrabiliary tumour infiltration and intraluminal progression (Fig. 2). The resection margins were tumour-free. After surgery, treatment with CTx was indicated.
In October 2013, a hepatic lesion was once again identified, which in this case was adjacent to the surgical resection margin and was therefore considered compatible with tumour recurrence or persistence.
In January 2014, the patient was operated on and, although right hepatectomy had been planned, limited resection was ultimately done due to technical difficulties. The pathology study confirmed the metastatic lesion, with no invasion of the bile duct. Currently, the patient is disease free.
Most publications about CLM with intrabiliary growth have been written by Japanese authors,1–3 who argue that this is a frequent clinical situation that can be observed in up to 40.6% of cases, although the involvement is macroscopi in only 12% of cases.
In western countries, there have only been publications of some isolated cases and series,4–7 and it is difficult to establish the incidence of this clinical situation. One study by Jhavery et al.6 in 2009 observed intrahepatic bile duct dilatation in 16.5% of patients with CLM. This publication also concluded that there was no correlation between the size of the hepatic focal lesion and the probability of presenting bile duct dilatation. More recently, a publication by Jeannelyn et al.7 observed intrabiliary growth in 3.6%–10.6% of CLM. In more than 50% of cases, the infiltration affected major bile ducts and adopted 2 possible types of growth: (1) substitution of biliary epithelium and (2) formation of “plugs” in the bile duct lumen.
Intrabiliary infiltration produces data of cholestasis in the hepatic biochemistry and can alter the histology of the surrounding parenchyma, causing changes related with the bile duct obstruction and episodes of focal cholangitis. From a radiological standpoint, intrahepatic masses are observed associated with bile duct dilatation and thickening of the duct walls, especially when there is involvement of a major bile duct. Okano et al.8 described several radiological signs related with the presence of macroscopic intrabiliary invasion: thickening of the portal pedicle, biliary dilatation and observation of a wedge-shaped hypervascular area.
The differential diagnosis with cholangiocarcinoma9 is not usually difficult, but more difficulties arise when the disease-free interval is prolonged and when there is involvement of major bile ducts. In these cases, diagnosis is only possible in the histological study by applying immunohistochemistry techniques (CK20+ and CK7−).
Some studies done in Japan have suggested that this phenomenon can imply a less aggressive form of CLM.1,10 In the study by Okano et al.,10 patients with macroscopic intrabiliary involvement presented a 5-year survival rate of 80%, compared to 57% of patients without bile duct involvement. The observations by Kubo et al.1 could explain these results, since colorectal primary tumours whose metastases are associated with macroscopic biliary invasion are usually well differentiated, with no venous invasion and with a longer disease-free interval after colectomy. In contrast, in the study by Jeannelyn et al., bile duct invasion was not observed to influence survival.
Although there are no conclusive specific studies, the clinical importance of intrabiliary growth mainly lies in its possible role as a risk factor for recurrence in the resection margins. Consequently, surgeons should be well informed of this clinical situation in order to preferentially plan anatomical resections that are extensive enough to include the dilatation, and to conduct intraoperative histology studies of the margins.2
Please cite this article as: Lopez Gordo S, Ramos Rubio E, Torras Torra J, Lladó Garriga L, Rafecas Renau A. Crecimiento endobiliar de las metástasis de carcinoma colorrectal. Cir Esp. 2016;94:115–116.
No funding was received for the preparation of this article in the form of grants. The data has not been previously presented at any medical conference.