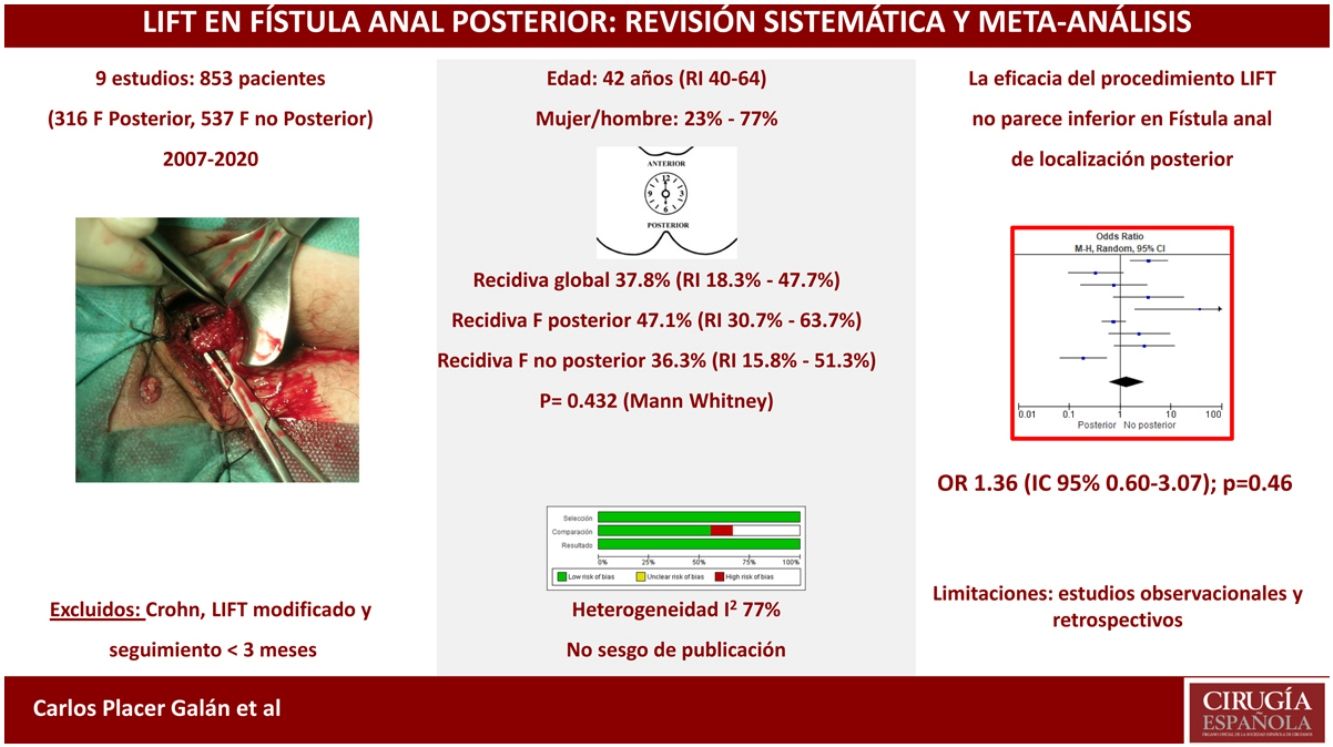
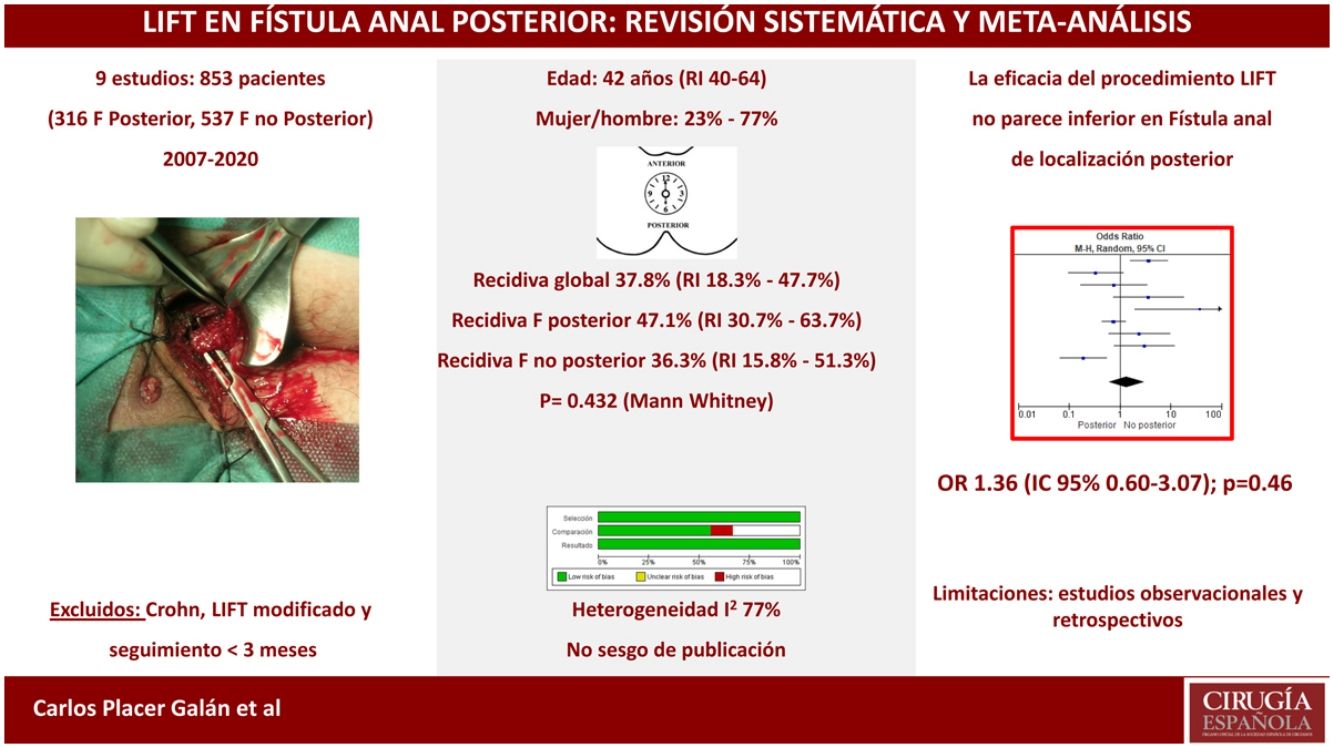
Efficacy of the ligation of intersphincteric fistula tract (LIFT) procedure for posterior fistula-in-ano remains under debate. However, there is scarcity of quality evidence analysing this issue. Thus, the aim of this study is to evaluate outcomes of LIFT surgery in patients with posterior anal fistula.
Material and methodsSystematic review and meta-analysis to evaluate efficacy of LIFT procedure for posterior anal fistula. MEDLINE (PubMed), EMBASE, Scopus, Web of Science, Cochrane Library and Google Scholar data sources were searched for key-words (MeSH terms): “LIFT” OR “Ligation of the intersphincteric fistula tract” AND “posterior anal fistula” OR “posterior fistula-in-ano”. Original, observational and experimental, non-language restriction studies published from January 2000 to March 2020 and reporting outcomes on LIFT procedure for posterior anal fistula were reviewed. Quality and potential biases were assessed using Newcastle-Ottawa scale, following AHRQ recommendations. Additional sensitivity analysis and publication bias evaluation (Beg and Egger’s test) were performed.
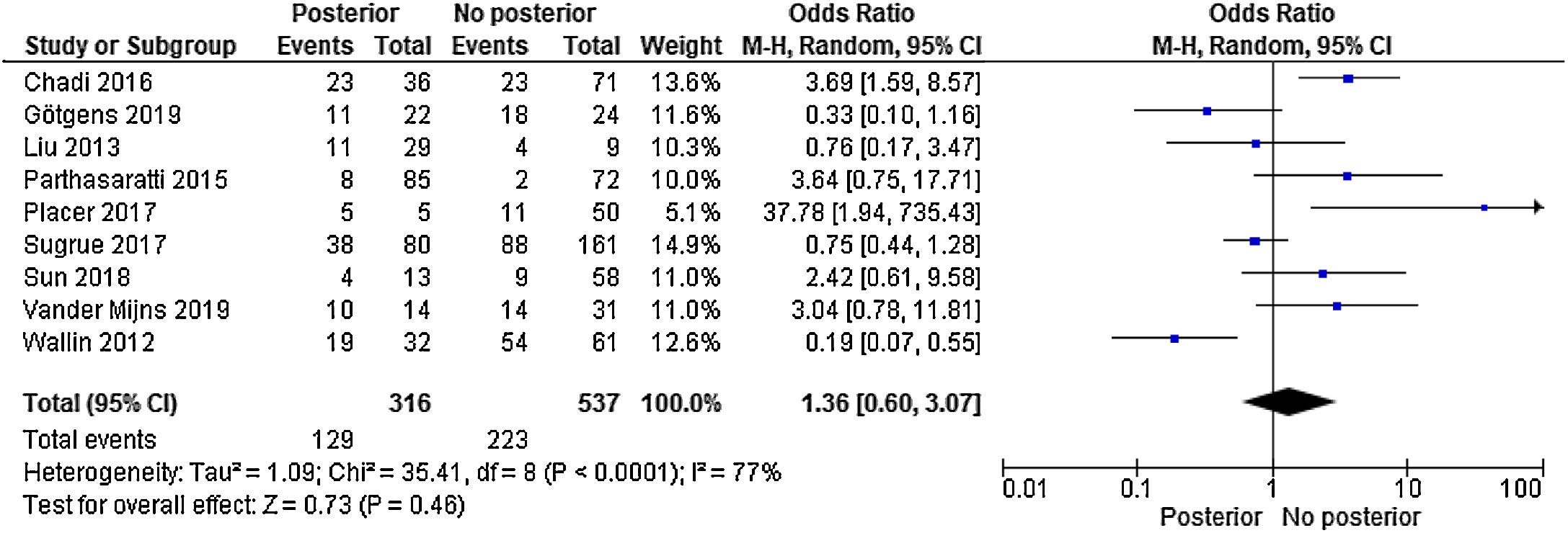
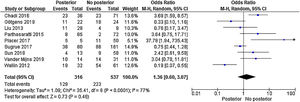
ResultsNo significant differences were found in recurrence rate among patients undergoing LIFT procedure for posterior fistula-in-ano in contrast to other locations (OR 1.36 [95%CI 0.60–3.07]; P = .46). I2 test value was 77%, expressing a fair heterogeneity among included studies. The weighed median for overall recurrence was 37.8% (IQR 18.3%-47.7%); with a weighed median of 47.1% (IQR 30.7% - 63.7%) and 36.3% (IQR 15.8%-51.3%) (P= .436) respectively for recurrence after LIFT for posterior fistula and fistula in other locations. There was not clear evidence about the sample size (n) of included studies nor the disparities in quality assessment of those, could justify the observed heterogeneity. No significant publication bias was found.
ConclusionThis systematic review and meta-analysis suggests that there are no clear data in the literature for not performing the LIFT procedure in posteriorly located fistulas.
El procedimiento LIFT para las FA de localización posterior ha sido cuestionado. Sin embargo esta controversia no ha sido analizada previamente y es el objetivo de esta revisión sistemática con metaanálisis.
Material y métodoRevisión sistemática PRISMA, de las bases MEDLINE (PubMed), EMBASE, Scopus, Web of Science, Cochrane Library y Google Scholar hasta marzo de 2020. La evaluación de la calidad y sesgos de los estudios seleccionados se ha realizado mediante la escala Newcastle-Ottawa, según la AHRQ. Se empleó el método inverso de la varianza y el modelo de efectos aleatorios. Además, se realizó un análisis de sensibilidad y sobre el sesgo de publicación mediante funnel-plot y las pruebas de Beg y Egger.
ResultadosNo se apreciaron diferencias significativas en el porcentaje de recurrencias entre los pacientes con fístula posterior y el resto de localizaciones (OR 1,36 [IC 95% 0,60-3,07]; p = 0,46). El valor I2 fue de 77%, lo cual muestra la heterogeneidad de resultados entre los estudios elegidos. Los 9 estudios incluidos presentaron una mediana ponderada (RI) de recidiva global del 37,8% (RI 18,3-47,7%), recidiva de fístula posterior del 47,1% (RI 30,7-63,7%) y de fístula no posterior del 36,3% (RI 15,8-51,3%) (p = 0,436). Ni el número de pacientes ni la diferente calidad metodológica de los estudios explican el nivel de heterogeneidad de los mismos. No se demostró sesgo de publicación.
ConclusionesNuestro metaanálisis sugiere que no existen datos claros en la literatura para no realizar el procedimiento LIFT en fístulas de localización posterior.
The goals of anal fistula treatment are to achieve a cure, prevent recurrence/persistence, and maintain continence. The treatment of complex anal fistula (which cannot be resolved with a simple fistulotomy) continues to be a surgical challenge, which is proven by the wide variety of techniques used today.
In 2007, Rojanasakul described a new sphincter-preservation technique, intersphincteric ligation of the fistulous tract (LIFT),1 by readapting the intersphincteric approach previously described by the St. Mark’s group in 1993.2
The LIFT procedure has been gaining popularity in the last decade by associating an acceptable percentage of cure (greater than 70%) with little impact on anal continence.3 Furthermore, around one-third of recurrences do so in the form of intersphincteric fistula, transforming the initial complexity into a simple second intervention (downstaging).4
The LIFT technique is based on the dissection and ligation of the fistulous tract in the intersphincteric plane, which requires consistent tissue and the absence of abscess in this plane. Some studies have reported obtaining worse results in posterior fistulas, possibly related to greater technical complexity.5–7 However, this issue has not been previously analyzed.
Given the absence of studies designed to answer this question, the objective of this study was to carry out a systematic search of the literature and provide consistent data for decision-making on the impact of posterior anal fistulas on the success rate of the LIFT procedure.
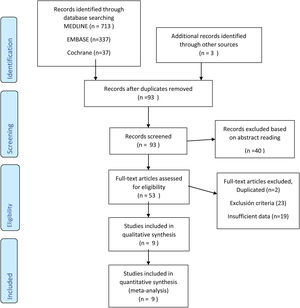
MaterialsWe performed a systematic review of the literature, following the recommendations of Preferred Reposting Items for Systematic Reviews and Meta-Analysis Statement (PRISMA)8 (Appendix B).
Search strategyThe study search strategy was carried out on the MEDLINE (PubMed), EMBASE, Scopus, Web of Science, Cochrane Library and Google Scholar electronic databases. We also conducted a manual secondary search of bibliographic references found in the selected studies. A combination of MeSH terms and keywords were used: “LIFT” OR “Ligation of intersphincteric fistula tract” AND “posterior location” OR “post-anal fistula” AND “anal fistula” OR “fistula-in-ano”. The search ended in March 2020.
Eligibility criteriaThree independent reviewers checked the inclusion criteria, titles and abstracts. Duplicates were removed and articles were selected for full reading. Reasons were given for exclusion, and discrepancies were resolved by consensus. The following data were chosen for each study: author and year, study design, sample size, patient age and sex, follow-up time, and percentage of recurrence/cure according to the location of the fistula. Some authors were contacted to complete information.9 Other authors could not be contacted (Appendix B).
The studies selected met the following inclusion criteria: 1) studies about LIFT with data on the location of the fistulas and the results (success vs recurrence); 2) No exclusions were made for language; 3) Definition of cure and failure. Exclusion criteria were: 1) studies with fewer than 20 patients; 2) Fistula in Crohn’s disease; 3) Modified LIFT (BIO-LIFT, LIFT with anal flap, etc); 4) Follow-up of fewer than 3 months.
Quality of the studiesThe quality and biases of the selected studies were evaluated with the Newcastle-Ottawa scale (NOS) for non-randomized studies,10 collecting stars in 3 domains: selection, comparability and result (outcome). These were classified as good quality, weak quality, and poor quality, according to the Agency for Health Research and Quality (AHRQ).11 Three independent authors (TP, IA, YS) assessed the studies and, when there was lack of agreement, a fourth author (CPG) was used.
Statistical analysisThe statistical analysis was performed with the Review Manager (RevMan) program v.5.3 (Copenhagen: The Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen Denmark, 2014). The OR were calculated from the original data. The values were expressed with a 95% confidence interval (CI). Heterogeneity among the included studies was qualitatively assessed using the chi squared based on the Q test. A P value less than 0.05 showed that there was no significant heterogeneity between the studies. The level of heterogeneity between the studies was calculated using the I2 statistic. An I2 <30% was considered low in heterogeneity. Given the heterogeneity of the data, according to the I2 test, the inverse variance method and the random effect model were used for the quantitative analysis of dichotomous variables. In addition, a sensitivity analysis was done by grouping the studies according to the number of patients included and according to the NOS quality. The publication bias analysis was obtained with a funnel-plot as well as Begg’s and Egger’s tests.
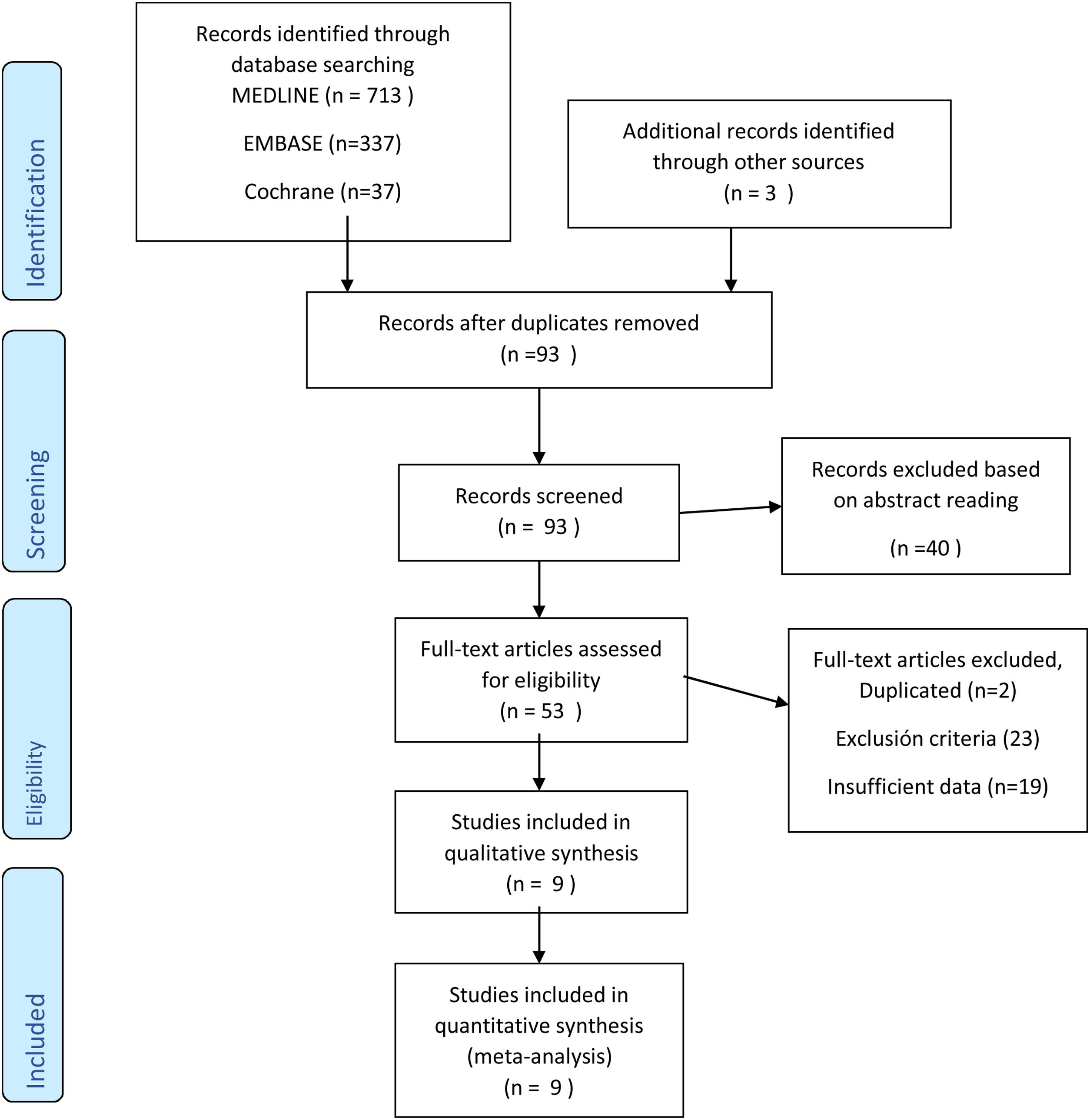
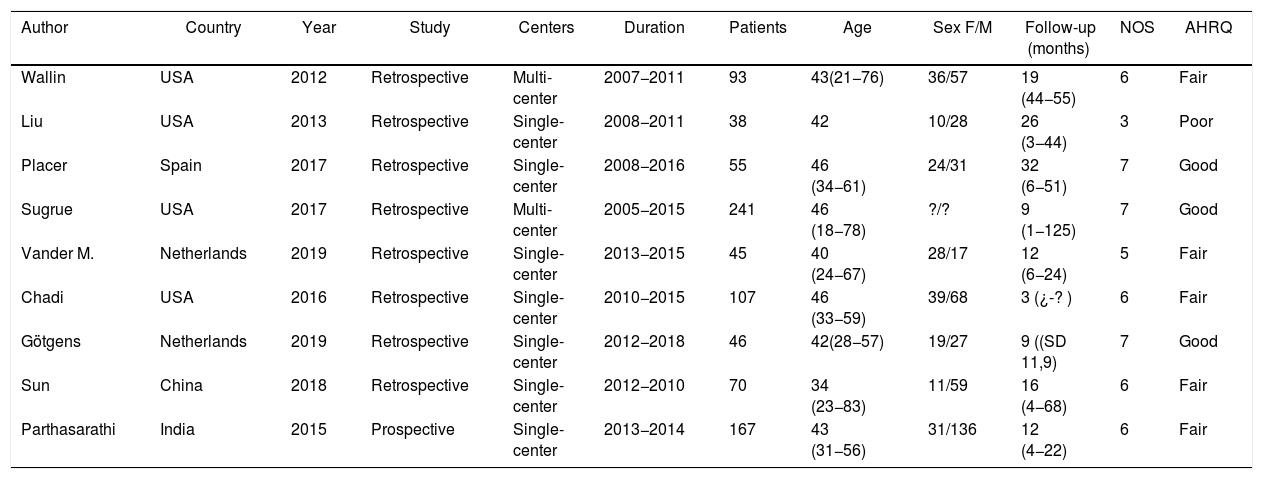
ResultsWe have conducted a systematic search from 2007 (when the LIFT technique was described) to March 2020. After reviewing the title and abstracts, 53 papers were selected and finally 9 studies were included with 853 patients for qualitative and quantitative analysis (Fig. 1).5–7,9,12–16 The median age was 42 years (IQR 40–46), and the female:male ratio was 23% to 77%. Most studies that were excluded were due to sample size (<20 patients), lack of data for results in terms of fistula location, and a smaller number of studies with mixed techniques (Bio-LIFT, additional flap, etc) or those that included patients with Crohn’s disease. Almost all the studies included were retrospective (cohorts or case series) and included patients treated between 2007 and 2018. Half of the studies included were from the US, and most were single-center. The median number of patients per study was 63 (IQR 43–103). The median follow-up time was more than one year, except for one study (more than 3 months).16,17 Most studies treated transsphincteric fistulas with some cases of intersphincteric, recto-vaginal and posterior horseshoe fistulas (Tables 1 and 2). All the studies defined the criteria for cure/failure. However, few studies assessed impaired continence or complications based on the location of the fistula.
Characteristics of the studies and patients included.
| Author | Country | Year | Study | Centers | Duration | Patients | Age | Sex F/M | Follow-up (months) | NOS | AHRQ |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Wallin | USA | 2012 | Retrospective | Multi-center | 2007−2011 | 93 | 43(21−76) | 36/57 | 19 (44−55) | 6 | Fair |
| Liu | USA | 2013 | Retrospective | Single-center | 2008−2011 | 38 | 42 | 10/28 | 26 (3−44) | 3 | Poor |
| Placer | Spain | 2017 | Retrospective | Single-center | 2008−2016 | 55 | 46 (34−61) | 24/31 | 32 (6−51) | 7 | Good |
| Sugrue | USA | 2017 | Retrospective | Multi-center | 2005−2015 | 241 | 46 (18−78) | ?/? | 9 (1−125) | 7 | Good |
| Vander M. | Netherlands | 2019 | Retrospective | Single-center | 2013−2015 | 45 | 40 (24−67) | 28/17 | 12 (6−24) | 5 | Fair |
| Chadi | USA | 2016 | Retrospective | Single-center | 2010−2015 | 107 | 46 (33−59) | 39/68 | 3 (¿-? ) | 6 | Fair |
| Götgens | Netherlands | 2019 | Retrospective | Single-center | 2012−2018 | 46 | 42(28−57) | 19/27 | 9 ((SD 11,9) | 7 | Good |
| Sun | China | 2018 | Retrospective | Single-center | 2012−2010 | 70 | 34 (23−83) | 11/59 | 16 (4−68) | 6 | Fair |
| Parthasarathi | India | 2015 | Prospective | Single-center | 2013−2014 | 167 | 43 (31−56) | 31/136 | 12 (4−22) | 6 | Fair |
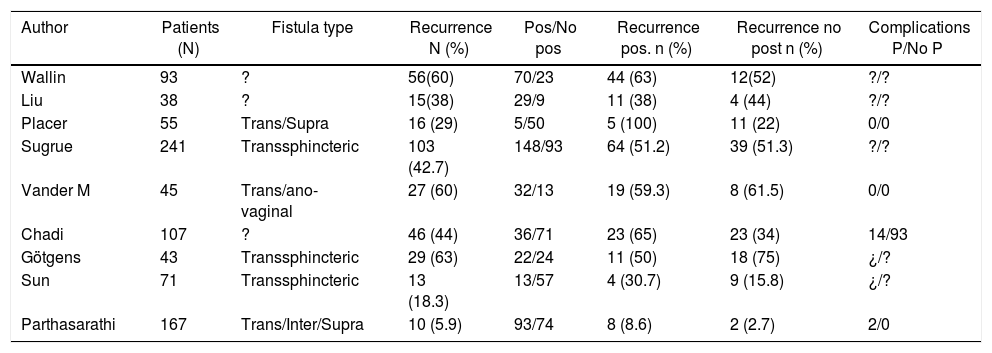
Results of the LIFT procedure in studies according to the location of the fistula.
| Author | Patients (N) | Fistula type | Recurrence N (%) | Pos/No pos | Recurrence pos. n (%) | Recurrence no post n (%) | Complications P/No P |
|---|---|---|---|---|---|---|---|
| Wallin | 93 | ? | 56(60) | 70/23 | 44 (63) | 12(52) | ?/? |
| Liu | 38 | ? | 15(38) | 29/9 | 11 (38) | 4 (44) | ?/? |
| Placer | 55 | Trans/Supra | 16 (29) | 5/50 | 5 (100) | 11 (22) | 0/0 |
| Sugrue | 241 | Transsphincteric | 103 (42.7) | 148/93 | 64 (51.2) | 39 (51.3) | ?/? |
| Vander M | 45 | Trans/ano-vaginal | 27 (60) | 32/13 | 19 (59.3) | 8 (61.5) | 0/0 |
| Chadi | 107 | ? | 46 (44) | 36/71 | 23 (65) | 23 (34) | 14/93 |
| Götgens | 43 | Transsphincteric | 29 (63) | 22/24 | 11 (50) | 18 (75) | ¿/? |
| Sun | 71 | Transsphincteric | 13 (18.3) | 13/57 | 4 (30.7) | 9 (15.8) | ¿/? |
| Parthasarathi | 167 | Trans/Inter/Supra | 10 (5.9) | 93/74 | 8 (8.6) | 2 (2.7) | 2/0 |
The assessment of the methodological quality of the studies with the NOS scale was low, with an Agency for Healthcare Research and Quality (AHRQ) classification that showed 3 good quality studies, 5 weak quality studies and one poor quality study (Appendix B).
No significant differences were observed in the percentage of recurrences between patients with a posterior fistula and the remaining locations (OR 1.36 [95%CI 0.60–3.07]; P = .46). The I2 value was 77%, which shows the heterogeneity of results between the chosen studies. The 9 included studies presented a weighted median and interquartile range (IQR) for global recurrence of 37.8% (IQR 18.3%-47.7%), posterior fistula recurrence 47.1% (IQR 30.7%-63.7%), and non-posterior fistula 36.3% ( 15.8%-51.3%) (P = .436; Mann Whitney) (Fig. 2).
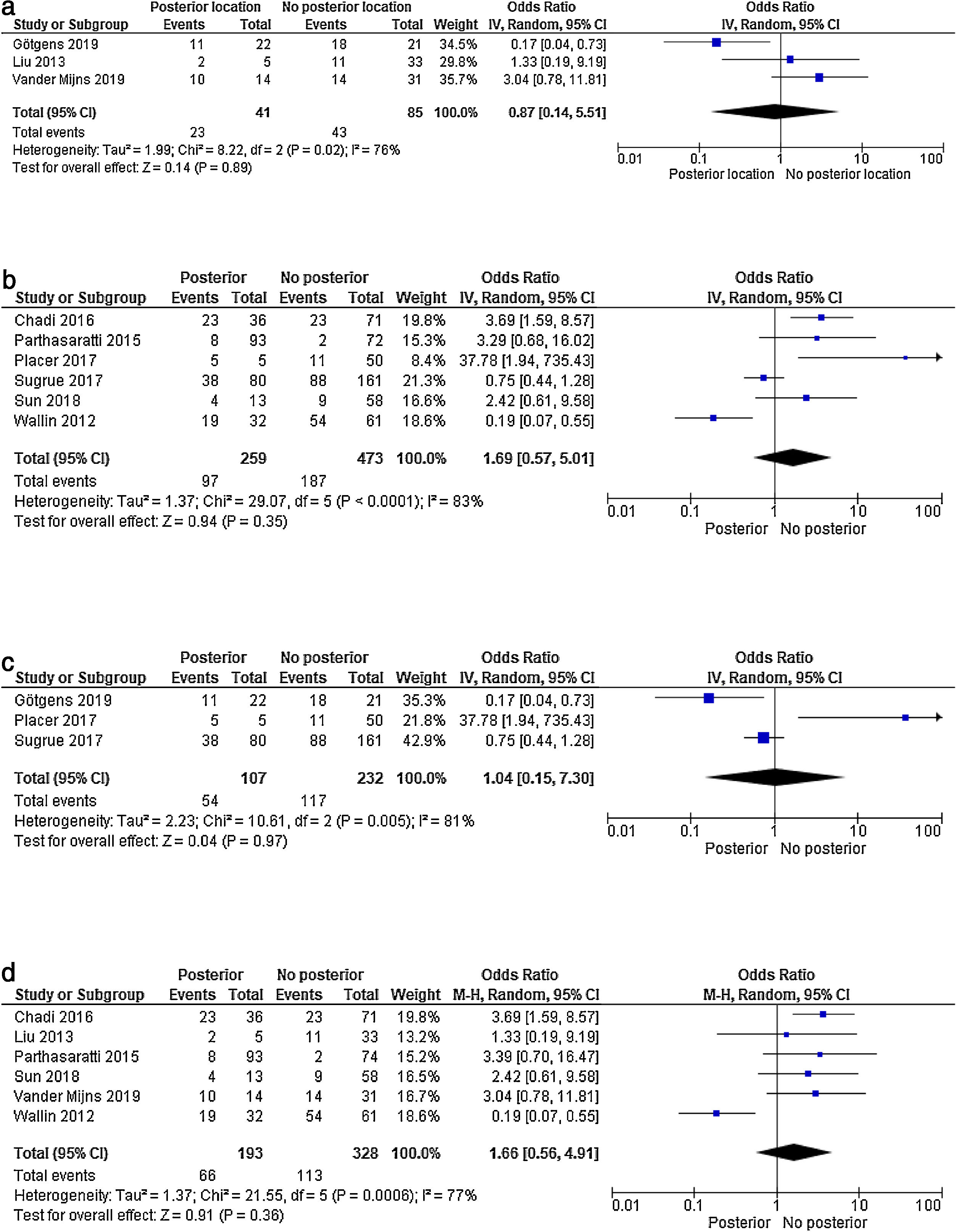
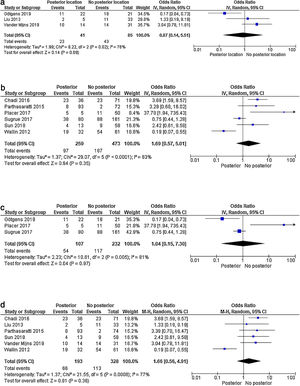
A sensitivity analysis was performed according to the number of patients included in each selected study (with >/<50 patients) and the NOS quality of the studies. In the study subgroups, according to the number of patients as well as the NOS scale, no differences in results were observed between the posterior location and the remaining locations (Fig. 3 a–d). Therefore, neither the number of patients nor the different methodological qualities of the studies explain their level of heterogeneity.
Forest plot of the sensitivity analysis: a) Forest plot of recurrences according to sample size (studies with <50 patients); b) Forest plot of recurrences according to sample size (studies with >50 patients); c) Forest plot according to NOS quality scale – good quality studies; d) Forest plot according to NOS quality scale: weak and poor quality studies.
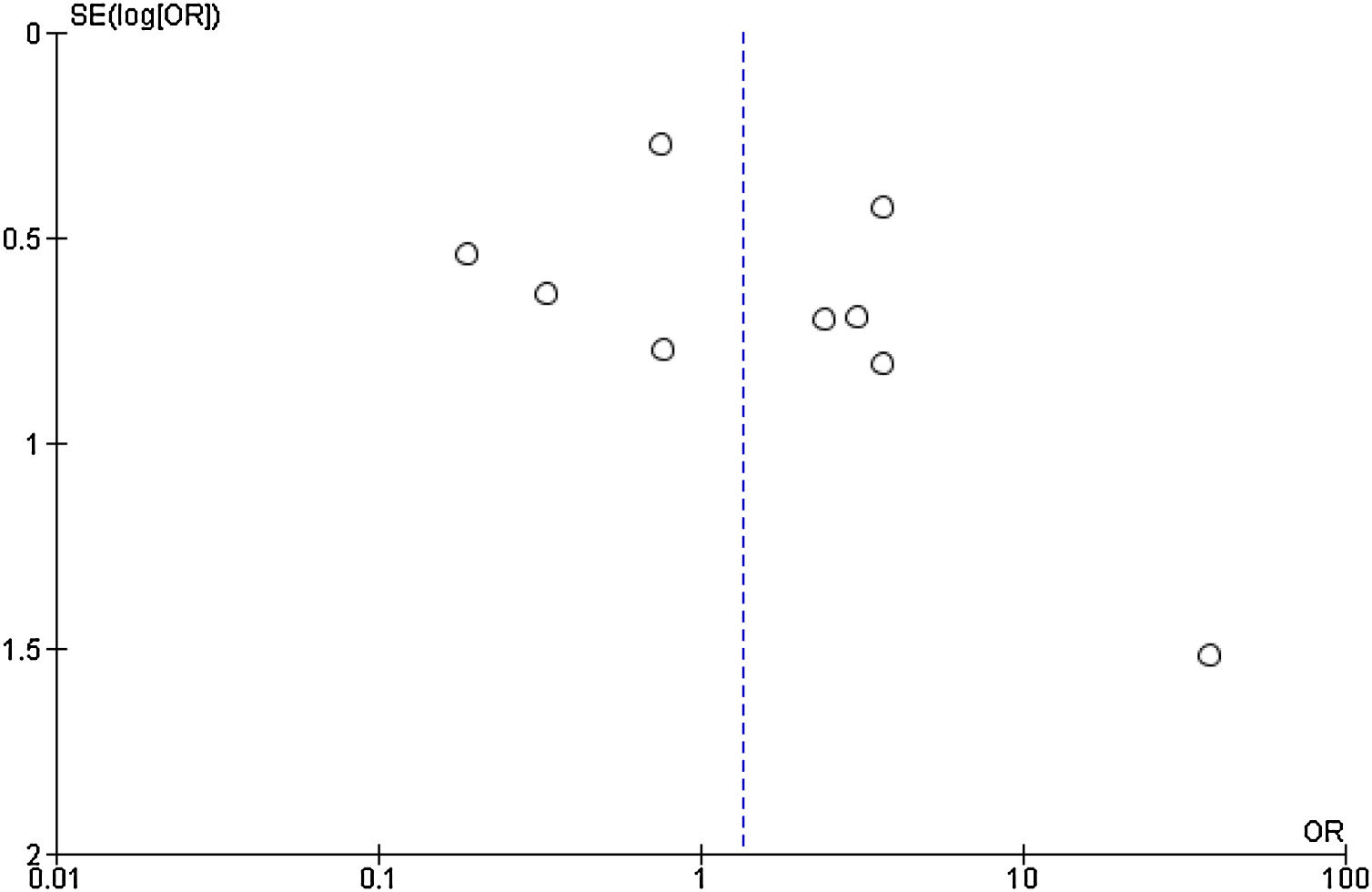
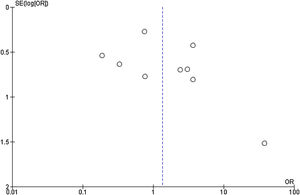
Publication bias was assessed using a funnel plot (Fig. 4). In addition, the Begg’s (Z = 0.9383; P = 0.3481) and Egger’s (t = 01.1248; P = .2978) tests were used. All three tests showed an absence of publication bias.
DiscussionThis systematic review and meta-analysis of the most recent data shows that the LIFT procedure does not obtain worse results in posterior anal fistulas. However, the risk of selection bias inherent in the included retrospective and uncontrolled studies should be understood for correct interpretation of the results. Furthermore, although a clear publication bias has not been observed, the number of studies that present the results according to the location of the fistula is small; therefore, the sample size could yield a type II error.
The idea of the intersphincteric approach is not new and is a consequence of the cryptoglandular theory of most anal fistulas. In 1993, Matos et al. published a series of 13 cases (8 high transsphincteric fistulas and 5 suprasphincteric) with success in 7/13 (54%) and a mean follow-up of 22 months (4–33).2 Despite not being widely utilized, in 2007 Rojanasakul took up the idea again and described a modified technique, the LIFT procedure.1
Very few studies have analyzed the location factor in the LIFT procedure.5–7 The Cleveland group, in a study of 107 LIFT procedures, presented an overall success rate of 55%, but only 35% in the posterior location (OR 3.9; P = .004). Their hypothesis is based on the greater complexity of the technique due to the depth of the path at this level, its greater caliber and the possible involvement of the deep postanal space.5 Placer et al. did not obtain any cure in 5 complex posterior fistulas (1 suprasphincteric and 4 high transsphincteric). In 2 cases, the anal canal mucosa was injured during dissection.6 This is a poorly described lesion, but it is the cause of poor results after dissection of a deep fistulous tract or with fibrosis in the intersphincteric space.
Intersphincteric ligation requires the absence of active infection in this area, the presence of a mature tract (fibrous or consistent), and the absence of secondary tracts. In posterior fistulas, the path is usually larger and deeper in the anal canal. This can make the ligation technique difficult and increase the risk of injury to the anal mucosa during dissection. However, the posterior location has not been associated with worse results in anal fistula surgery, despite it being well known that most complex fistulas have a posterior origin, and this may represent a significant bias if not included in a multivariate analysis. One recent study on the epidemiology of transsphincteric fistulas, with a series of 300 patients, showed that 82.5% of high transsphincteric fistulas were posterior, with an OR of 8.5 (95%CI 4.17–17.48) in the multivariate analysis.18 Also, the presence of abscesses in posterior fistulas has been reported in 47% versus 5% in anterior fistulas.17 Several reviews on recurrences in anal fistula surgery have not addressed the location as a risk factor, and almost all have focused on the Goligher classification as the main variable, attributing to the higher forms (supra- and high transsphincteric) a higher percentage of recurrence/persistence.19–21 In a recent meta-analysis on risk factors for recurrence, Mei et al. did not identify location as a risk factor for recurrence/persistence.22 In the studies included in this review, it is striking that only 37% of the fistulas were located posterior, which may lead to a selection bias and ultimately less use of the LIFT procedure in posterior fistulas.
The main weakness of this study is that it is based on retrospective observational studies that have not been designed for this purpose. In addition, as they are no prospective studies, the circumstance of abandoned procedures may occur due to the impossibility of performing proper ligation of the fistulous tract cause by the complexity; therefore, these have not been included in the studies. It would be very interesting for future studies on the LIFT procedure to present their results analyzing the location of the fistula and have an adequate sample size to draw consistent conclusions.
However, the thorough bibliographic search and the inclusion/exclusion criteria have allowed us to obtain a representative sample of studies. Furthermore, ours is the first study on the impact of the location of the anal fistula on the results of the LIFT procedure.
With the inherent limitations of retrospective and intermediate-quality studies, this meta-analysis concludes that there are no data in the literature to not indicate the LIFT procedure in anal fistulas in posterior locations. Nevertheless, the results should be interpreted with caution due to the heterogeneity of the studies published.
Authorship/collaboratorsStudy design and concept: CPG. Data collection, analysis and interpretation: CPG, IA, TP, AE. Critical review: CPG, JMEN. Approval of the final version: CPG, IA, TP, AE, JMEN.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Placer Galán C, Aguirre I, Pastor T, Etxart A, Enriquez Navascués JM. Procedimiento LIFT en fístulas anales de localización posterior. ¿Son buenos los resultados? Revisión sistemática y metaanálisis de estudios observacionales. Cir Esp. 2021;99:183–189.