Solitary fibrous tumors (SFT) are rare mesenchymal neoplasms that appear mainly in the pleura, meninges, etc., and their location in the liver1 or the pancreas2 is especially rare. Symptoms are non-specific and related with the anatomical location and tumor size.3
The majority of these lesions are benign, but they may have an aggressive behavior, with possible local recurrence4,5 and distant metastasis.1,6–9 The treatment of choice is surgical resection.3–10 We present the first case described in the literature of the surgical resection of one liver and two pancreatic metastases of a meningeal SFT.
We present the case of a 40-year-old male who underwent complete resection of a left frontal SFT in 1998. In 2009, he was treated surgically once again for a recurrence in the same region, with complete re-resection.
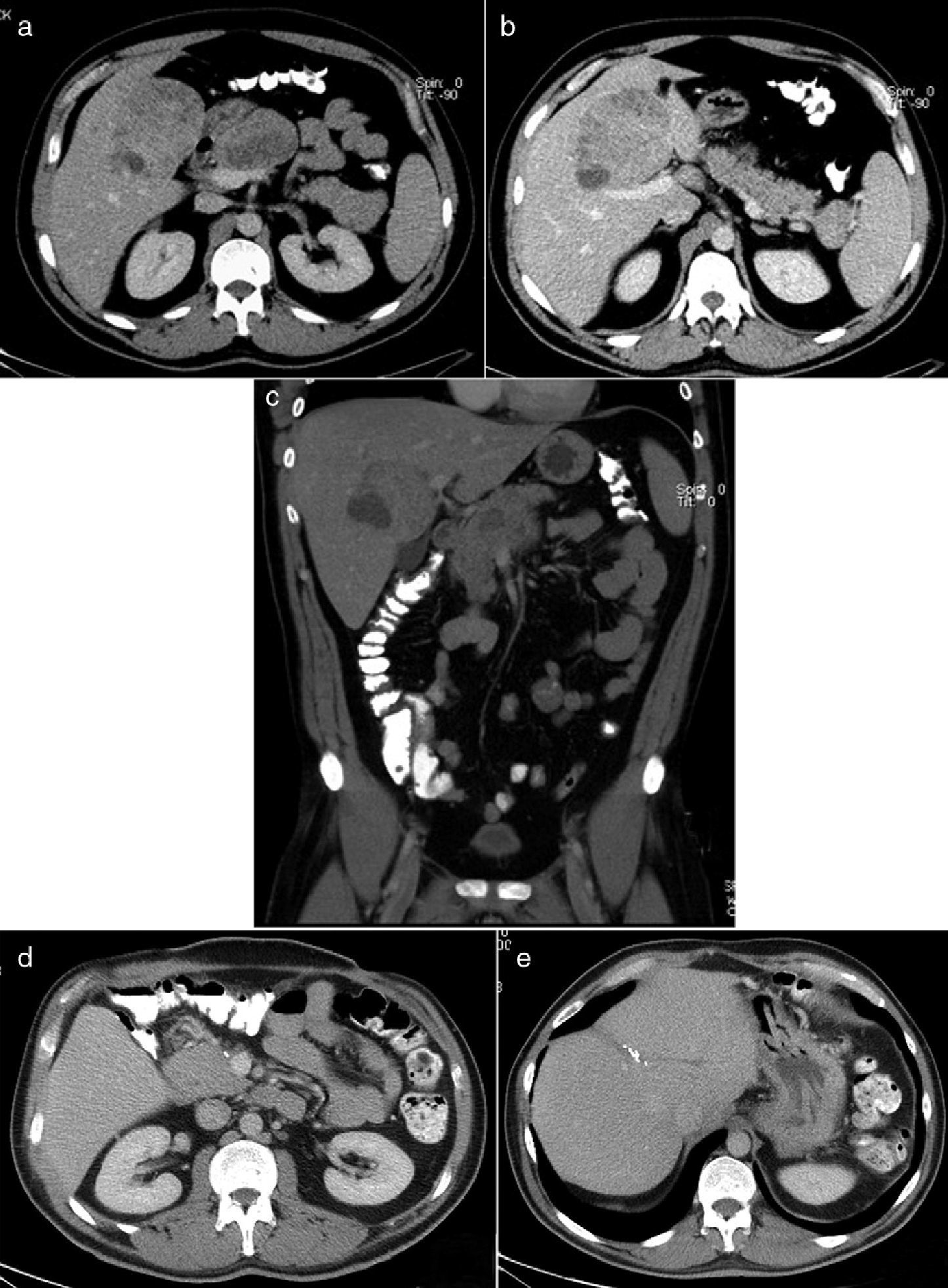
During the postoperative period after this latest procedure, the patient began to have abdominal pain. Abdominal computed tomography showed evidence of a liver mass measuring 8cm that was suggestive of metastasis as well as 2 tumor formations in the pancreas: a 7cm mass in the head/body of the pancreas (Fig. 1a and c) and a 4cm mass in the tail (Fig. 1b). Fine needle aspiration of the 2 lesions was compatible with SFT metastasis. Surgery was performed, which revealed a large central mass lying on the portal bifurcation that infiltrated the left liver duct as well as another lesion in the head/body of the pancreas attached to the portal vein, and another tumor in the tail of the pancreas. In the same intervention, we performed a total pancreatectomy followed by central hepatectomy. Caudal pancreatectomy was done first, followed by pancreatectomy of the head and body, due to the proximity of the portal vein and the lesion, and its dissection was possible under total vascular occlusion. Afterwards, central hepatectomy of segments IV, V and VIII was completed, with partial resection of the left bile duct and end-to-end reconstruction with a Kehr's tube. The pathological studies of both lesions were positive for SFT metastasis (Fig. 2).
Abdominal CT: (a) cross-sectional image showing metastases in the liver and head and body of the pancreas; (b) cross-sectional image with metastasis in the liver and tail of the pancreas; (c) sagittal slice of the liver metastasis and the proximity of the metastasis in the head/body of the pancreas with the portal vein; (d and e) follow-up abdominal CT showing no evidence of recurrence or metastasis in the abdominal region.
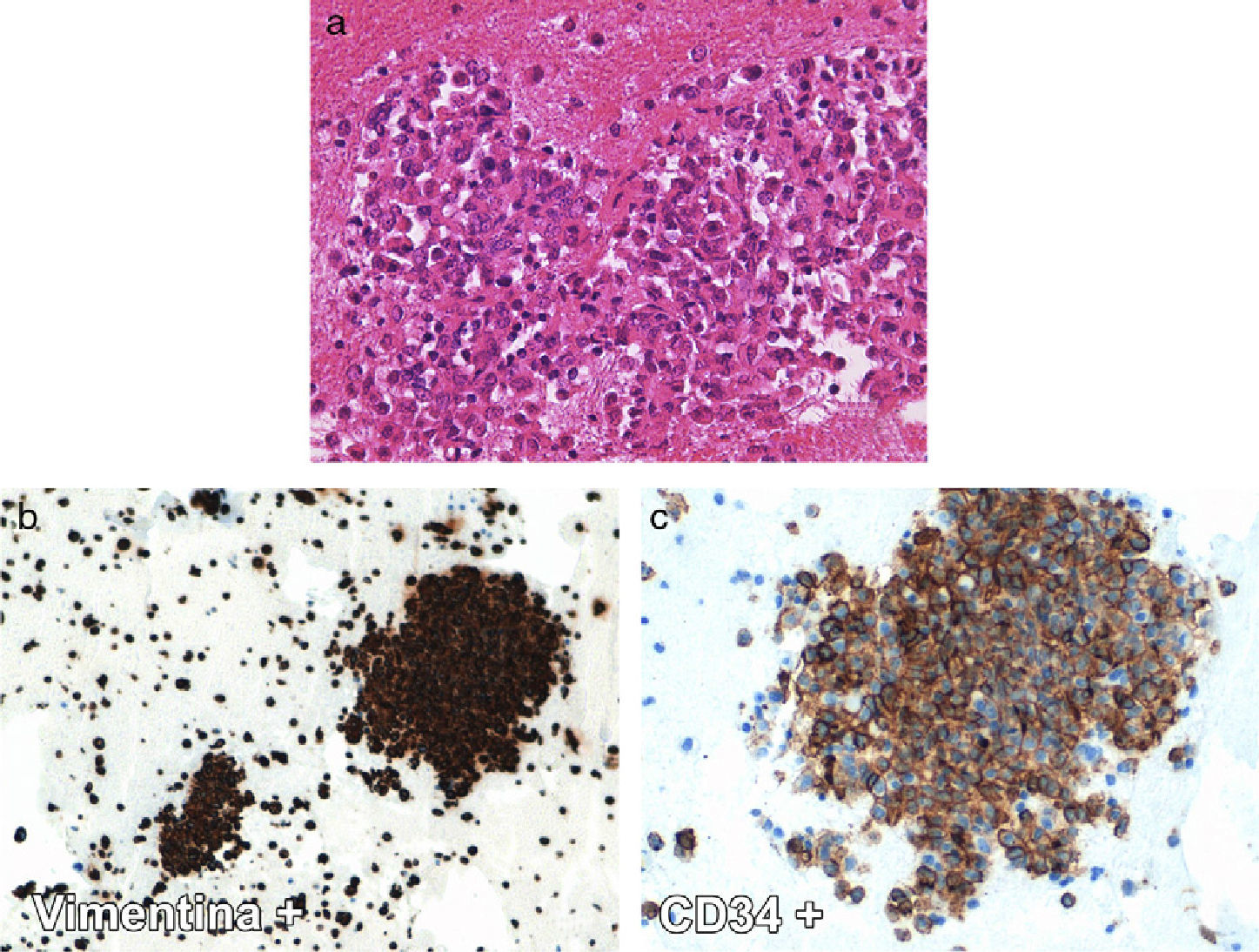
Histology images of the solitary fibrous tumor: (a) hematoxylin–eosin stain (40×) with few small, round, neoplastic cells, limited eosinophilic cytoplasm and eccentric round nuclei; (b and c) stain for immunohistochemistry study (20–40×, respectively): intense positivity of the neoplastic population for vimentin and CD34.
Postoperative complications included subhepatic and pancreaectomy bed fluid collections, which were resolved with 2 radiologically placed drainage tubes. The patient was discharged on the 29th day post-op. Fourteen months after surgery, the patient is asymptomatic, showing no evidence of either recurrence or metastasis (Fig. 1d and e).
In the literature, there are reports of less than 100 cases of SFT that affect the central nervous system.5 The diagnosis is based on immunohistochemistry tests, with very notable positivity for vimentin and CD34 (antigen originally described in hematopoietic stem cells) and negativity for epithelial membrane antigen (EMA).10 As for the biological aggressiveness of meningeal SFT, there are few reports of recurrence in Ref. 5, and complete resection of the primary tumor is described as the most important prognostic factor for a cure.5,10 Furthermore, there are two case descriptions of lung metastases appearing 10 and 25 years after the meningeal tumor presentation, respectively,6,7 and another case that, in addition to lung metastasis, debuted with spinal and hepatic metastasis 9 years after presenting the meningeal tumor.8 In our case, in addition to the local recurrence, there were metastases in the liver and pancreas. The latter location has not been previously reported in the literature.
SFT located in the liver is a rare occurrence, and we have found less than 30 cases in Ref. 3 The majority of these tumors appear as large lesions in non-cirrhotic livers with non-specific symptoms.3,4
Primary hepatic SFT are usually benign,3 although there is a case report of malignization to fibrosarcoma,4 bone metastases1,9 and local recurrence.1 The surgical resection of these tumors is the treatment of choice.
The role of chemotherapy and radiotherapy in these tumors is still controversial and is reserved for cases when resection is incomplete or there are signs of malignancy.1
There are no data about liver transplantation in patients with SFT. Nonetheless, Novais et al.3 suggest that, in some cases with unresectable liver involvement, transplantation may be indicated.
It has been argued whether aggressive surgical treatment is indicated in asymptomatic patients with advanced disease given the possible postoperative complications.3 But normally, due to the dimensions that these tumors usually reach, patients experience abdominal pain, while its malignant potential has not been well established. The risk of complications could be reduced by treating these patients in specialized Hepatobiliopancreatic Surgery Units.
In addition, SFT of the pancreas are also rare, and less than 10 cases have been published in Ref. 2 All the cases described have been located in the head or body of the pancreas, and our case is the only report of double metastasis in both the head and tail of the pancreas. Complete tumor resection (R0) is also the treatment of choice.
In conclusion, we present the first case report in the literature of a meningeal SFT with liver metastasis and 2 pancreatic metastases treated with R0 resection, due to the ineffectiveness of adjuvant therapy and the unknown malignant potential of the disease.
Please cite this article as: Febrero B, Robles R, Brusadin R, Marín C, López-Conesa A, Martínez C, et al. Metástasis hepática y pancreáticas de un tumor fibroso solitario. Cir Esp. 2014;92(6):438–441.
A video related to this case was presented at the 28th National Surgery Congress in Madrid on November 11, 2010, under the title “Pancreatectomía corporocaudal y hepatectomía central simultánea por metastasis de un tumor fibroso solitario cerebral”.