Sleeve gastrectomy (SG) has replaced gastric bypass (47% vs 35.3%) as the most commonly performed bariatric procedure worldwide.1 Despite its excellent results in terms of weight loss and resolution of comorbidities, SG is a technique associated with potentially serious complications.
The most serious complication after SG is gastric fistula, with an incidence ranging from 0.5% to 5.3% of cases,2 although the related mortality rate can reach 9%.
Although several strategies have been described for dealing with this complication, the therapeutic algorithm has not yet been standardized.3
Except for situations in which the fistula presents with signs of sepsis and/or hemodynamic instability requiring urgent reoperation, the conservative therapeutic option is reasonable, combining parenteral nutrition, broad-spectrum antibiotics, and percutaneous drainage of collections.4,5
As an alternative to this conservative treatment, the placement of a nasogastric tube allows for outpatient management with enteral nutrition until the resolution of the fistula.
With the development of endoscopic techniques, several alternatives have been arisen for the treatment of fistulae. Self-expanding stents have been used with variable success rates higher than 50%, although there is also a high rate of migration (47%), ulcers (41%), and patient discomfort. Other options include clips to close the fistula orifice (Over-the-Scope-Clip [OTSC®]), stricturotomies of the fistula septum, application of adhesives, and placement of a pigtail catheter or Endo-SPONGE®.6–9 However, the great heterogeneity of treatments means that there is no consensus on the strategy to be followed with these patients.
The time of evolution from surgery to diagnosis is a key factor in estimating the possible success of conservative treatment. Thus, patients with fistulae that have not been resolved after more than 30 days or fistulae that have become chronic 12 weeks after surgery do not have a very favorable response to endoscopic treatments and require surgical treatment in most cases.10
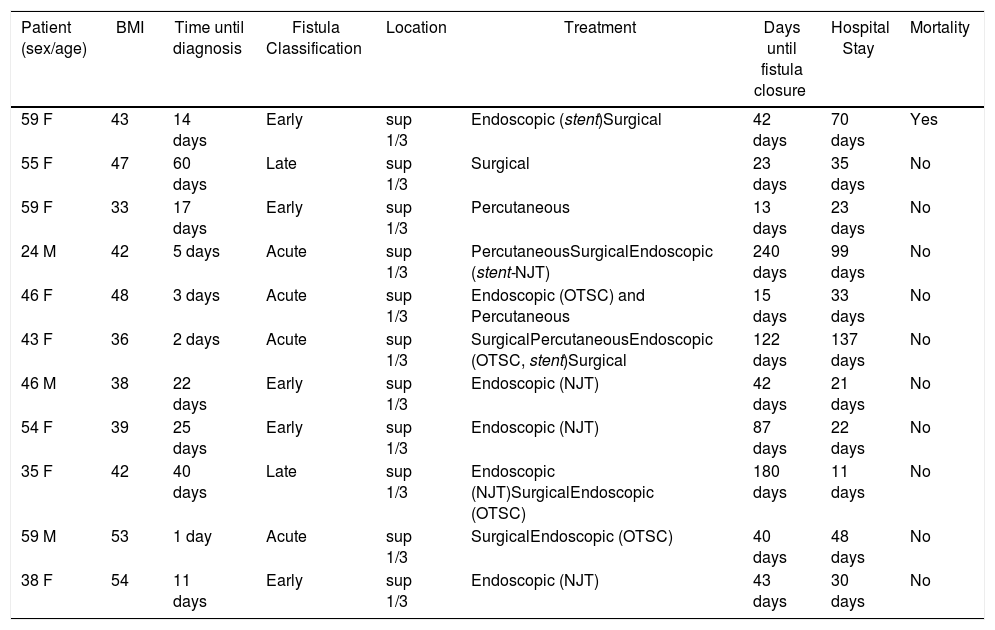
The aim of this study was to analyze the incidence and management of post-SG gastric fistulae in our group. We conducted a retrospective study of 11 patients diagnosed and treated for post-SG fistula between January 2010 and September 2019. After 498 SG, the incidence of gastric fistula was 2.2%.
Mean age was 46 years (range: 38–59 years), and there were 8 women and 3 men. Preoperative mean BMI was 42kg/m2 (range: 38–48kg/m2), and 55% of the patients had comorbidities: diabetes, arterial hypertension, dyslipidemia, and apnea–hypopnea syndrome, while 36% were active smokers. Two patients had a history of adjustable gastric band removal prior to SG.
In all patients except one, SG was performed laparoscopically, and the staple line was reinforced in 10 (9 Peristrip Dry® and 1 Seamguard®). In 3 of the 11 patients, the fistula was diagnosed during hospitalization, while 8 were readmitted due to related symptoms. The time elapsed between the procedure and the diagnosis was 14 days (range: 3–25 days). In all patients, the diagnosis was by computed tomography.
Out of the 8 patients who underwent nonsurgical treatment (endoscopic or percutaneous), the fistula resolved in 5 (62.5%). The 3 patients refractory to conservative treatment required surgical intervention.
Despite the increasing use of stents in the literature for the treatment of this complication, in our experience with the 3 patients in which they were used, we did not obtain good results. All of the stents migrated and one eroded the aorta, requiring reoperation, although the patient ultimately died (mortality: 9%). In contrast, we have had good results with the combined placement of a nasojejunal tube for enteral nutrition and the application of OTSC® in the fistula orifice. Despite limited experience (4 cases), we have achieved a 75% success rate.
In the remaining 3 patients, surgical management was chosen due to their hemodynamic instability. The approach was laparoscopic in one case and open in 2. In 2 cases, the collection was drained, while in the other the fistula was closed and the tube removed. The success rate was 33%, with subsequent endoscopic procedures for the resolution of the fistula (Table 1).
Therapeutic Management of Post-SG Gastric Fistula.
| Patient (sex/age) | BMI | Time until diagnosis | Fistula Classification | Location | Treatment | Days until fistula closure | Hospital Stay | Mortality |
|---|---|---|---|---|---|---|---|---|
| 59 F | 43 | 14 days | Early | sup 1/3 | Endoscopic (stent)Surgical | 42 days | 70 days | Yes |
| 55 F | 47 | 60 days | Late | sup 1/3 | Surgical | 23 days | 35 days | No |
| 59 F | 33 | 17 days | Early | sup 1/3 | Percutaneous | 13 days | 23 days | No |
| 24 M | 42 | 5 days | Acute | sup 1/3 | PercutaneousSurgicalEndoscopic (stent-NJT) | 240 days | 99 days | No |
| 46 F | 48 | 3 days | Acute | sup 1/3 | Endoscopic (OTSC) and Percutaneous | 15 days | 33 days | No |
| 43 F | 36 | 2 days | Acute | sup 1/3 | SurgicalPercutaneousEndoscopic (OTSC, stent)Surgical | 122 days | 137 days | No |
| 46 M | 38 | 22 days | Early | sup 1/3 | Endoscopic (NJT) | 42 days | 21 days | No |
| 54 F | 39 | 25 days | Early | sup 1/3 | Endoscopic (NJT) | 87 days | 22 days | No |
| 35 F | 42 | 40 days | Late | sup 1/3 | Endoscopic (NJT)SurgicalEndoscopic (OTSC) | 180 days | 11 days | No |
| 59 M | 53 | 1 day | Acute | sup 1/3 | SurgicalEndoscopic (OTSC) | 40 days | 48 days | No |
| 38 F | 54 | 11 days | Early | sup 1/3 | Endoscopic (NJT) | 43 days | 30 days | No |
SG: sleeve gastrectomy; BMI: body mass index; F: female; M: male; OTSC®: Over-the-Scope-Clip; NJT: nasojejunal tube; sup: superior.
Fistula classification: Acute ≤7 days; Early 1–6 weeks; Late 7–12 weeks.
The treatment column shows the different types of treatment that the patient has undergone, in their order of appearance.
In 2 patients (20%) with chronic fistula that had undergone other treatments, total gastrectomy was decisive in both cases.
The mean time to resolution of the fistula after diagnosis was 42 days (range: 23–122 days), and the mean postoperative stay was 33 days (range: 22–70 days).
In conclusion, the management of post-SG gastric fistula is not completely standardized. In our experience, conservative management has been successful in 62.5% of patients, and the current treatment of choice at our hospital is the placement of a nasojejunal tube for enteral nutrition, combined with the application of OTSC® in select cases. We do not have much experience in the use of stents, but neither have we had good results with their placement due to migration, ulceration and the need for additional treatments.
Please cite this article as: Vilar A, Priego P, Cuadrado M, Arranz R, Galindo J. Manejo de la fistula gástrica tras gastrectomía vertical. Cir Esp. 2020;98:639–640.